Sackett DL, Rosenberg WM, Gray JA, et al. Evidence based medicine: what it is and what it isn't. BMJ. 1996;312(7023):71-72. doi:10.1136/bmj.312.7023.71.
Федеральный закон от 21.11.2011 № 323-ФЗ (ред. от 03.04.2017) «Об основах охраны здоровья граждан в Российской Федерации».
Эпидемиологический словарь, 4-е издание. Под ред. Джона М. Ласта для Международной эпидемиологической ассоциации. М., 2009. 316 с.
Федеральное агентство по техническому регулированию и метрологии. Национальный стандарт Российской Федерации. ГОСТР 52379-2005. Надлежащая клиническая практика. Москва, 2005.
Федеральный закон от 12.04.2010 № 61-ФЗ (ред. от 03.07.2016) «Об обращении лекарственных средств».
Малая медицинская энциклопедия. М.: Медицинская энциклопедия, 1991—96 гг. [Электронный ресурс]. Режим доступа: http://dic.academic.ru/dic.nsf/enc_medicine/28878/Синдром
Андреева НС, Реброва ОЮ, Зорин НА и др. Системы оценки достоверности научных доказательств и убедительности рекомендаций: сравнительная характеристика и перспективы унификации. Медицинские технологии. Оценка и выбор. 2012;4(10):10–24.
Насонов ЕЛ, Елисеев МС. Роль интерлейкина 1 в развитии заболеваний человека. Научно-практическая ревматология. 2016;54(1):60-77. doi: 10.14412/1995-4484-2016-60-77.
Martillo MA, Nazzal L, Crittenden DB. The crystallization of monosodium urate. Curr Rheumatol Rep. 2014;16(2):400. doi:10.1007/s11926-013-0400-9.
Loeb JN. The influence of temperature on the solubility of monosodium urate. Arthritis Rheum. 1972;15(2):189-192. doi:10.1002/art.1780150209.
Dalbeth N, Phipps-Green A, Frampton C, et al. Relationship between serum urate concentration and clinically evident incident gout: an individual participant data analysis. Ann Rheum Dis. 2018;77(7):1048-1052.
Dalbeth N, House ME, Aati O, et al. Urate crystal deposition in asymptomatic hyperuricaemia and symptomatic gout: a dual energy CT study. Ann Rheum Dis. 2015;74(5):908-911. doi:10.1136/annrheumdis-2014-206397.
Campion EW, Glynn RJ, DeLabry LO. Asymptomatic hyperuricemia. Risks and consequences in the Normative Aging Study. Am J Med. 1987;82(3):421-426. doi:10.1016/0002-9343(87)90441-4.
Chen-Xu M, Yokose C, Rai SK, et al. Contemporary Prevalence of Gout and Hyperuricemia in the United States and Decadal Trends: The National Health and Nutrition Examination Survey, 2007-2016. Arthritis Rheumatol. 2019;71(6):991-999. doi:10.1002/art.40807.
Sumino H, Ichikawa S, Kanda T, et al. Reduction of serum uric acid by hormone replacement therapy in postmenopausal women with hyperuricaemia. Lancet. 1999;354(9179):650. doi:10.1016/S0140-6736(99)92381-4.
Boocock J, Leask M, Okada Y, et al. Genomic dissection of 43 serum urate-associated loci provides multiple insights into molecular mechanisms of urate control. Hum Mol Genet. 2020;29(6):923-943. doi:10.1093/hmg/ddaa013.
Tin A, Marten J, Halperin Kuhns VL, et al. Target genes, variants, tissues and transcriptional pathways influencing human serum urate levels. Nat Genet. 2019;51(10):1459-1474. doi:10.1038/s41588-019-0504-x.
Choi HK, Curhan G. Soft. Beer, liquor, and wine consumption and serum uric acid level: the Third National Health and Nutrition Examination Survey. Arthritis Rheum. 2004;51(6):1023-1029. doi:10.1002/art.20821.
Choi HK, Atkinson K, Karlson EW, et al. Purine-rich foods, dairy and protein intake, and the risk of gout in men. N Engl J Med. 2004;350(11):1093-1103. doi:10.1056/NEJMoa035700.
Choi HK, Willett W, Curhan G. Fructose-rich beverages and risk of gout in women. JAMA. 2010;304(20):2270-2278. doi:10.1001/jama.2010.1638.
McAdams DeMarco MA, Maynard JW, Baer AN, et al. Diuretic use, increased serum urate levels, and risk of incident gout in a population-based study of adults with hypertension: the Atherosclerosis Risk in Communities cohort study. Arthritis Rheum. 2012;64(1):121-129. doi:10.1002/art.33315.
Mikuls TR, Farrar JT, Bilker WB, et al. Gout epidemiology: results from the UK General Practice Research Database, 1990-1999. Ann Rheum Dis. 2005;64(2):267-272. doi:10.1136/ard.2004.024091.
Cohen SD, Kimmel PL, Neff R, et al. Association of incident gout and mortality in dialysis patients. J Am Soc Nephrol. 2008;19(11):2204-2210. doi:10.1681/ASN.2007111256.
Galozzi P, Bindoli S, Doria A, et al. Autoinflammatory Features in Gouty Arthritis. J Clin Med. 2021;10(9):1880. Published 2021 Apr 26. doi:10.3390/jcm10091880.
Choi HK, Mount DB, Reginato AM; American College of Physicians; American Physiological Society. Pathogenesis of gout. Ann Intern Med. 2005;143(7):499-516. doi:10.7326/0003-4819-143-7-200510040-00009.
Dehlin M, Jacobsson L, Roddy E. Global epidemiology of gout: prevalence, incidence, treatment patterns and risk factors. Nat Rev Rheumatol. 2020;16(7):380-390. doi:10.1038/s41584-020-0441-1.
Safiri S, Kolahi AA, Cross M, et al. Prevalence, Incidence, and Years Lived With Disability Due to Gout and Its Attributable Risk Factors for 195 Countries and Territories 1990-2017: A Systematic Analysis of the Global Burden of Disease Study 2017. Arthritis Rheumatol. 2020;72(11):1916-1927. doi:10.1002/art.41404.
GBD 2017 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017 [published correction appears in Lancet. 2019 Jun 22;393(10190):e44]. Lancet. 2018;392(10159):1859-1922. doi:10.1016/S0140-6736(18)32335-3.
Choi HK, Curhan G. Independent impact of gout on mortality and risk for coronary heart disease. Circulation. 2007;116(8):894-900. doi:10.1161/CIRCULATIONAHA.107.703389.
Vargas-Santos AB, Neogi T, da Rocha Castelar-Pinheiro G, et al. Cause-Specific Mortality in Gout: Novel Findings of Elevated Risk of Non-Cardiovascular-Related Deaths. Arthritis Rheumatol. 2019;71(11):1935-1942. doi:10.1002/art.41008.
Fisher MC, Rai SK, Lu N, et al. The unclosing premature mortality gap in gout: a general population-based study. Ann Rheum Dis. 2017;76(7):1289-1294. doi:10.1136/annrheumdis-2016-210588.
Danve A, Neogi T. Rising Global Burden of Gout: Time to Act. Arthritis Rheumatol. 2020;72(11):1786-1788. doi:10.1002/art.41453.
Черёмушкина ЕВ, Елисеев МС. Гиперурикемия и подагра: влияние на костный метаболизм и суставной хрящ (обзор литературы). Ожирение и метаболизм. 2022;19(3):348-357. doi:10.14341/omet12894.
Zhang W, Doherty M, Pascual E, et al. EULAR evidence based recommendations for gout. Part I: Diagnosis. Report of a task force of the Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis. 2006;65(10):1301-1311. doi:10.1136/ard.2006.055251.
Sivera F, Andrés M, Carmona L, et al. Multinational evidence-based recommendations for the diagnosis and management of gout: integrating systematic literature review and expert opinion of a broad panel of rheumatologists in the 3e initiative. Ann Rheum Dis. 2014;73(2):328-335. doi:10.1136/annrheumdis-2013-203325.
Kuo CF, Grainge MJ, Zhang W, Doherty M. Global epidemiology of gout: prevalence, incidence and risk factors. Nat Rev Rheumatol. 2015;11(11):649-662. doi:10.1038/nrrheum.2015.91.
Lioté F, Lancrenon S, Lanz S, et al. GOSPEL: prospective survey of gout in France. Part I: design and patient characteristics (n = 1003). Joint Bone Spine. 2012;79(5):464-470. doi:10.1016/j.jbspin.2011.12.006.
Елисеев МС, Денисов ИС, Маркелова ЕИ, и др. Независимые факторы риска развития тяжелых сердечно-сосудистых осложнений у мужчин с подагрой: результаты 7-летнего проспективного исследования. Терапевтический архив. 2017;89(5):10-19. doi: 10.17116/terarkh201789510-19.
Fatima T, Nilsson PM, Turesson C, et al. The absolute risk of gout by clusters of gout-associated comorbidities and lifestyle factors-30 years follow-up of the Malmö Preventive Project. Arthritis Res Ther. 2020;22(1):244. doi:10.1186/s13075-020-02339-0.
Evans PL, Prior JA, Belcher J, et al. Obesity, hypertension and diuretic use as risk factors for incident gout: a systematic review and meta-analysis of cohort studies. Arthritis Res Ther. 2018;20(1):136. doi:10.1186/s13075-018-1612-1.
Krishnan E. Chronic kidney disease and the risk of incident gout among middle-aged men: a seven-year prospective observational study. Arthritis Rheum. 2013;65(12):3271-3278. doi:10.1002/art.38171.
Hsu CY, Iribarren C, McCulloch CE, et al. Risk factors for end-stage renal disease: 25-year follow-up. Arch Intern Med. 2009;169(4):342-350. doi:10.1001/archinternmed.2008.605.
Ma LD, Sun RX, Xin Y, et al. [Clinical characteristics in gout patients with different body mass index]. Zhonghua Nei Ke Za Zhi. 2017 May 1;56(5):353-357. Chinese. doi: 10.3760/cma.j.issn.0578-1426.2017.05.010.
Richette P, Doherty M, Pascual E, et al. 2018 updated European League Against Rheumatism evidence-based recommendations for the diagnosis of gout. Ann Rheum Dis. 2020;79(1):31-38. doi:10.1136/annrheumdis-2019-215315.
Jamnik J, Rehman S, Blanco Mejia S, et al. Fructose intake and risk of gout and hyperuricemia: a systematic review and meta-analysis of prospective cohort studies. BMJ Open. 2016;6(10):e013191. doi:10.1136/bmjopen-2016-013191.
Chi X, Cen Y, Yang B, et al. Effects of dietary factors on hyperuricaemia and gout: a systematic review and meta-analysis of observational studies. Int J Food Sci Nutr. 2024;75(8):753-773. doi:10.1080/09637486.2024.2400489.
Choi HK, Curhan G. Soft drinks, fructose consumption, and the risk of gout in men: prospective cohort study. BMJ. 2008;336(7639):309-312. doi:10.1136/bmj.39449.819271.BE.
McCormick N, Rai SK, Lu N, et al. Estimation of Primary Prevention of Gout in Men Through Modification of Obesity and Other Key Lifestyle Factors. JAMA Netw Open. 2020;3(11):e2027421. Published 2020 Nov 2. doi:10.1001/jamanetworkopen.2020.27421.
Choi HK, Atkinson K, Karlson EW, et al. Alcohol intake and risk of incident gout in men: a prospective study. Lancet. 2004;363(9417):1277-1281. doi:10.1016/S0140-6736(04)16000-5.
Gao X, Qi L, Qiao N, et al. Intake of added sugar and sugar-sweetened drink and serum uric acid concentration in US men and women. Hypertension. 2007;50(2):306-312. doi:10.1161/HYPERTENSIONAHA.107.091041.
Choi HK, Willett W, Curhan G. Fructose-rich beverages and risk of gout in women. JAMA. 2010;304(20):2270-2278. doi:10.1001/jama.2010.1638.
Topless RKG, Major TJ, Florez JC, et al. The comparative effect of exposure to various risk factors on the risk of hyperuricaemia: diet has a weak causal effect. Arthritis Res Ther. 2021;23(1):75. doi:10.1186/s13075-021-02444-8.
Narang RK, Gamble G, Phipps-Green AJ, et al. Do Serum Urate-associated Genetic Variants Influence Gout Risk in People Taking Diuretics? Analysis of the UK Biobank. J Rheumatol. 2020;47(11):1704-1711. doi:10.3899/jrheum.191005.
Vedder D, Walrabenstein W, Heslinga M, et al. Dietary Interventions for Gout and Effect on Cardiovascular Risk Factors: A Systematic Review. Nutrients. 2019;11(12):2955. doi:10.3390/nu11122955.
Araújo F, Cordeiro I, Teixeira F, et al. Portuguese recommendations for the diagnosis and management of gout. Acta Reumatol Port. 2014;39(2):158-171.
Choi HK, Soriano LC, Zhang Y, Rodríguez LA. Antihypertensive drugs and risk of incident gout among patients with hypertension: population based case-control study. BMJ. 2012;344:d8190. doi:10.1136/bmj.d8190.
Burack DA, Griffith BP, Thompson ME, Kahl LE. Hyperuricemia and gout among heart transplant recipients receiving cyclosporine. Am J Med. 1992;92(2):141-146. doi:10.1016/0002-9343(92)90104-j.
Shapiro M, Hyde L. Hyperuricemia due to pyrazinamide. Am J Med. 1957;23(4):596-599. doi:10.1016/0002-9343(57)90230-9.
Narang RK, Agarwal MC, Raina AK, et al. Hyperuricaemia induced by ethambutol. Br J Dis Chest. 1983;77(4):403-406.
Caspi D, Lubart E, Graff E, et al. The effect of mini-dose aspirin on renal function and uric acid handling in elderly patients. Arthritis Rheum. 2000;43(1):103-108.
Wallace SL, Robinson H, Masi AT, et al. Preliminary criteria for the classification of the acute arthritis of primary gout. Arthritis Rheum. 1977;20(3):895-900. doi:10.1002/art.1780200320.
Neogi T, Jansen TL, Dalbeth N, et al. 2015 Gout classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative [published correction appears in Ann Rheum Dis. 2016 Feb;75(2):473]. Ann Rheum Dis. 2015;74(10):1789-1798. doi:10.1136/annrheumdis-2015-208237.
Елисеев МС, Владимиров СА. Распространенность и клинические особенности подагры и болезни депонирования пирофосфата кальция у пациентов с острым артритом. Научно-практическая ревматология. 2015;53(4):375-378. doi:10.14412/1995-4484-2015-375-378.
Stewart S, Dalbeth N, Vandal AC, Rome K. The first metatarsophalangeal joint in gout: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2016 Feb 11;17:69. doi: 10.1186/s12891-016-0919-9.
Taylor WJ, Fransen J, Jansen TL, et al. Study for Updated Gout Classification Criteria: Identification of Features to Classify Gout. Arthritis Care Res (Hoboken). 2015;67(9):1304-1315. doi:10.1002/acr.22585.
Барскова ВГ. Рациональные подходы к диагностике подагры (по материалам рекомендаций европейской антиревматической лиги). Современная ревматология. 2007;1(1):10-12.
Perez-Ruiz F, Castillo E, Chinchilla SP, Herrero-Beites AM. Clinical manifestations and diagnosis of gout. Rheum Dis Clin North Am. 2014;40(2):193-206. doi:10.1016/j.rdc.2014.01.003.
Janssens HJ, Janssen M, van de Lisdonk EH, et al. Limited validity of the American College of Rheumatology criteria for classifying patients with gout in primary care. Ann Rheum Dis. 2010;69(6):1255-1256. doi:10.1136/ard.2009.123687.
Juraschek SP, Miller ER 3rd, Gelber AC. Body mass index, obesity, and prevalent gout in the United States in 1988-1994 and 2007-2010. Arthritis Care Res (Hoboken). 2013;65(1):127-132. doi:10.1002/acr.21791.
Combe B, Landewe R, Daien CI, et al. 2016 update of the EULAR recommendations for the management of early arthritis. Ann Rheum Dis. 2017;76(6):948-959. doi:10.1136/annrheumdis-2016-210602.
Российские клинические рекомендации. Ревматология. Под ред. Е.Л. Насонова. М.:ГЭОТАР-Медиа, 2017; 253-264.
Malik A, Schumacher HR, Dinnella JE, Clayburne GM. Clinical diagnostic criteria for gout: comparison with the gold standard of synovial fluid crystal analysis. J Clin Rheumatol. 2009 Feb;15(1):22-4. doi:10.1097/RHU.0b013e3181945b79.
Pascual E, Doherty M. Aspiration of normal or asymptomatic pathological joints for diagnosis and research: indications, technique and success rate. Ann Rheum Dis. 2009;68(1):3-7. doi:10.1136/ard.2008.088328.
Pascual E, Sivera F. Time required for disappearance of urate crystals from synovial fluid after successful hypouricaemic treatment relates to the duration of gout. Ann Rheum Dis. 2007;66(8):1056-1058. doi:10.1136/ard.2006.060368.
Taylor WJ, Fransen J, Dalbeth N, et al. Diagnostic Arthrocentesis for Suspicion of Gout Is Safe and Well Tolerated. J Rheumatol. 2016;43(1):150-153. doi:10.3899/jrheum.150684.
Parker JD, Capell HA. An acute arthritis clinic--one year's experience. Br J Rheumatol. 1986;25(3):293-295. doi:10.1093/rheumatology/25.3.293.
Freed JF, Nies KM, Boyer RS, Louie JS. Acute monoarticular arthritis. A diagnostic approach. JAMA. 1980;243(22):2314-2316.
Shmerling RH, Delbanco TL, Tosteson AN, Trentham DE. Synovial fluid tests. What should be ordered? JAMA. 1990;264(8):1009-1014.
Jeng GW, Wang CR, Liu ST, et al. Measurement of synovial tumor necrosis factor-alpha in diagnosing emergency patients with bacterial arthritis. Am J Emerg Med. 1997;15(7):626-629. doi:10.1016/s0735-6757(97)90173-x.
Maki DG. Risk for septic arthritis was increased in adults with incident diagnosis of gout. Ann Intern Med. 2015;163(12):JC12. doi:10.7326/ACPJC-2015-163-12-012.
Yu KH, Luo SF, Liou LB, et al. Concomitant septic and gouty arthritis--an analysis of 30 cases. Rheumatology (Oxford). 2003;42(9):1062-1066. doi:10.1093/rheumatology/keg297
Richette P, Doherty M, Pascual E, et al. 2016 updated EULAR evidence-based recommendations for the management of gout. Ann Rheum Dis. 2017;76(1):29-42. doi:10.1136/annrheumdis-2016-209707.
Bhole V, de Vera M, Rahman MM, Krishnan E, Choi H. Epidemiology of gout in women: Fifty-two-year followup of a prospective cohort. Arthritis Rheum. 2010;62(4):1069-1076. doi:10.1002/art.27338.
Lin KC, Lin HY, Chou P. The interaction between uric acid level and other risk factors on the development of gout among asymptomatic hyperuricemic men in a prospective study. J Rheumatol. 2000;27(6):1501-1505.
Neilson J, Bonnon A, Dickson A, Roddy E; Guideline Committee. Gout: diagnosis and management-summary of NICE guidance. BMJ. 2022;378:o1754. doi:10.1136/bmj.o1754.
Lu J, Zhang Q, Yang G, Gu Z, Wu Y. Analysis of Superb Microvascular Imaging Blood Flow Scoring, Disease Duration, and Laboratory Indicators Involved in Gout. J Clin Ultrasound. doi:10.1002/jcu.23940.
Jiang Y, Tu X, Liao X, et al. New Inflammatory Marker Associated with Disease Activity in Gouty Arthritis: The Systemic Inflammatory Response Index. J Inflamm Res. 2023;16:5565-5573. doi:10.2147/JIR.S432898.
Bardin T, Richette P. Impact of comorbidities on gout and hyperuricaemia: an update on prevalence and treatment options. BMC Med. 2017;15(1):123. Published 2017 Jul 3. doi:10.1186/s12916-017-0890-9.
San Gabriel DED, Slark J. The association of gout with an increased risk of hypertension and diabetes mellitus among stroke survivors in New Zealand: A cross-sectional study using routinely collected electronic health data. JRSM Cardiovasc Dis. 2019;8:2048004019863239. Published 2019 Jul 19. doi:10.1177/2048004019863239.
Российская ассоциация эндокринологов. Клинические рекомендации. Сахарный диабет 2 типа у взрослых. 2022.
Li L, Lip GYH, Li S, Adachi JD, Thabane L, Li G. Associations between glycated hemoglobin and the risks of incident cardiovascular diseases in patients with gout. Cardiovasc Diabetol. 2022;21(1):133. Published 2022 Jul 15. doi:10.1186/s12933-022-01567-9.
Fhima F, El Amri N, Khalifa D, et al. AB1069. Uric Acid Levels In Relation To Fasting Blood Glucose And HbA1c. Annals of the Rheumatic Diseases 2022;81:1654.
Lai HM, Chen CJ, Su BY, et al. Gout and type 2 diabetes have a mutual inter-dependent effect on genetic risk factors and higher incidences. Rheumatology (Oxford). 2012;51(4):715-720. doi:10.1093/rheumatology/ker373.
Елисеев МС, Барскова В.Г. Нарушения углеводного обмена при подагре: частота выявления и клинические особенности. Терапевтический архив. 2010; 82(5):50-54.
Richette P, Clerson P, Périssin L, et al. Revisiting comorbidities in gout: a cluster analysis. Ann Rheum Dis. 2015;74(1):142-147. doi:10.1136/annrheumdis-2013-203779.
Дедов ИИ, Шестакова МВ, Майорова АЮ, и др. Алгоритмы специализированной медицинской помощи больным сахарным диабетом. 9-й выпуск.2019.
Johnson RJ, Titte S, Cade JR, et al. Uric acid, evolution and primitive cultures. Semin Nephrol. 2005;25(1):3-8. doi:10.1016/j.semnephrol.2004.09.002.
Li HN, Liu J, Shao Z, Xiong W, Cheng L. Gouty arthritis patients' diagnostic, biochemical, and hematological characteristics study: a single-center retrospective study. BMC Musculoskelet Disord. 2024;25(1):1054. doi:10.1186/s12891-024-08151-0.
Han L, Zhang L, Hu W, Lu Y, Wang Z. Association of C-reactive protein with all-cause and cause-specific mortality in people with gout. Eur J Med Res. 2024;29(1):320. doi:10.1186/s40001-024-01923-3.
Schlesinger N, Alten RE, Bardin T, Schumacher HR, Bloch M, Gimona A, Krammer G, Murphy V, Richard D, So AK. Canakinumab for acute gouty arthritis in patients with limited treatment options: results from two randomised, multicentre, active-controlled, double-blind trials and their initial extensions. Ann Rheum Dis. 2012 Nov;71(11):1839-48. Doi: 10.1136/annrheumdis-2011-200908. Epub 2012 May 14. PMID: 22586173.
De Cosmo S, Viazzi F, Pacilli A, et al. Serum Uric Acid and Risk of CKD in Type 2 Diabetes. Clin J Am Soc Nephrol. 2015;10(11):1921-1929. doi:10.2215/CJN.03140315.
Jaffe DH, Klein AB, Benis A, et al. Incident gout and chronic Kidney Disease: healthcare utilization and survival. BMC Rheumatol. 2019;3:11. Published 2019 Mar 19. doi:10.1186/s41927-019-0060-0.
Елисеев МС. Гиперурикемия как фактор поражения почек и мишень терапии. Эффективная фармакотерапия. 2020;16(6):30-35. doi: 10.33978/2307-3586-2020-16-6-30-35.
Roughley MJ, Belcher J, Mallen CD, Roddy E. Gout and risk of chronic kidney disease and nephrolithiasis: meta-analysis of observational studies. Arthritis Res Ther. 2015;17(1):90. Published 2015 Apr 1. doi:10.1186/s13075-015-0610-9.
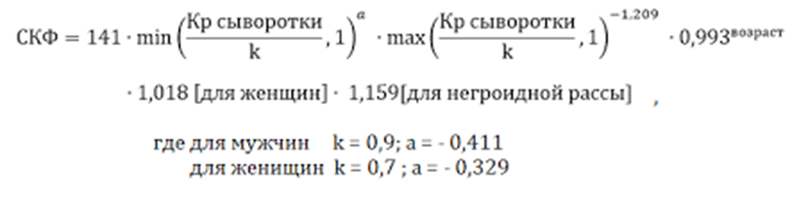
Ahmed S, Subash T, Ahmed H, Sadiqa A, Yaqub S, Jafri L. Diagnostic Accuracy of Creatinine-Based Equations for eGFR Estimation in Pakistanis: Evaluation of the European Kidney Function Consortium Equation vs the CKD-EPI Pakistan Equation. EJIFCC. 2024;35(4):285-293.
Gharipour M, Sadeghi M, Nezafati P, Dianatkhah M, Sarrafzadegan N. Cardiovascular Disease Risk Assessment: Triglyceride/High-Density Lipoprotein versus Metabolic Syndrome Criteria. J Res Health Sci. 2019 May 13;19(2):e00442.
Kuwabara M, Borghi C, Cicero AFG, et al. Elevated serum uric acid increases risks for developing high LDL cholesterol and hypertriglyceridemia: A five-year cohort study in Japan. Int J Cardiol. 2018;261:183-188. doi:10.1016/j.ijcard.2018.03.045.
Russo E, Viazzi F, Pontremoli R, et al. Association of uric acid with kidney function and albuminuria: the Uric Acid Right for heArt Health (URRAH) Project [published online ahead of print, 2021 Mar 23]. J Nephrol. 2021;10.1007/s40620-021-00985-4. doi:10.1007/s40620-021-00985-4.
Su X, Xu B, Yan B, et al. Effects of uric acid-lowering therapy in patients with chronic kidney disease: A meta-analysis. PLoS One. 2017;12(11):e0187550. Published 2017 Nov 2. doi:10.1371/journal.pone.0187550.
Канакинумаб (Иларис®). Государственный реестр лекарственных средств. https://grls.minzdrav.gov.ru/Grls_View_v2.aspx?routingGuid=011c2bd7-a3f5-4750-80ef-52c6cf58051b (дата обращения 04.05.2024).
Ortiz-Brizuela E, Apriani L, Mukherjee T, et al. Assessing the Diagnostic Performance of New Commercial Interferon-γ Release Assays for Mycobacterium tuberculosis Infection: A Systematic Review and Meta-Analysis. Clin Infect Dis. 2023;76(11):1989-1999. doi:10.1093/cid/ciad030.
Zhou G, Luo Q, Luo S, et al. Interferon-γ release assays or tuberculin skin test for detection and management of latent tuberculosis infection: a systematic review and meta-analysis. Lancet Infect Dis. 2020;20(12):1457-1469. doi:10.1016/S1473-3099(20)30276-0.
Mrozek N, Pereira B, Soubrier M, Gourdon F, Laurichesse H. Screening of tuberculosis before biologics. Med Mal Infect. 2012;42(1):1-4. doi:10.1016/j.medmal.2011.08.002.
Avena-Woods C, Hilas O. Febuxostat (Uloric), A New Treatment Option for Gout. P T. 2010 Feb;35(2):82–5.
Hoeltzenbein M, Stieler K, Panse M, et al. Allopurinol Use during Pregnancy - Outcome of 31 Prospectively Ascertained Cases and a Phenotype Possibly Indicative for Teratogenicity. PLoS One. 2013;8(6):e66637. doi:10.1371/journal.pone.0066637.
Kozenko M, Grynspan D, Oluyomi-Obi T, Sitar D, Elliott AM, Chodirker BN. Potential teratogenic effects of allopurinol: a case report. Am J Med Genet A. 2011;155A(9):2247-2252. doi:10.1002/ajmg.a.34139.
Patel AV, Gaffo AL. Managing Gout in Women: Current Perspectives. J Inflamm Res. 2022;15:1591-1598. Published 2022 Mar 3. doi:10.2147/JIR.S284759.
Mathieu S, Pereira B, Couderc M, Soubrier M. Usefulness of ultrasonography in the diagnosis of gout: a meta-analysis. Ann Rheum Dis. 2013;72(10):e23. doi:10.1136/annrheumdis-2013-204108.
Lee YH, Song GG. Diagnostic accuracy of ultrasound in patients with gout: A meta-analysis. Semin Arthritis Rheum. 2018;47(5):703-709. doi:10.1016/j.semarthrit.2017.09.012.
Ogdie A, Taylor WJ, Neogi T, et al. Performance of Ultrasound in the Diagnosis of Gout in a Multicenter Study: Comparison With Monosodium Urate Monohydrate Crystal Analysis as the Gold Standard. Arthritis Rheumatol. 2017;69(2):429-438. doi:10.1002/art.39959.
Якунина ИА, Ильиных ЕВ, Удельнова ИА и др. Частота выявления симптома «пробойника» при рентгенологическом исследовании дистальных отделов стоп больных с подагрой: связь с длительностью болезни и течением артрита. Научно-практическая ревматология. 2003;2:222-231.
Hoff LS, Goldenstein-Schainberg C, Fuller R. Nephrolithiasis in gout: prevalence and characteristics of Brazilian patients. Adv Rheumatol. 2019;60(1):2. Published 2019 Dec 31. doi:10.1186/s42358-019-0106-4.
Alvarez-Nemegyei J, Medina-Escobedo M, Villanueva-Jorge S, Vazquez-Mellado J. Prevalence and risk factors for urolithiasis in primary gout: is a reappraisal needed?. J Rheumatol. 2005;32(11):2189-2191.
Kramer HJ, Choi HK, Atkinson K, et al. The association between gout and nephrolithiasis in men: The Health Professionals' Follow-Up Study. Kidney Int. 2003;64(3):1022-1026. doi:10.1046/j.1523-1755.2003.t01-2-00171.x.
Wyngaarden J.B., Kelley W.N. Gout and hyperuricemia. 1976:233-252.
Shang J, Zhou LP, Wang H, Liu B. Diagnostic Performance of Dual-energy CT Versus Ultrasonography in Gout: A Meta-analysis. Acad Radiol. 2022 Jan;29(1):56-68. doi: 10.1016/j.acra.2020.08.030.
Gamala M, Jacobs JWG, van Laar JM. The diagnostic performance of dual energy CT for diagnosing gout: a systematic literature review and meta-analysis. Rheumatology (Oxford). 2019;58(12):2117-2121. doi:10.1093/rheumatology/kez180.
Chen J, Liao M, Zhang H, Zhu D. Diagnostic accuracy of dual-energy CT and ultrasound in gouty arthritis: A systematic review. Z Rheumatol. 2017 Oct;76(8):723-729. English. doi: 10.1007/s00393-016-0250-8.
Bindu S, Mazumder S, Bandyopadhyay U. Non-steroidal anti-inflammatory drugs (NSAIDs) and organ damage: A current perspective. Biochem Pharmacol. 2020 Oct;180:114147. doi: 10.1016/j.bcp.2020.114147. Epub 2020 Jul 10. PMID: 32653589; PMCID: PMC7347500, James DS. The multisystem adverse effects of NSAID therapy. J Am Osteopath Assoc. 1999 Nov 1;99(11_suppl):S1-S7. doi: 10.7556/jaoa.1999.99.11.S1. PMID: 26981697.
Lanas A, Boers M, Nuevo J. Gastrointestinal events in at-risk patients starting non-steroidal anti-inflammatory drugs (NSAIDs) for rheumatic diseases: the EVIDENCE study of European routine practice. Ann Rheum Dis. 2015;74(4):675-681. doi:10.1136/annrheumdis-2013-204155.
Каратеев АЕ, Насонов ЕЛ, Ивашкин ВТ, и др. Рациональное использование нестероидных противовоспалительных препаратов. Клинические рекомендации. Научно-практическая ревматология. 2018;56:1-29. doi:10.14412/1995-4484-2018-1-29.
Arfè A, Scotti L, Varas-Lorenzo C, et al. Non-steroidal anti-inflammatory drugs and risk of heart failure in four European countries: nested case-control study. BMJ. 2016;354:i4857. doi:10.1136/bmj.i4857.
Wang X, Li X, Wang H, et al. All-cause and specific mortality in patients with gout: A systematic review and meta-analysis. Semin Arthritis Rheum. 2023;63:152273. doi:10.1016/j.semarthrit.2023.152273.
Kawasoe S, Kubozono T, Yoshifuku S, et al. Uric Acid Level and Prevalence of Atrial Fibrillation in a Japanese General Population of 285,882. Circ J. 2016;80(12):2453-2459. doi:10.1253/circj.CJ-16-0766.
Lee SJ, Oh BK, Sung KC. Uric acid and cardiometabolic diseases. Clin Hypertens. 2020;26:13. doi:10.1186/s40885-020-00146-y.
Huang H, Huang B, Li Y, et al. Uric acid and risk of heart failure: a systematic review and meta-analysis. Eur J Heart Fail. 2014;16(1):15-24. doi:10.1093/eurjhf/hft132.
Kearney PM, Baigent C, Godwin J, at al. Do selective cyclo-oxygenase-2 inhibitors and traditional non-steroidal anti-inflammatory drugs increase the risk of atherothrombosis? Meta-analysis of randomised trials. BMJ. 2006;332:1302-8. doi:10.1136/bmj.332.7553.1302 pmid:16740558.
García Rodríguez LA, Tacconelli S, Patrignani P. Role of dose potency in the prediction of risk of myocardial infarction associated with nonsteroidal anti-inflammatory drugs in the general population. J Am Coll Cardiol. 2008;52:1628-36. doi:10.1016/j.jacc.2008.08.041 pmid:18992652.
McGettigan P, Henry D. Cardiovascular risk with non-steroidal anti-inflammatory drugs: systematic review of population-based controlled observational studies. PLoS Med. 2011;8:e1001098. doi:10.1371/journal.pmed.1001098 pmid:21980265.
Trelle S, Reichenbach S, Wandel S, et al. Cardiovascular safety of non-steroidal anti-inflammatory drugs: network meta-analysis. BMJ. 2011;342:c7086. doi:10.1136/bmj.c7086 pmid:21224324.
Bhala N, Emberson J, Merhi A, et al. Coxib and traditional NSAID Trialists’ (CNT) Collaboration. Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials. Lancet. 2013;382:769-79. doi:10.1016/S0140-6736(13)60900-9 pmid:23726390.
Vilaca T, Eastell R, Schini M. Osteoporosis in men. Lancet Diabetes Endocrinol. 2022 Apr;10(4):273-283. doi:10.1016/S2213-8587(22)00012-2.
Anam AK, Insogna K. Update on Osteoporosis Screening and Management. Med Clin North Am. 2021;105(6):1117-1134. doi:10.1016/j.mcna.2021.05.016.
Kaul S, Gupta M, Bandyopadhyay D, Hajra A, Deedwania P, Roddy E, Mamas M, Klein A, Lavie CJ, Fonarow GC, Ghosh RK. Gout Pharmacotherapy in Cardiovascular Diseases: A Review of Utility and Outcomes. Am J Cardiovasc Drugs. 2021 Sep;21(5):499-512. doi: 10.1007/s40256-020-00459-1.
Colantonio LD, Saag KG, Singh JA, et al. Gout is associated with an increased risk for incident heart failure among older adults: the REasons for Geographic And Racial Differences in Stroke (REGARDS) cohort study. Arthritis Res Ther. 2020;22(1):86. doi:10.1186/s13075-020-02175-2.
van Durme CM, Wechalekar MD, Landewé RB, et al. Non-steroidal anti-inflammatory drugs for acute gout. Cochrane Database Syst Rev. 2021;12(12):CD010120. doi:10.1002/14651858.CD010120.pub3.
FitzGerald JD, Dalbeth N, Mikuls T, et al. 2020 American College of Rheumatology Guideline for the Management of Gout [published correction appears in Arthritis Care Res (Hoboken). 2020 Aug;72(8):1187. doi: 10.1002/acr.24401.] [published correction appears in Arthritis Care Res (Hoboken). 2021 Mar;73(3):458. doi: 10.1002/acr.24566.]. Arthritis Care Res (Hoboken). 2020;72(6):744-760. doi:10.1002/acr.24180.
Li S, Yang H, Guo Y, et al. Comparative efficacy and safety of urate-lowering therapy for the treatment of hyperuricemia: a systematic review and network meta-analysis. Sci Rep. 2016;6:33082. doi:10.1038/srep33082.
Pascart T, Latourte A, Flipo RM, et al. 2020 recommendations from the French Society of Rheumatology for the management of gout: Urate-lowering therapy. Joint Bone Spine. 2020;87(5):395-404. doi:10.1016/j.jbspin.2020.05.002.
Hui M, Carr A, Cameron S, et al. The British Society for Rheumatology Guideline for the Management of Gout. Rheumatology (Oxford). 2017;56(7):1246. doi:10.1093/rheumatology/kex250.
Jeyaruban A, Larkins S, Soden M. Management of gout in general practice--a systematic review. Clin Rheumatol. 2015;34(1):9-16. doi:10.1007/s10067-014-2783-z.
Conley B, Bunzli S, Bullen J, et al. What are the core recommendations for gout management in first line and specialist care? Systematic review of clinical practice guidelines. BMC Rheumatol. 2023;7(1):15. doi:10.1186/s41927-023-00335-w.
Yu Y, Wang D, Zhou Q, et al. Recommendations in clinical practice guidelines on gout: systematic review and consistency analysis. Clin Exp Rheumatol. 2020;38(5):964-972.
Terkeltaub RA. Colchicine update: 2008. Semin Arthritis Rheum. 2009;38(6):411-419. doi:10.1016/j.semarthrit.2008.08.006.
Dalbeth N, Merriman TR, Stamp LK. Gout. Lancet. 2016;388(10055):2039-2052. doi:10.1016/S0140-6736(16)00346-9.
Doherty M, Jansen TL, Nuki G, et al. Gout: why is this curable disease so seldom cured?. Ann Rheum Dis. 2012;71(11):1765-1770. doi:10.1136/annrheumdis-2012-201687.
Keenan RT, O'Brien WR, Lee KH, et al. Prevalence of contraindications and prescription of pharmacologic therapies for gout. Am J Med. 2011;124(2):155-163. doi:10.1016/j.amjmed.2010.09.012.
Zhang W, Doherty M, Bardin T, et al. EULAR evidence based recommendations for gout. Part II: Management. Report of a task force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis. 2006;65(10):1312-1324. doi:10.1136/ard.2006.055269.
McKenzie BJ, Wechalekar MD, Johnston RV, et al. Colchicine for acute gout. Cochrane Database Syst Rev. 2021;8(8):CD006190. Published 2021 Aug 26. doi:10.1002/14651858.CD006190.pub3.
Wechalekar MD, Vinik O, Moi JH, et al. The efficacy and safety of treatments for acute gout: results from a series of systematic literature reviews including Cochrane reviews on intraarticular glucocorticoids, colchicine, nonsteroidal antiinflammatory drugs, and interleukin-1 inhibitors. J Rheumatol Suppl. 2014;92:15-25. doi:10.3899/jrheum.140458.
Billy CA, Lim RT, Ruospo M, et al. Corticosteroid or Nonsteroidal Antiinflammatory Drugs for the Treatment of Acute Gout: A Systematic Review of Randomized Controlled Trials. J Rheumatol. 2018;45(1):128-136. doi:10.3899/jrheum.170137.
Yu J, Lu H, Zhou J, et al. Oral prednisolone versus non-steroidal anti-inflammatory drugs in the treatment of acute gout: a meta-analysis of randomized controlled trials [published correction appears in Inflammopharmacology. 2019 Feb;27(1):199. doi: 10.1007/s10787-018-0518-5.]. Inflammopharmacology. 2018;26(3):717-723. doi:10.1007/s10787-018-0442-8.
Janssens HJ, Lucassen PL, Van de Laar FA, Janssen M, Van de Lisdonk EH. Systemic corticosteroids for acute gout. Cochrane Database Syst Rev. 2008;2008(2):CD005521. doi:10.1002/14651858.CD005521.pub2.
Reardon JA, Stockman A, Darlington LG, Scott JT. Double-blind trial of feprazone and phenylbutazone in acute gout. Curr Med Res Opin. 1980;6(7):445-448. doi:10.1185/03007998009109465.
Ruotsi A, Vainio U. Treatment of acute gouty arthritis with proquazone and indomethacin. A comparative, double-blind trial. Scand J Rheumatol Suppl. 1978;(21):15-17. doi:10.3109/03009747809095668.
Shrestha M, Morgan DL, Moreden JM, et al. Randomized double-blind comparison of the analgesic efficacy of intramuscular ketorolac and oral indomethacin in the treatment of acute gouty arthritis. Ann Emerg Med. 1995;26(6):682-686. doi:10.1016/s0196-0644(95)70037-4.
Siegmeth W, Placheta P. Doppelblindstudie: Ketoprofen gegen Phenylbutazon bei akuter Gichtarthritis [Double-blind trial: ketoprofen versus phenylbutazone in acute gouty arthritis (author's transl)]. Wien Klin Wochenschr. 1976;88(16):535-537.
Weiner GI, White SR, Weitzner RI, Rubinstein HM. Double-blind study of fenoprofen versus phenylbutazone in acute gouty arthritis. Arthritis Rheum. 1979;22(4):425-426. doi:10.1002/art.1780220420.
Terkeltaub RA, Furst DE, Bennett K, et al. High versus low dosing of oral colchicine for early acute gout flare: Twenty-four-hour outcome of the first multicenter, randomized, double-blind, placebo-controlled, parallel-group, dose-comparison colchicine study. Arthritis Rheum. 2010;62(4):1060-1068. doi:10.1002/art.27327.
Groff GD, Franck WA, Raddatz DA. Systemic steroid therapy for acute gout: a clinical trial and review of the literature. Semin Arthritis Rheum. 1990;19(6):329-336. doi:10.1016/0049-0172(90)90070-v.
Janssens HJ, Janssen M, van de Lisdonk EH, et al. Use of oral prednisolone or naproxen for the treatment of gout arthritis: a double-blind, randomised equivalence trial. Lancet. 2008;371(9627):1854-1860. doi:10.1016/S0140-6736(08)60799-0.
Федорова АА, Барскова ВГ, Якунина ИА, и др. Кратковременное применение глюкокортикоидов у больных с затяжным и хроническим подагрическим артритом. Часть II- сравнение эффективности различных лекарственных форм. Научно-практическая ревматология. 2008;46(5):72-75.
Ahern MJ, Reid C, Gordon TP, et al. Does colchicine work? The results of the first controlled study in acute gout. Aust N Z J Med. 1987;17(3):301-304. doi:10.1111/j.1445-5994.1987.tb01232.x.
Roddy E, Clarkson K, Blagojevic-Bucknall M, et al. Open-label randomised pragmatic trial (CONTACT) comparing naproxen and low-dose colchicine for the treatment of gout flares in primary care. Ann Rheum Dis. 2020;79(2):276-284. doi:10.1136/annrheumdis-2019-216154.
Pascart T, Robinet P, Ottaviani S, et al. Evaluating the safety and short-term equivalence of colchicine versus prednisone in older patients with acute calcium pyrophosphate crystal arthritis (COLCHICORT): an open-label, multicentre, randomised trial. Lancet Rheumatol. 2023;5(9):e523-e531. doi:10.1016/S2665-9913(23)00165-0.
Hansten PD, Tan MS, Horn JR, et al. Colchicine Drug Interaction Errors and Misunderstandings: Recommendations for Improved Evidence-Based Management. Drug Saf. 2023;46(3):223-242. doi:10.1007/s40264-022-01265-1.
Stamp LK, Horsley C, Karu LT, et al. Colchicine: the good, the bad, the ugly, and how to minimise the risks. Rheumatology (Oxford). 2023 Nov 29:kead625. doi: 10.1093/rheumatology/kead625.
Stewart S, Yang KCK, Atkins K, et al. Adverse events during oral colchicine use: a systematic review and meta-analysis of randomised controlled trials. Arthritis Res Ther. 2020;22(1):28. doi:10.1186/s13075-020-2120-7.
van Echteld I, Wechalekar MD, Schlesinger N, et al. Colchicine for acute gout. Cochrane Database Syst Rev. 2014;(8):CD006190. doi:10.1002/14651858.CD006190.pub2.
Finkelstein Y, Aks SE, Hutson JR, et al. Colchicine poisoning: the dark side of an ancient drug. Clin Toxicol (Phila). 2010;48(5):407-414. doi:10.3109/15563650.2010.495348.
Wason S, Mount D, Faulkner R. Single-dose, open-label study of the differences in pharmacokinetics of colchicine in subjects with renal impairment, including end-stage renal disease. Clin Drug Investig. 2014;34(12):845-855. doi:10.1007/s40261-014-0238-6.
Terkeltaub RA, Furst DE, Digiacinto JL, et al. Novel evidence-based colchicine dose-reduction algorithm to predict and prevent colchicine toxicity in the presence of cytochrome P450 3A4/P-glycoprotein inhibitors [published correction appears in Arthritis Rheum. 2011 Nov;63(11):3521. Dosage error in article text]. Arthritis Rheum. 2011;63(8):2226-2237. doi:10.1002/art.30389.
Terkeltaub RA. Clinical practice. Gout. N Engl J Med. 2003;349(17):1647-1655. doi:10.1056/NEJMcp030733.
Slobodnick A, Shah B, Krasnokutsky S, Pillinger MH. Update on colchicine, 2017. Rheumatology (Oxford). 2018;57(suppl_1):i4-i11. doi:10.1093/rheumatology/kex453.
Liu X, Sun D, Ma X, et al. Benefit-risk of corticosteroids in acute gout patients: An updated meta-analysis and economic evaluation. Steroids. 2017;128:89-94. doi:10.1016/j.steroids.2017.09.002.
Rainer TH, Cheng CH, Janssens HJ, et al. Oral Prednisolone in the Treatment of Acute Gout: A Pragmatic, Multicenter, Double-Blind, Randomized Trial. Ann Intern Med. 2016;164(7):464-471. doi:10.7326/M14-2070.
Федорова АА, Барскова ВГ, Якунина ИА, Насонова ВА. Кратковременное применение глюкокортикоидов у больных затяжным и хроническим подагрическим артритом. Часть III – частота развития нежелательных реакций. Научно-практическая ревматология. 2009;47(2):38-42.
Yasir M, Goyal A, Sonthalia S. Corticosteroid Adverse Effects. In: StatPearls. Treasure Island (FL): StatPearls Publishing; July 3, 2023.
Барскова ВГ, Кудаева ФМ. Применение гранулированной формы нимесулида при подагре. РМЖ. 2007;26:2020.
Барскова ВГ, Якунина ИА, Насонова ВА. Применение нимесила при подагрическом артрите. Терапевтических архив. 2003; 5: 60–4.
Kress HG, Baltov A, Basiński A, et al. Acute pain: a multifaceted challenge - the role of nimesulide. Curr Med Res Opin. 2016;32(1):23-36. doi:10.1185/03007995.2015.1100986.
Franck WA, Brown MM. Letter: Ibuprofen in acute polyarticular gout. Arthritis Rheum. 1976;19(2):269. doi:10.1002/art.1780190225.
Zeng L, Qasim A, Neogi T, et al. Efficacy and Safety of Pharmacologic Interventions in Patients Experiencing a Gout Flare: A Systematic Review and Network Meta-Analysis. Arthritis Care Res (Hoboken). 2021;73(5):755-764. doi:10.1002/acr.24402.
Soliman S, Ahmed RM, Ahmed MM, et al. Non-steroidal anti-inflammatory drugs: what is the actual risk of chronic kidney disease? A systematic review and meta-analysis. Rom J Intern Med. 2025;63(1):3-27. doi:10.2478/rjim-2024-0029.
Martín Arias LH, Martín González A, Sanz Fadrique R, Vazquez ES. Cardiovascular Risk of Nonsteroidal Anti-inflammatory Drugs and Classical and Selective Cyclooxygenase-2 Inhibitors: A Meta-analysis of Observational Studies. J Clin Pharmacol. 2019;59(1):55-73. doi:10.1002/jcph.1302.
Bally M, Dendukuri N, Rich B, et al. Risk of acute myocardial infarction with NSAIDs in real world use: bayesian meta-analysis of individual patient data. BMJ. 2017;357:j1909. doi:10.1136/bmj.j1909.
Schmidt M, Sørensen HT, Pedersen L. Diclofenac use and cardiovascular risks: series of nationwide cohort studies. BMJ. 2018;362:k3426. doi:10.1136/bmj.k3426.
Saag KG, Khanna PP, Keenan RT, et al. A Randomized, Phase II Study Evaluating the Efficacy and Safety of Anakinra in the Treatment of Gout Flares. Arthritis Rheumatol. 2021;73(8):1533-1542. doi: 10.1002/art.41699.
So A, De Smedt T, Revaz S, Tschopp J. A pilot study of IL-1 inhibition by anakinra in acute gout. Arthritis Res Ther. 2007;9(2):R28. doi:10.1186/ar2143.
Martinon F, Pétrilli V, Mayor A, et al. Gout-associated uric acid crystals activate the NALP3 inflammasome. Nature. 2006;440(7081):237-241. doi:10.1038/nature04516.
Bursill D, Taylor WJ, Terkeltaub R, et al. Gout, Hyperuricemia, and Crystal-Associated Disease Network Consensus Statement Regarding Labels and Definitions for Disease Elements in Gout. Arthritis Care Res (Hoboken). 2019;71(3):427-434. doi:10.1002/acr.23607.
Lee YH, Song GG. Effect of urate-lowering therapy on all-cause and CVD-specific mortality in gout and hyperuricemia: a meta-analysis. Auswirkungen von harnsäuresenkender Therapie auf die Gesamt- und die kardiovaskuläre Mortalität bei Gicht und Hyperurikämie: eine Metaanalyse. Z Rheumatol. 2024;83(Suppl 3):338-344. doi:10.1007/s00393-024-01600-0.
Pérez Ruiz F, Richette P, Stack AG, et al. Failure to reach uric acid target of <0.36 mmol/L in hyperuricaemia of gout is associated with elevated total and cardiovascular mortality. RMD Open. 2019;5(2):e001015.. doi:10.1136/rmdopen-2019-001015.
Pagidipati NJ, Clare RM, Keenan RT, et al. Association of Gout With Long-Term Cardiovascular Outcomes Among Patients With Obstructive Coronary Artery Disease. J Am Heart Assoc. 2018;7(16):e009328. doi:10.1161/JAHA.118.009328.
Bardin T. Hyperuricemia starts at 360 micromoles (6 mg/dL). Joint Bone Spine. 2015;82(3):141-143. doi:10.1016/j.jbspin.2015.01.002.
Goldfien R, Pressman A, Jacobson A, et al. A Pharmacist-Staffed, Virtual Gout Management Clinic for Achieving Target Serum Uric Acid Levels: A Randomized Clinical Trial. Perm J. 2016;20(3):15-234. doi:10.7812/TPP/15-234.
Mikuls TR, Cheetham TC, Levy GD, et al. Adherence and Outcomes with Urate-Lowering Therapy: A Site-Randomized Trial. Am J Med. 2019;132(3):354-361. doi:10.1016/j.amjmed.2018.11.011.
Ellmann H, Bayat S, Araujo E, et al. Effects of Conventional Uric Acid-Lowering Therapy on Monosodium Urate Crystal Deposits. Arthritis Rheumatol. 2020;72(1):150-156. doi:10.1002/art.41063.
Pascart T, Grandjean A, Capon B, et al. Monosodium urate burden assessed with dual-energy computed tomography predicts the risk of flares in gout: a 12-month observational study: MSU burden and risk of gout flare. Arthritis Res Ther. 2018;20(1):210. doi:10.1186/s13075-018-1714-9.
Doherty M, Jenkins W, Richardson H, et al. Efficacy and cost-effectiveness of nurse-led care involving education and engagement of patients and a treat-to-target urate-lowering strategy versus usual care for gout: a randomised controlled trial. Lancet. 2018;392(10156):1403-1412. doi:10.1016/S0140-6736(18)32158-5.
Stamp LK, Frampton C, Morillon MB, et al. Association between serum urate and flares in people with gout and evidence for surrogate status: a secondary analysis of two randomised controlled trials. Lancet Rheumatol. 2022;4(1):e53-e60. https://doi.org/10.1016/S2665-9913(21)00319-2.
Schretlen DJ, Inscore AB, Vannorsdall TD, et al. Serum uric acid and brain ischemia in normal elderly adults. Neurology. 2007;69(14):1418-1423. doi:10.1212/01.wnl.0000277468.10236.f1.
Chen H, Mosley TH, Alonso A, Huang X. Plasma urate and Parkinson's disease in the Atherosclerosis Risk in Communities (ARIC) study. Am J Epidemiol. 2009;169(9):1064-1069. doi:10.1093/aje/kwp033.
Weisskopf MG, O'Reilly E, Chen H, et al. Plasma urate and risk of Parkinson's disease. Am J Epidemiol. 2007;166(5):561-567. doi:10.1093/aje/kwm127.
Kim TS, Pae CU, Yoon SJ, et al. Decreased plasma antioxidants in patients with Alzheimer's disease. Int J Geriatr Psychiatry. 2006;21(4):344-348. doi:10.1002/gps.1469.
Abraham A, Drory VE. Influence of serum uric acid levels on prognosis and survival in amyotrophic lateral sclerosis: a meta-analysis. J Neurol. 2014;261(6):1133-1138. doi:10.1007/s00415-014-7331-x.
Taylor TH, Mecchella JN, Larson RJ, et al. Initiation of allopurinol at first medical contact for acute attacks of gout: a randomized clinical trial. Am J Med. 2012;125(11):1126-1134.e7. doi:10.1016/j.amjmed.2012.05.025.
Seth R, Kydd AS, Buchbinder R, et al. Allopurinol for chronic gout. Cochrane Database Syst Rev. 2014;2014(10):CD006077. doi:10.1002/14651858.CD006077.pub3.
Perez-Ruiz F, Herrero-Beites AM, Carmona L. A two-stage approach to the treatment of hyperuricemia in gout: the "dirty dish" hypothesis. Arthritis Rheum. 2011;63(12):4002-4006. doi:10.1002/art.30649.
Schumacher HR Jr, Becker MA, Wortmann RL, et al. Effects of febuxostat versus allopurinol and placebo in reducing serum urate in subjects with hyperuricemia and gout: a 28-week, phase III, randomized, double-blind, parallel-group trial. Arthritis Rheum. 2008;59(11):1540-1548. doi:10.1002/art.24209.
O'Dell JR, Brophy MT, Pillinger MH, et al. Comparative Effectiveness of Allopurinol and Febuxostat in Gout Management [published correction appears in NEJM Evid. 2022 Jul;1(7):EVIDx2200150. doi: 10.1056/EVIDx2200150.] [published correction appears in NEJM Evid. 2022 Aug;1(8):EVIDx2200180. doi: 10.1056/EVIDx2200180.]. NEJM Evid. 2022;1(3):10.1056/evidoa2100028. doi:10.1056/evidoa2100028.
Jutkowitz E, Choi HK, Pizzi LT, Kuntz KM. Cost-effectiveness of allopurinol and febuxostat for the management of gout. Ann Intern Med. 2014;161(9):617-626. doi:10.7326/M14-0227.
Dalbeth N, Kumar S, Stamp L, Gow P. Dose adjustment of allopurinol according to creatinine clearance does not provide adequate control of hyperuricemia in patients with gout. J Rheumatol. 2006;33(8):1646-1650.
Yokose C, Lu N, Xie H, et al. Heart disease and the risk of allopurinol-associated severe cutaneous adverse reactions: a general population-based cohort study. CMAJ. 2019;191(39):E1070-E1077. doi:10.1503/cmaj.190339.
Jennings CG, Mackenzie IS, Flynn R, et al. Up-titration of allopurinol in patients with gout. Semin Arthritis Rheum. 2014;44(1):25-30. doi:10.1016/j.semarthrit.2014.01.004.
Елисеев М.С., Чикина М.Н., Желябина О.В. Открытое 6-месячное исследование эффективности титрования дозы аллопуринола у пациентов с подагрой в рамках стратегии «лечение до цели». РМЖ. 2022;6:17–22.
Rees F, Jenkins W, Doherty M. Patients with gout adhere to curative treatment if informed appropriately: proof-of-concept observational study. Ann Rheum Dis. 2013;72(6):826-830. doi:10.1136/annrheumdis-2012-201676.
Stamp LK, Taylor WJ, Jones PB, et al. Starting dose is a risk factor for allopurinol hypersensitivity syndrome: a proposed safe starting dose of allopurinol. Arthritis Rheum. 2012;64(8):2529-2536. doi:10.1002/art.34488.
Stamp LK, O’Donnell JL, Zhang M, et al. Using allopurinol above the dose based on creatinine clearance is effective and safe in patients with chronic gout, including those with renal impairment. Arthritis Rheum. 2011;63(2):412-421. Doi:10.1002/art.30119.
Becker MA, Schumacher HR Jr, Wortmann RL, et al. Febuxostat compared with allopurinol in patients with hyperuricemia and gout. N Engl J Med. 2005;353(23):2450-2461. doi:10.1056/NEJMoa050373.
Becker MA, Schumacher HR Jr, Wortmann RL, et al. Febuxostat, a novel nonpurine selective inhibitor of xanthine oxidase: a twenty-eight-day, multicenter, phase II, randomized, double-blind, placebo-controlled, dose-response clinical trial examining safety and efficacy in patients with gout. Arthritis Rheum. 2005;52(3):916-923. doi:10.1002/art.20935.
Koto R, Nakajima A, Horiuchi H, Yamanaka H. Factors associated with achieving target serum uric acid level and occurrence of gouty arthritis: A retrospective observational study of Japanese health insurance claims data. Pharmacoepidemiol Drug Saf. 2021;30(2):157-168. doi:10.1002/pds.5127.
Kim YE, Ahn SM, Oh JS, et al. Febuxostat dose requirement according to renal function in patients who achieve target serum urate levels: A retrospective cohort study. Joint Bone Spine. 2024;91(2):105668. doi:10.1016/j.jbspin.2023.105668.
Gao L, Wang B, Pan Y, Lu Y, Cheng R. Cardiovascular safety of febuxostat compared to allopurinol for the treatment of gout: A systematic and meta-analysis. Clin Cardiol. 2021 Jul;44(7):907-916. doi: 10.1002/clc.23643.
Xie H, Hu N, Pan T, et al. Effectiveness and safety of different doses of febuxostat compared with allopurinol in the treatment of hyperuricemia: a meta-analysis of randomized controlled trials. BMC Pharmacol Toxicol. 2023;24(1):79. doi:10.1186/s40360-023-00723-5.
Чикина МН, Елисеев МС, Желябина ОВ. Практическое применение национальных клинических рекомендаций по лечению подагры (предварительные данные). Современная ревматология. 2020; 14(2):97-103. doi: 10.14412/1996-7012-2020-2-97-103.
Becker MA, Schumacher HR, MacDonald PA, et al. Clinical efficacy and safety of successful longterm urate lowering with febuxostat or allopurinol in subjects with gout. J Rheumatol. 2009;36(6):1273-1282. doi:10.3899/jrheum.080814.
Tausche AK, Reuss-Borst M, Koch U. Urate lowering therapy with febuxostat in daily practice-a multicentre, open-label, prospective observational study. Int J Rheumatol. 2014;2014:123105. doi:10.1155/2014/123105.
Елисеев МС, Чикина МН, Желябина ОВ. Влияние фебуксостата на вероятность достижения целевого уровня мочевой кислоты в сыворотке крови и почечную функцию у пациентов с подагрой: результаты проспективного наблюдательного исследования. Эффективная фармакотерапия. 2023;19(29):16–21. doi:10.33978/2307-3586-2023-19-29-16-21.
O'Dell JR, Brophy MT, Pillinger MH, et al. Comparative Effectiveness of Allopurinol and Febuxostat in Gout Management [published correction appears in NEJM Evid. 2022;1(7):EVIDx2200150. doi: 10.1056/EVIDx2200150.] [published correction appears in NEJM Evid. 2022 Aug;1(8):EVIDx2200180. doi: 10.1056/EVIDx2200180.]. NEJM Evid. 2022;1(3):10.1056/evidoa2100028. doi:10.1056/evidoa2100028
Yang XH, Zhang BL, Cheng Y, et al. Febuxostat provides renoprotection in patients with hyperuricemia or gout: a systematic review and meta-analysis of randomized controlled trials. Ann Med. 2024;56(1):2332956. doi:10.1080/07853890.2024.2332956.
Kim SH, Lee SY, Kim JM, Son CN. Renal safety and urate-lowering efficacy of febuxostat in gout patients with stage 4-5 chronic kidney disease not yet on dialysis. Korean J Intern Med. 2020;35(4):998-1003. doi:10.3904/kjim.2018.423.
Kim YE, Ahn SM, Oh JS, et al. Febuxostat dose requirement according to renal function in patients who achieve target serum urate levels: A retrospective cohort study. Joint Bone Spine. 2024;91(2):105668. doi:10.1016/j.jbspin.2023.105668.
Елисеев МС, Желябина ОВ, Чикина МН, Тхакоков ММ. Эффективность фебуксостата у пациентов с подагрой в зависимости от функции почек. РМЖ. Медицинское обозрение. 2022;6(3):140-147. doi:10.32364/2587-6821-2022-6-3-140-147.
Елисеев МС, Чикина МН, Желябина ОВ. Эффективность фебуксостата у пациентов с умеренным снижением функции почек: результаты пилотного исследования. Эффективная фармакотерапия. 2024;20(10):6–11. doi:10.33978/2307-3586-2024-20-10-6-11.
Lee MKR, Lim YNA. Initiation of Urate Lowering Therapy (ULT). The Singapore Family Physician. 2022;48(1):23-27. doi:10.33591/sfp.49.1.u4.
Qurie A, Preuss CV, Musa R. Allopurinol. In: StatPearls. Treasure Island (FL): StatPearls Publishing; June 26, 2023.
Becker MA, Fitz-Patrick D, Choi HK, et al. An open-label, 6-month study of allopurinol safety in gout: The LASSO study. Semin Arthritis Rheum. 2015;45(2):174-183. doi:10.1016/j.semarthrit.2015.05.005.
de Lautour H, Taylor WJ, Adebajo A, et al. Development of Preliminary Remission Criteria for Gout Using Delphi and 1000Minds Consensus Exercises. Arthritis Care Res (Hoboken). 2016;68(5):667-672. doi:10.1002/acr.22741.
Robinson PC, Dalbeth N, Donovan P. The Cost-effectiveness of Biannual Serum Urate (SU) Monitoring after Reaching Target in Gout: A Health Economic Analysis Comparing SU Monitoring [published correction appears in J Rheumatol. 2019;46(3):330]. J Rheumatol. 2018;45(5):697-704. doi:10.3899/jrheum.170199.
Sutton Burke EM, Kelly TC, Shoales LA, Nagel AK. Angiotensin Receptor Blockers Effect on Serum Uric Acid-A Class Effect?. J Pharm Pract. 2020;33(6):874-881. doi:10.1177/0897190019866315.
Daskalopoulou SS, Tzovaras V, Mikhailidis DP, Elisaf M. Effect on serum uric acid levels of drugs prescribed for indications other than treating hyperuricaemia. Curr Pharm Des. 2005;11(32):4161-4175. doi:10.2174/138161205774913309.
Miao Y, Ottenbros SA, Laverman GD, et al. Effect of a reduction in uric acid on renal outcomes during losartan treatment: a post hoc analysis of the reduction of endpoints in non-insulin-dependent diabetes mellitus with the Angiotensin II Antagonist Losartan Trial. Hypertension. 2011;58(1):2-7. doi:10.1161/HYPERTENSIONAHA.111.171488.
Derosa G, Maffioli P, Sahebkar A. Plasma uric acid concentrations are reduced by fenofibrate: A systematic review and meta-analysis of randomized placebo-controlled trials. Pharmacol Res. 2015;102:63-70. doi:10.1016/j.phrs.2015.09.012.
Hepburn AL, Kaye SA, Feher MD. Long-term remission from gout associated with fenofibrate therapy. Clin Rheumatol. 2003;22(1):73-76. doi:10.1007/s10067-002-0658-1.
Zhao Y, Xu L, Tian D, et al. Effects of sodium‐glucose co‐transporter 2 (SGLT2) inhibitors on serum uric acid level: A meta‐analysis of randomized controlled trials. Diabetes, Obesity and Metabolism. 2017;20(2):458–62. doi:10.1111/dom.13101.
Xin Y, Guo Y, Li Y, et al. Effects of sodium glucose cotransporter-2 inhibitors on serum uric acid in type 2 diabetes mellitus: A systematic review with an indirect comparison meta-analysis. Saudi Journal of Biological Sciences. 2019;26(2):421–6. doi:10.1016/j.sjbs.2018.11.013.
Ghukasyan H, Pedro Navalha DD, Pérez Romero I, et al. Reducing hyperuricemic events with SGLT2 inhibitors: An updated systematic review with meta-regression. Endocrinol Diabetes Nutr (Engl Ed). 2025;72(1):26-36. doi:10.1016/j.endien.2024.12.005.
Wang A, Shi W, Zhang N, et al. X. Newer Glucose-Lowering Drugs and Risk of Gout: A Network Meta-Analysis of Randomized Outcomes Trials. Clin Ther. 2024;46(11):851-854. doi:10.1016/j.clinthera.2024.04.013.
Lai SW, Hwang BF, Kuo YH, et al. Sodium-glucose cotransporter-2 inhibitors use and the risk of gout: a systematic review and meta-analysis. Front Endocrinol (Lausanne). 2023;14:1158153. doi:10.3389/fendo.2023.1158153.
Butt JH, Docherty KF, Claggett BL, et al. Association of Dapagliflozin Use With Clinical Outcomes and the Introduction of Uric Acid-Lowering Therapy and Colchicine in Patients With Heart Failure With and Without Gout: A Patient-Level Pooled Meta-analysis of DAPA-HF and DELIVER. JAMA Cardiol. 2023;8(4):386-393. doi:10.1001/jamacardio.2022.5608.
Caulfield MJ, Munroe PB, O’Neill D, et al. SLC2A9 Is a High-Capacity Urate Transporter in Humans. Hattersley A, editor. PLoS Medicine. 2008;5(10):e197. doi:10.1371/journal.pmed.0050197.
Singh JA, Reddy SG, Kundukulam J. Risk factors for gout and prevention: a systematic review of the literature. Curr Opin Rheumatol. 2011;23(2):192-202. doi:10.1097/BOR.0b013e3283438e13.
Hueskes BA, Roovers EA, Mantel-Teeuwisse AK, Janssens HJ, van de Lisdonk EH, Janssen M. Use of diuretics and the risk of gouty arthritis: a systematic review. Semin Arthritis Rheum. 2012;41(6):879-889. doi:10.1016/j.semarthrit.2011.11.008.
Ranieri L, Contero C, Peral ML, et al. Impact of diuretics on the urate lowering therapy in patients with gout: analysis of an inception cohort. Arthritis Res Ther. 2018;20(1):53. doi:10.1186/s13075-018-1559-2.
Zhang P, Wang H, Chen XH, et al. Effect of low-dose aspirin on serum uric acid levels in Chinese individuals over 60: subanalysis of a multicentre randomized clinical trial. Eur Rev Med Pharmacol Sci. 2020;24(5):2719-2724. doi:10.26355/eurrev_202003_20544.
Yu J, Qiu Q, Liang L, et al. Prophylaxis of acute flares when initiating febuxostat for chronic gouty arthritis in a real-world clinical setting. Mod Rheumatol. 2018;28(2):339-344. doi:10.1080/14397595.2017.1318467.
Елисеев МС, Чикина МН, Желябина ОВ, Кузьмина ЯИ, Панина ЕВ, Насонов ЕЛ. Эффективность и безопасность длительного приема различных доз колхицина у пациентов с подагрой. Научно-практическая ревматология. 2025;63(2):197-201. doi:10.47360/1995-4484-2025-197-201.
Wortmann RL, Macdonald PA, Hunt B, Jackson RL. Effect of prophylaxis on gout flares after the initiation of urate-lowering therapy: analysis of data from three phase III trials. Clin Ther. 2010;32(14):2386-2397. doi:10.1016/j.clinthera.2011.01.008.
Huang X, Du H, Gu J, et al. An allopurinol-controlled, multicenter, randomized, double-blind, parallel between-group, comparative study of febuxostat in Chinese patients with gout and hyperuricemia. Int J Rheum Dis. 2014;17(6):679-686. doi:10.1111/1756-185X.12266.
Чикина МН, Елисеев МС, Желябина ОВ. Сравнение эффективности и безопасности различных противовоспалительных препаратов при инициации уратснижающей терапии у пациентов с подагрой (предварительные данные). Современная ревматология. 2021;15(2):50–56. doi:10.14412/1996-7012-2021-2-50-56.
Wan H, Zeng L, Xiao R, et al. Colchicine linked with risk reduction for myocardial infarction in gout patients: systematic review and meta-analysis. Z Rheumatol. 2022 Aug;81(6):501-506. English. doi: 10.1007/s00393-022-01232-2.
Siddiqui MU, Junarta J, Sathyanarayanan S, et al. Risk of coronary artery disease in patients with gout on treatment with Colchicine: A systematic review and meta-analysis. Int J Cardiol Heart Vasc. 2023;45:101191. doi: 10.1016/j.ijcha.2023.101191.
Hennessy T, Soh L, Bowman M, et al. The Low Dose Colchicine after Myocardial Infarction (LoDoCo-MI) study: A pilot randomized placebo controlled trial of colchicine following acute myocardial infarction. Am Heart J. 2019;215:62-69. doi:10.1016/j.ahj.2019.06.003.
Nidorf SM, Eikelboom JW, Budgeon CA, Thompson PL. Low-dose colchicine for secondary prevention of cardiovascular disease. J Am Coll Cardiol. 2013;61(4):404-410. doi:10.1016/j.jacc.2012.10.027.
Nidorf SM, Fiolet ATL, Mosterd A, et al. Colchicine in Patients with Chronic Coronary Disease. N Engl J Med. 2020;383(19):1838-1847. doi:10.1056/NEJMoa2021372.
Tardif JC, Kouz S, Waters DD, et al. Efficacy and Safety of Low-Dose Colchicine after Myocardial Infarction. N Engl J Med. 2019;381(26):2497-2505. doi:10.1056/NEJMoa1912388.
Andreis A, Imazio M, Piroli F, et al. Efficacy and safety of colchicine for the prevention of major cardiovascular and cerebrovascular events in patients with coronary artery disease: a systematic review and meta-analysis on 12 869 patients. Eur J Prev Cardiol. 2022;28(17):1916-1925. doi:10.1093/eurjpc/zwab045.
Saseen JJ, Agashivala N, Allen RR, et al. Comparison of patient characteristics and gout-related health-care resource utilization and costs in patients with frequent versus infrequent gouty arthritis attacks. Rheumatology (Oxford). 2012;51(11):2004-2012. doi:10.1093/rheumatology/kes183.
Насонов ЕЛ, Яхно НН, Каратеев АЕ, и др. Общие принципы лечения скелетно-мышечной боли: междисциплинарный консенсус. Научно-практическая ревматология. 2016;54(3):247-265. doi:10.14412/1995-4484-2016-247-265.
Елисеев МС, Новикова АМ, Желябина ОВ, и др. Оценка сердечно-сосудистого риска у пациентов с микрокристаллическими артритами и ревматоидным артритом с помощью шкал ATP III и Reynolds Risk Score. Научно-практическая ревматология. 2020;58(5):512–519. doi:10.47360/1995-4484-2020-512-519.
Ly J, Gow P, Dalbeth N. Colchicine prescribing and safety monitoring in patients with gout. N Z Med J. 2007;120(1265):U2808.
Kuncl RW, Duncan G, Watson D, et al. Colchicine myopathy and neuropathy. N Engl J Med. 1987;316(25):1562-1568. doi:10.1056/NEJM198706183162502.
Kuritzky L, Panchal R. Gout: nonsteroidal anti-inflammatory drugs and colchicine to prevent painful flares during early urate-lowering therapy. J Pain Palliat Care Pharmacother. 2010;24(4):397-401. doi:10.3109/15360288.2010.526689.
Singh J., Yang S., Foster J. The risk of aplastic anemia and pancytopenia with colchicine: a retrospective study of integrated health system database. Art. Rheum. 2014;66;(11):20.
Pisaniello HL, Fisher MC, Farquhar H, et al. Efficacy and safety of gout flare prophylaxis and therapy use in people with chronic kidney disease: a Gout, Hyperuricemia and Crystal-Associated Disease Network (G-CAN)-initiated literature review. Arthritis Res Ther. 2021;23(1):130. doi:10.1186/s13075-021-02416-y.
Latourte A, Bardin T, Richette P. Prophylaxis for acute gout flares after initiation of urate-lowering therapy. Rheumatology (Oxford). 2014;53(11):1920-1926. doi:10.1093/rheumatology/keu157.
Chen M, Fu W, Xu H, Liu CJ. Pathogenic mechanisms of glucocorticoid-induced osteoporosis. Cytokine Growth Factor Rev. 2023;70:54-66. doi:10.1016/j.cytogfr.2023.03.002.
Ralston SH, Capell HA, Sturrock RD. Alcohol and response to treatment of gout. Br Med J (Clin Res Ed). 1988;296(6637):1641-1642. doi:10.1136/bmj.296.6637.1641-a.
Liu K, Yao Y, Chen W, et al. Modifiable risk factors and incidence of gout: Estimation of population attributable fraction in the US. Semin Arthritis Rheum. 2022;55:152040. doi: 10.1016/j.semarthrit.2022.152040.
Flynn TJ, Cadzow M, Dalbeth N, et al. Positive association of tomato consumption with serum urate: support for tomato consumption as an anecdotal trigger of gout flares. BMC Musculoskelet Disord. 2015;16:196.. doi:10.1186/s12891-015-0661-8.
Zhang Y, Chen C, Choi H, et al. Purine-rich foods intake and recurrent gout attacks. Ann Rheum Dis. 2012;71(9):1448-1453. doi:10.1136/annrheumdis-2011-201215.
Zhang Y, Chen S, Yuan M, et al. Gout and Diet: A Comprehensive Review of Mechanisms and Management. Nutrients. 2022;14(17):3525. doi: 10.3390/nu14173525.
Li R, Yu K, Li C. Dietary factors and risk of gout and hyperuricemia: a meta-analysis and systematic review. Asia Pac J Clin Nutr. 2018;27(6):1344-1356. doi:10.6133/apjcn.201811_27(6).0022.
Stirpe F, Della Corte E, Bonetti E, et al. Fructose-induced hyperuricaemia. Lancet. 1970;2(7686):1310-1311. doi:10.1016/s0140-6736(70)92269-5.
Zhou J, Wang Y, Lian F, et al. Physical exercises and weight loss in obese patients help to improve uric acid. Oncotarget. 2017;8(55):94893-94899. doi:10.18632/oncotarget.22046.
Nielsen SM, Bartels EM, Henriksen M, et al. Weight loss for overweight and obese individuals with gout: a systematic review of longitudinal studies. Ann Rheum Dis. 2017;76(11):1870-1882. doi:10.1136/annrheumdis-2017-211472.
Дедов ИИ, Шестакова МВ, Мельниченко ГА, и др. Междисциплинарные клинические рекомендации «Лечение ожирения и коморбидных заболеваний». Ожирение и метаболизм. 2021;18(1):5–99. doi: 10.14341/omet12714.
Chen JH, Wen CP, Wu SB, et al. Attenuating the mortality risk of high serum uric acid: the role of physical activity underused. Ann Rheum Dis. 2015;74(11):2034-2042. doi:10.1136/annrheumdis-2014-205312.
Park DY, Kim YS, Ryu SH, Jin YS. The association between sedentary behavior, physical activity and hyperuricemia. Vasc Health Risk Manag. 2019;15:291-299. doi:10.2147/VHRM.S200278.
Jablonski K, Young NA, Henry C, et al. Physical activity prevents acute inflammation in a gout model by downregulation of TLR2 on circulating neutrophils as well as inhibition of serum CXCL1 and is associated with decreased pain and inflammation in gout patients. PLoS One. 2020;15(10):e0237520. doi:10.1371/journal.pone.0237520.
Carcione J, Bodofsky S, LaMoreaux B, Schlesinger N. Beyond Medical Treatment: Surgical Treatment of Gout. Curr Rheumatol Rep. 2020;23(1):1. doi:10.1007/s11926-020-00969-6.
Harlianto NI, Harlianto ZN. Patient characteristics, surgical treatment, and outcomes in spinal gout: a systematic review of 315 cases. Eur Spine J. 2023;32(11):3697-3703. doi:10.1007/s00586-023-07942-8.
Poratt D, Rome K. Surgical Management of Gout in the Foot and Ankle A Systematic Review. J Am Podiatr Med Assoc. 2016;106(3):182-188. doi:10.7547/14-128.
Tan YL, Chen J, Ramalingam MB. Pan-Spinal Cord Compression From Gout: Visual Vignette of a Young Male Patient With Three Spinal Decompressive Surgeries. Am J Phys Med Rehabil. 2021;100(4):e58-e59. doi:10.1097/PHM.0000000000001524.
Ding Y, Wang W, Jiang W, et al. Tophaceous gout causing thoracic spinal cord compression: Case report and review of the literature. Neurochirurgie. 2018;64(3):171-176. doi:10.1016/j.neuchi.2017.11.002.
Kuo CF, Chou IJ, See LC, et al. Urate-lowering treatment and risk of total joint replacement in patients with gout. Rheumatology (Oxford). 2018;57(12):2129-2139. doi:10.1093/rheumatology/key212.
Teng GG, Leung YY, Ang LW, et al. Gout and risk of knee replacement for severe knee osteoarthritis in the Singapore Chinese Health Study. Osteoarthritis Cartilage. 2017;25(12):1962-1968. doi:10.1016/j.joca.2017.07.017.
Selvadurai D, Coleshill MJ, Day RO, et al. Patient factors and health outcomes associated with illness perceptions in people with gout. Rheumatology (Oxford). 2024;63(7):1927-1937. doi:10.1093/rheumatology/kead501.
Criscuolo M, Fianchi L, Dragonetti G, Pagano L. Tumor lysis syndrome: review of pathogenesis, risk factors and management of a medical emergency. Expert Rev Hematol. 2016;9(2):197-208. doi:10.1586/17474086.2016.1127156.
Bellos I, Kontzoglou K, Psyrri A, Pergialiotis V. Febuxostat administration for the prevention of tumour lysis syndrome: A meta-analysis. J Clin Pharm Ther. 2019;44(4):525-533. doi:10.1111/jcpt.12839.
Tamura K, Kawai Y, Kiguchi T, et al. Efficacy and safety of febuxostat for prevention of tumor lysis syndrome in patients with malignant tumors receiving chemotherapy: a phase III, randomized, multi-center trial comparing febuxostat and allopurinol. Int J Clin Oncol. 2016;21(5):996-1003. doi:10.1007/s10147-016-0971-3.
Mirrakhimov AE, Voore P, Khan M, Ali AM. Tumor lysis syndrome: A clinical review. World J Crit Care Med. 2015;4(2):130-138. doi:10.5492/wjccm.v4.i2.130.
Cairo MS, Bishop M. Tumour lysis syndrome: new therapeutic strategies and classification. Br J Haematol. 2004;127(1):3-11. doi:10.1111/j.1365-2141.2004.05094.x.
Coiffier B, Altman A, Pui CH, et al. Guidelines for the management of pediatric and adult tumor lysis syndrome: an evidence-based review [published correction appears in J Clin Oncol. 2010 Feb 1;28(4):708]. J Clin Oncol. 2008;26(16):2767-2778. doi:10.1200/JCO.2007.15.0177.
Cohen LF, Balow JE, Magrath IT, et al. Acute tumor lysis syndrome. A review of 37 patients with Burkitt's lymphoma. Am J Med. 1980;68(4):486-491. doi:10.1016/0002-9343(80)90286-7.
Howren A, Tsao NW, Choi HK, et al. eHealth-supported decentralized multi-disciplinary care for gout involving rheumatology, pharmacy, and dietetics: proof-of-concept study. Clin Rheumatol. 2020;39(4):1241-1249. doi:10.1007/s10067-019-04809-6.
Fields TR, Rifaat A, Yee AMF, et al. Pilot study of a multidisciplinary gout patient education and monitoring program. Semin Arthritis Rheum. 2017;46(5):601-608. doi:10.1016/j.semarthrit.2016.10.006.
Edwards NL, Schlesinger N, Clark S, et al. Management of Gout in the United States: A Claims-based Analysis. ACR Open Rheumatol. 2020;2(3):180-187. doi:10.1002/acr2.11121.
Keely E, Rostom K, Smith D, Liddy C. A comparison of faxed referrals and eConsult questions for rheumatology referrals: a descriptive study. CMAJ Open. 2021;9(1):E38-E43. doi:10.9778/cmajo.20200025.
Mikuls TR, Farrar JT, Bilker WB, et al. Suboptimal physician adherence to quality indicators for the management of gout and asymptomatic hyperuricaemia: results from the UK General Practice Research Database (GPRD). Rheumatology (Oxford). 2005;44(8):1038-1042. doi:10.1093/rheumatology/keh679.
Neogi T, Hunter DJ, Chaisson CE, et al. Frequency and predictors of inappropriate management of recurrent gout attacks in a longitudinal study. J Rheumatol. 2006;33(1):104-109.
Roddy E, Mallen CD, Hider SL, Jordan KP. Prescription and comorbidity screening following consultation for acute gout in primary care. Rheumatology (Oxford). 2010;49(1):105-111. doi:10.1093/rheumatology/kep332.
Roddy E, Zhang W, Doherty M. Concordance of the management of chronic gout in a UK primary-care population with the EULAR gout recommendations. Ann Rheum Dis. 2007;66(10):1311-1315. doi:10.1136/ard.2007.070755.
Singh JA, Wells GA, Christensen R, et al. Adverse effects of biologics: a network meta-analysis and Cochrane overview. Cochrane Database Syst Rev. 2011;2011(2):CD008794. doi:10.1002/14651858.CD008794.pub2.
Ridker PM, Everett BM, Thuren T, et al. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N Engl J Med. 2017;377(12):1119-1131. doi:10.1056/NEJMoa1707914.
Yokose C, McCormick N, Chen C, et al. Risk of gout flares after vaccination: a prospective case cross-over study. Ann Rheum Dis. 2019;78(11):1601-1604. doi:10.1136/annrheumdis-2019-215724.
American Academy of Pediatrics Committee on Drugs. Transfer of drugs and other chemicals into human milk. Pediatrics. 2001;108(3):776-789. doi:10.1542/peds.108.3.776.
Pecoraro V, Trenti T. Predictive value of serum uric acid levels for adverse maternal and perinatal outcomes in pregnant women with high blood pressure. A systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2020;252:447-454. doi:10.1016/j.ejogrb.2020.07.042.
Febuxostat Pregnancy and Breastfeeding Warnings. (Electronic resource). URL: https://www.drugs.com/pregnancy/febuxostat.html. (Last updated on Feb 12, 2025); (date of treatment: 03.05.2025)
Koopmans CM, van Pampus MG, Groen H, et al. Accuracy of serum uric acid as a predictive test for maternal complications in pre-eclampsia: bivariate meta-analysis and decision analysis. Eur J Obstet Gynecol Reprod Biol. 2009;146(1):8-14. doi:10.1016/j.ejogrb.2009.05.014.
Simsek M, Opperman RCM, Mulder CJJ, et al. The teratogenicity of allopurinol: A comprehensive review of animal and human studies. Reprod Toxicol. 2018;81:180-187. doi:10.1016/j.reprotox.2018.08.012.
Khanna D, Fitzgerald JD, Khanna PP et al. 2012 American College of Rheumatology guidelines for management of gout. Part 1: systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis Care Res. 2012;64(10):1431–46. doi: 10.1002/acr.21772.
Khanna D, Khanna PP, Fitzgerald JD et al. 2012 American College of Rheumatology guidelines for management of gout. Part 2: therapy and antiinflammatory prophylaxis of acute gouty arthritis. Arthritis Care Res. 2012;64(10):1447–61. doi: 10.1002/acr.21773.
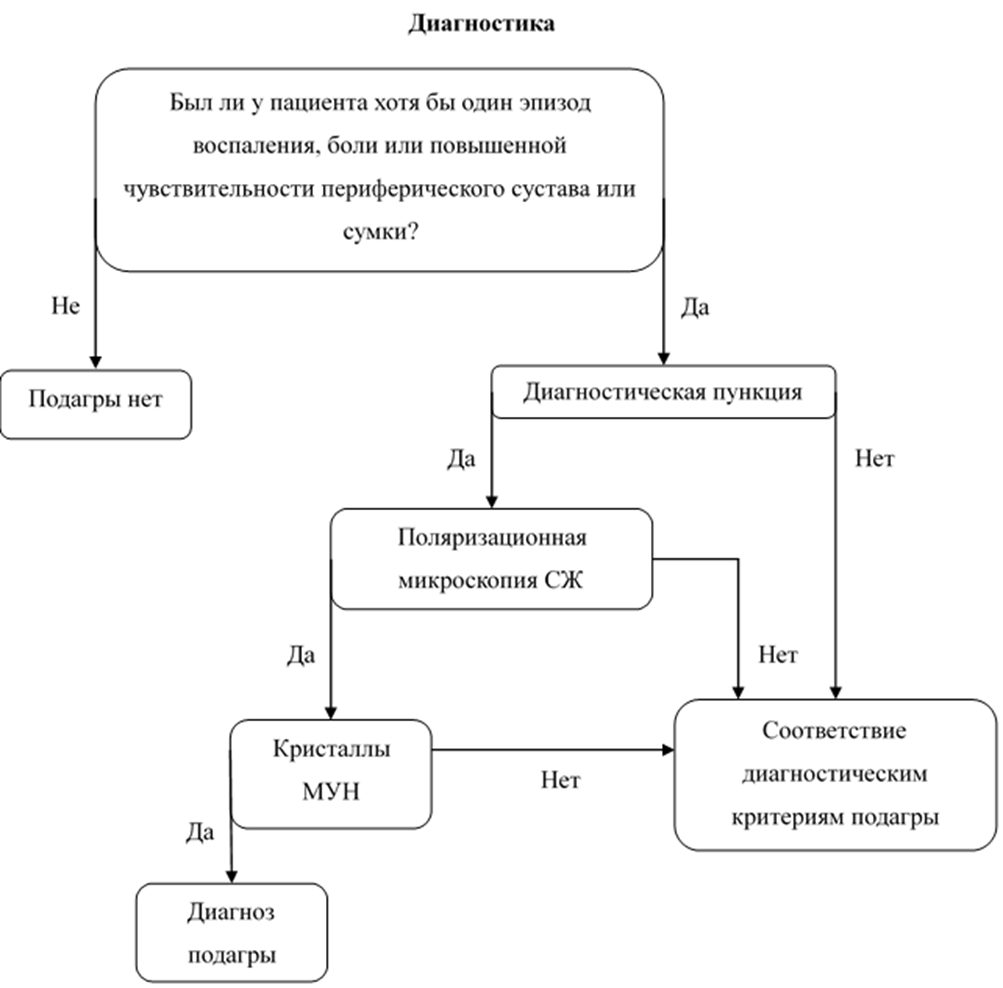 Название подсхемы «Лечение острого артрита» блок-схемы «Алгоритм ведения клинических рекомендациях «Подагра»: 1.2. Алгоритм ведения
Название подсхемы «Лечение острого артрита» блок-схемы «Алгоритм ведения клинических рекомендациях «Подагра»: 1.2. Алгоритм ведения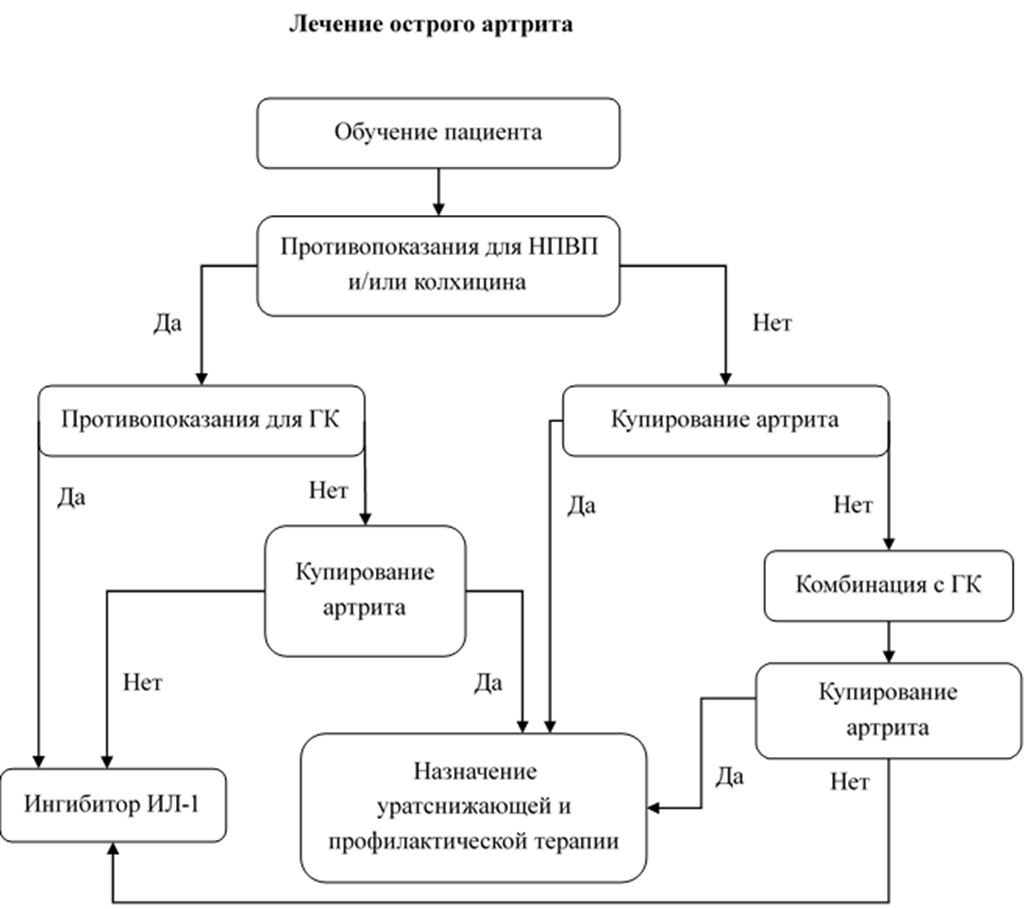 Название подсхемы «Назначение уратснижающей терапии» блок-схемы «Алгоритм ведения клинических рекомендациях «Подагра»: 1.3. Алгоритм ведения
Название подсхемы «Назначение уратснижающей терапии» блок-схемы «Алгоритм ведения клинических рекомендациях «Подагра»: 1.3. Алгоритм ведения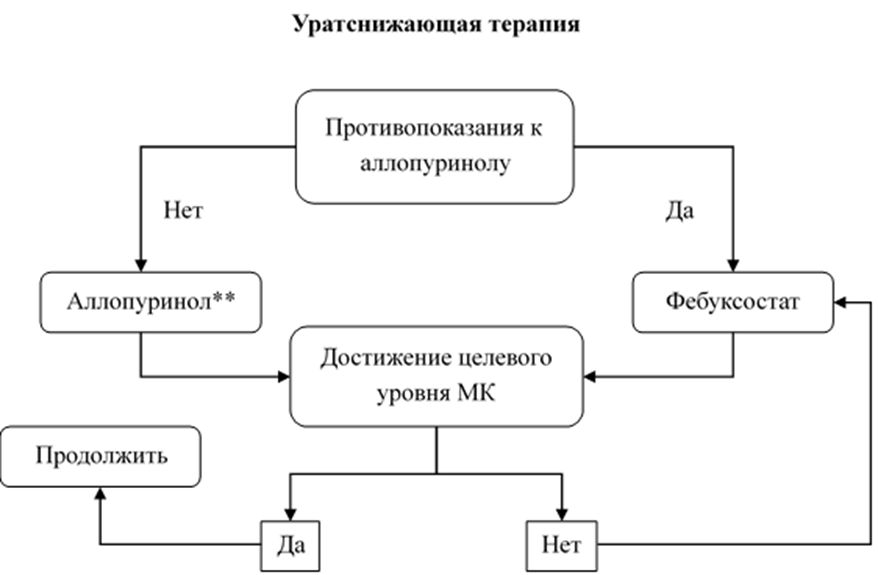
 Ключ (интерпретация):
Ключ (интерпретация):