Dasgupta S, Iannucci G, Mao C, Clabby M, Oster ME. Myocarditis in the pediatric popu-lation: A review // Congenit Heart Dis. - 2019 Sep. -Vol.14 (5). -P. 868-877. doi: 10.1111/chd.12835.
Sagar S, Liu PP, Cooper LT Jr. Myocarditis // Lancet. -2012 Feb. -Vol.379 (9817). -P. 738–747. doi: 10.1016/S0140-6736(11)60648-X
Caforio AL, Pankuweit S, Arbustini E, Basso C, et al. European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases // European Heart Journal. -2013 Sep. -Vol.34 (33). -P. 2636–2648. doi: 10.1093/eurheartj/eht210
Canter CE, Simpson KP. Diagnosis and Treatment of Myocarditis in Children in the Cur-rent Era // Circulation. -2014 Jan. Vol.129(1). -P.115–128.
Tschöpe C, Ammirati E, Bozkurt B, Caforio ALP, et al. Myocarditis and inflammatory cardiomyopathy: current evidence and future directions // Nat Rev Cardiol. -2021 Mar. -Vol.18 (3). -P. 169-193.
Rroku A, Kottwitz J, Heidecker B. Update on myocarditis – what we know so far and where we may be heading // European Heart Journal. Acute Cardiovascular Care. -2021 April. -Vol.10 - Issue 4. -P. 455–467. doi.org/10.1177/2048872620910109
Elamm C, Fairweather D, Cooper LT. Pathogenesis and diagnosis of myocarditis // Heart. -2012. Vol.98. -P. 835–840. doi: 10.1136/heartjnl-2012-301686
Trachtenberg BH, Hare JM. Inflammatory cardiomyopathic syndromes // Circ Res. -2017 -Vol.121. -P. 803–818. doi.org/10.1161/CIRCRESAHA.117.310221
Pollack A, Kontorovich AR, Fuster V, Dec GW. Viral myocarditisdiagnosis, treatment options, and current controversies // Nat Rev Cardiol. -2015. -Vol.12. -P. 670–680. doi: 10.1038/nrcardio.2015.108
Karatolios K, Pankuweit S, Maisch B. Diagnosis and treatment of myocarditis: the role of endomyocardial biopsy // Curr Treat Options Cardiovasc Med. -2007 Dec. -Vol.9 (6). -P. 473-81.
Van Linthout S, Tschöpe C. Viral myocarditis: a prime example for endomyocardial bi-opsy-guided diagnosis and therapy //Curr Opin Cardiol. -2018 May. -Vol.33(3). -P. 325-333. doi: 10.1097/HCO.0000000000000515
Zhang M, Wang H, Tang J, He Y, Xiong T, Li W, Qu Y, Mu D. Clinical characteristics of severe neonatal enterovirus infection: a systematic review // BMC Pediatr. -2021 Mar 15. -Vol. 21 (1). -P. 127. doi: 10.1186/s12887-021-02599-y
Maki S, Aizawa Y, Ito Y, Suda M, Saitoh A. Acute heart failure due to dilated cardio-myopathy exacerbated by systemic parechovirus A1 infection in an infant // Int J Infect Dis. -2021 Mar. -Vol.104. -P. 273-275. doi: 10.1016/j.ijid.2021.01.021
Verdonschot J, Hazebroek M, Merken J, et al. Relevance of cardiac parvovirus B19 in myocarditis and dilated cardiomyopathy: review of the literature // Eur J Heart Fail 2016. -Vol. 18 (12). -P. 1430–1441. doi: 10.1002/ejhf.665
Bejiqi R, Retkoceri R, Maloku A, Mustafa A, et al. The Diagnostic and Clinical Approach to Pediatric Myocarditis: A Review of the Current Literature // Open Access Maced J Med Sci. -2019 Jan 4. -Vol.7(1). -P. 162-173. doi: 10.3889/oamjms.2019.010
Molina KM, Garcia X, Denfield SW, Fan Y, Morrow WR, TowbinJA, Frazier EA, Nelson DP. Parvovirus B19 myocarditis causes significant morbidity and mortality in chil-dren // Pediatr Cardiol. -2013. -Vol.34. -P. 390–397. doi: 10.1007/s00246-012-0468-4
McMurray JC, May JW, Cunningham MW, Jones OY. Multisystem Inflammatory Syndrome in Children (MIS-C), a Post-viral Myocarditis and Systemic Vasculitis-A Critical Review of Its Pathogenesis and Treatment // Front Pediatr. -2020 Dec 16. -Vol.8. -P. 626182. doi: 10.3389/fped.2020.626182
Dhar D, Dey T, Samim MM, Padmanabha H, Chatterjee A, Naznin P, Chandra SR, Mallesh K, Shah R, Siddiqui S, Pratik K, Ameya P, Abhishek G. Systemic inflammatory syndrome in COVID-19-SISCoV study: systematic review and metaanalysis // Pediatr Res. -2021 May. -Vol.18. -P. 1–16.
Bellissima BL, Vara A, Helsby N, Garavan F, Tingle MD. Incidence and investigation of potential risk-factors for clozapine-associated myocarditis and cardiomyopathy in a New Zealand cohort // Psychiatry Res. -2021 May. -Vol.299. -P. 113873. DOI: 10.1016/j.psychres.2021.113873
Curigliano G, Cardinale D, Suter T, Plataniotis G, et al. ESMO Guidelines Working Group. Cardiovascular toxicity induced by chemotherapy, targeted agents and radiother-apy: ESMO Clinical Practice Guidelines // Ann Oncol. -2012 Oct. -23 Suppl 7. -vii155-66. doi: 10.1093/annonc/mds293
Curigliano G, Lenihan D, Fradley M, et al. ESMO Guidelines Committee. Management of cardiac disease in cancer patients throughout oncological treatment: ESMO consensus recommendations // Ann Oncol. -2020 Feb. Vol.31(2). -P. 171-190.
Gauntt C. Coxsackievirus experimental heart diseases // Front. Biosci. -2003. -Vol. 8 (5). -e23-35. Doi: 10.2741/928
Engler R.J.M.et al. A Prospective Study of the Incidence of Myocarditis/Pericarditis and New Onset Cardiac Symptoms following Smallpox and Influenza Vaccination // PLOS ONE / ed. Horwitz M.S. -2015. -Vol.10 (3). -e0118283. doi.org/10.1371/journal.pone.0118283
Mason J.W. Myocarditis and dilated cardiomyopathy: an inflammatory link // Cardiovasc. Res. – 2003. – Vol.60 (1). – P. 5–10. doi: 10.1016/s0008-6363(03)00437-1
Calabrese F., Thiene G. Myocarditis and inflammatory cardiomyopathy: microbiological and molecular biological aspects // Cardiovasc. Res. – 2003. – Vol. 60 (1). – P. 11–25. doi: 10.1016/s0008-6363(03)00475-9
Baggio С, Gagno G, Porcari A .et al. Myocarditis: Which Role for Genetics? // Curr Car-diol Rep. -2021. -Vol.23 (6). -P. 58-63. doi: 10.1007/s11886-021-01492-5
Artico J, Merlo M, Delcaro G, .et al. Lymphocytic myocarditis: a genetically predisposed disease? // J Am Coll Cardiol. -2020. -Vol.75. -P. 3098–3100. doi: 10.1016/j.jacc.2020.04.048
Ammirati E, Frigerio M, Adler ED, et al. Management of Acute Myocarditis and Chronic Inflammatory Cardiomyopathy: An Expert Consensus Document // Circ Heart Fail. -2020 Nov. -Vol. 13(11). -e007405. doi.org/10.1161/CIRCHEARTFAILURE.120.007405
Caforio ALP, Malipiero G, Marcolongo R, Iliceto S. Myocarditis: A Clinical Overview // Curr Cardiol Rep.- 2017. -Vol. 19. -P. 63. doi: 10.1007/s11886-017-0870-x
Chang Y-J, Hsiao H-J, Hsia S-H, et al. Analysis of clinical parameters and echocardiography as predictors of fatal pediatric myocarditis // PLoS ONE. -2019. -Vol.14(3). -e0214087. doi.org/10.1371/journal.pone.0214087
Matsuura H, Ichida F, Saji T, et al. Clinical features of acute and fulminant myocarditis in children // Circ J. – 2016. -Vol.80 (11). -P. 2362–2368. doi: 10.1253/circj.CJ-16-0234
Arola A, Pikkarainen E.et al. Occurrence and Features of Childhood Myocarditis: A Nationwide Study in Finland // J Am Heart Assoc. -2017 Nov. -Vol.6(11). -e005306. doi: 10.1161/JAHA.116.005306
Lipshultz SE, Sleeper LA, Towbin JA, et al. The incidence of pediatric cardiomyopathy in two regions of the United States // N Engl J Med. -2003 Apr. -Vol.348. -P. 1647-1655. DOI: 10.1056/NEJMoa021715
Myocarditis Foundation. Myocarditis in children: incidence, clinical characteristics and outcomes // -Published July 29. 2020. Accessed November 15, 2020. https://www.myocarditisfoundation.org/myocarditis-in-children-incidence-clinical-characteristics-and-outcomes/
Butts RJ, Boyle GJ, Deshpande SR, et al. Characteristics of clinically diagnosed pediatric myocarditis in a contemporary multicenter cohort // Pediatr Cardiol. -2017. -Vol.38(6). -P. 1175–1182. doi: 10.1007/s00246-017-1638-1
Ghelani SJ, Spaeder MC, Pastor W, Spurney CF, Klugman D (2012) Demographics, trends, and outcomes in pediatric acute myocarditis in the United States, 2006 to 2011 // Circ Cardiovasc Qual Outcomes. -2012 Sep. -Vol.5(5). -P. 622–627. doi: 10.1161/CIRCOUTCOMES.112.965749
Klugman D, Berger JT, Sable CA, He J, et al. Pediatric patients hospitalized with myo-carditis: a multiinstitutional analysis // Pediatr Cardiol. -2010. -Vol.31. -P. 222–228. doi: 10.1007/s00246-009-9589-9
Durani Y, Giordano K, Goudie BW. Myocarditis and pericarditis in children // Pediatr Clin North Am. -2010. -Vol.57. -P. 1281-1303.
Neagu O, Rodríguez AF, Callon D, Andréoletti L, Cohen MC. Myocarditis Presenting as Sudden Death in Infants and Children: A Single Centre Analysis by ESGFOR Study Group // Pediatr Dev Pathol. -2021 Apr. -Vol.19. -P. 10935266211007262. doi: 10.1016/j.pcl.2010.09.012
Meyer L, Stubbs B, Fahrenbruch C, Maeda C, et al. Incidence, causes, and survival trends from cardiovascular-related sudden cardiac arrest in children and young adults 0 to 35 years of age: a 30-year review // Circulation. -2012 Sep 11. -Vol.126(11). -P. 1363-72.
Nugent AW, Daubeney PE, Chondros P, et al. National Australian Childhood Cardiomyopathy Study. The epidemiology of childhood cardiomyopathy in Australia // N Engl J Med. -2003 Apr 24. -Vol.348(17). -P. 1639-46. Accessed January 14, 2020. doi: 10.1161/CIRCULATIONAHA.111.076810
Vetter VL, Covington TM, Dugan PN, Haley DM, MPH, Dykstra H, Overpeck M et al. Cardiovascular deaths in children: General overview from the National Center for the Review and Prevention of Child Deaths // Am Heart J. -2015. -Vol.169(3). -P. 426-437.
Lv J, Han B, Wang C, Wang J, Jiang D, Zhao L, Yi Y, Zhang J. The Clinical Features of Children With Acute Fulminant Myocarditis and the Diagnostic and Follow-Up Value of Cardiovascular Magnetic Resonance // Front Pediatr. -2019 Oct. -Vol.7. -P. 388. doi: 10.3389/fped.2019.00388
Winkel BG, Risgaard B, Sadjadieh G, et al. Sudden cardiac death in children (1–18 years): symptoms and causes of death in a nationwide setting // Eur Heart J 2014. -Vol.35. -P. 868–875. doi: 10.1093/eurheartj/eht509
Bohm P, Scharhag J, Meyer T. Data from a nationwide registry on sportsrelated sudden cardiac deaths in Germany // Eur J Prev Cardiol. -2016 Apr. -Vol.23(6). -P. 649-56. doi: 10.1177/2047487315594087
Lieberman EB, Hutchins GM, Herskowitz A, Rose NR, Baughman KL. Clinicopathologic description of myocarditis // J Am Coll Cardiol. -1991 Dec. -Vol.18(7). -P. 1617-26. doi: 10.1016/0735-1097(91)90493-s
Ginsberg F, Parrillo JE. Fulminant myocarditis // Crit Care Clin. -2013. -Vol.29. -P. 465–483. doi: 10.1016/j.ccc.2013.03.004
Sinagra G, Anzini M, Pereira NL, Bussani R, Finocchiaro G, Bartunek J, Merlo M. Myocarditis in Clinical Practice // Mayo Clin Proc. -2016 Sep. -Vol.91(9). -P. 1256-66. doi: 10.1016/j.mayocp.2016.05.013
Abe T, Tsuda E, Miyazaki A, et al. Clinical characteristics and longterm outcome of acute myocarditis in children // Heart Vessels. -2013. -Vol.28(5). -P. 632–8. doi: 10.1007/s00380-012-0296-8
Degener F, Opgen-Rhein B, Bo¨hne M, et al. Four-Year Experience of the German Multicenter Registry for Pediatric Patients with Suspected Myocarditis: MYKKE // In: 50th Annual Meeting of the German Society for Pediatric Cardiology (DGPK). -2018. -Vol 66. Georg Thieme Verlag KG. doi:10.1055/s-0038-1628324
Niu L, An X-J, Tian J, et al. 124 cases of clinical analysis of children with viral myocarditis // Eur Rev Med Pharmacol Sci. -2015. -Vol.19 (15). -P. 2856–9.
Price S, Bodys A, Celinska A, et al. Interlibrary Loan The value of chosen diagnostic tools in evaluating myocarditis in children and adolescents // Pediatr Pol J Paediatr. -2018. -Vol. 93(5). -P. 389–95.
Rodriguez-Gonzalez M, Sanchez-Codez MI, Lubian-Gutierrez M, et al. Clinical presentation and early predictors for poor outcomes in pediatric myocarditis: A retrospective study // World J Clin Cases. -2019. -Vol.7(5). -P. 548–61. doi: 10.12998/wjcc.v7.i5.548
Suthar D, Dodd DA, Godown J. Identifying Noninvasive Tools to Distinguish Acute Myocarditis from Dilated Cardiomyopathy in Children // Pediatr Cardiol. -2018. -Vol.39(6). -P. 1134–8. doi: 10.1007/s00246-018-1867-y
Wu HP, Lin MJ, Yang WC, et al. Predictors of Extracorporeal Membrane Oxygenation Support for Children with Acute Myocarditis // Biomed Res Int. -2017 May. -Vol. 2017. -P. 8. doi.org/10.1155/2017/2510695
Freund MW, Kleinveld G, Krediet TG, et al. Prognosis for neonates with enterovirus myocarditis // Arch Dis Child Fetal Neonatal Ed. -2010 May. -Vol.95(3). -F206–12. doi: 10.1136/adc.2009.165183.
Putschoegl A, Auerbach S. Diagnosis, Evaluation, and Treatment of Myocarditis in Chil-dren // Pediatr Clin N Am. -2020 Oct. -Vol.67 (5). -P. 855–874. doi: 10.1016/j.pcl.2020.06.013
Tunuguntla H, Jeewa A, Denfield SW. Acute Myocarditis and Pericarditis in Children // Pediatr Rev. -2019. -Vol.40(1). -P. 14-25. doi: 10.1542/pir.2018-0044
Levine MC, Klugman D, Teach SJ. Update on myocarditis in children // Curr Opin Pediatr. -2010. -Vol.22. -P. 278–283. doi: 10.1097/MOP.0b013e32833924d2
Freedman SB, Haladyn JK, Floh A, Kirsh JA, Taylor G, Thull-Freedman J. Pediatric my-ocarditis: emergency department clinical findings and diagnostic evaluation // Pediatrics. – 2007. – Vol.120(6). – P. 1278-1285. doi: 10.1542/peds.2007-1073
Schubert S, Opgen-Rhein B, Boehne M, Weigelt A, et al. MYKKE consortium. Severe heart failure and the need for mechanical circulatory support and heart transplantation in pediatric patients with myocarditis: Results from the prospective multicenter registry "MYKKE" // Pediatr Transplant. -2019 Nov. -Vol.23(7). -e13548. doi.org/10.1111/petr.13548
Howard А., Hasan A., Brownlee J., Mehmood N., Ali M., et al. Pediatric Myocarditis Protocol: An Algorithm for Early Identification and Management with Retrospective Analysis for Validation // Pediatric Cardiology. – 2020 Feb. -Vol.41. -P. 316–326. doi: 10.1007/s00246-019-02258-1
Kantor, P. F., Lougheed, J., Dancea, A., et al. Presentation, diagnosis, and medical management of heart failure in children: Canadian cardiovascular society guidelines // Canadian Journal of Cardiology. – 2013. -Vol.29(12). -P. 1535-1552. doi: 10.1016/j.cjca.2013.08.008
Bergmann KR, Kharbanda A, Haveman L Myocarditis and Pericarditis In The Pediatric Patient: Validated Management Strategies // Pediatr Emerg Med Pract. -2015 Jul. -Vol.12(7). -P. 1-22; quiz 23.
Kern J, Modi R, Atalay MK, Kochilas LK. Clinical myocarditis masquerading as acute coronary syndrome // J Pediatr. -2009 Apr. -Vol.154(4). -P. 612-5. doi: 10.1016/j.jpeds.2008.10.018
Cooper LT Jr.Ventricular Arrhythmias and Sudden Cardiac Death in Lymphocytic Myocarditis // J Am Coll Cardiol. -2020 Mar 10. -Vol.75(9). -P. 1058-1060. doi: 10.1016/j.jacc.2020.01.032
Ling N, Li CL, Wang ZZ, Zhang HN, Xu H, An XJ. Heart rate variability in children with myocarditis presenting with ventricular arrhythmias // Eur Rev Med Pharmacol Sci. -2018 Feb. -Vol. 22(4). -P. 1102-1105. doi: 10.26355/eurrev_201802_14397
Школьникова М. А, Алексеева Е.И. Клинические рекомендации по детской кардиологии и ревматологии // М. -2011. – c. 512.
Brady WJ, Ferguson JD, Ullman EA, Perron AD. Myocarditis: emergency department recognition and management // Emerg Med Clin North Am. -2004 Nov. -Vol.22(4). -P. 865-85. doi: 10.1016/j.emc.2004.05.010
Балыкова Л.А., Краснопольская А.В., Власова Е.А. Миокардиты у детей: клиническая картина, диагностика и лечение // Педиатрическая фармакология. -2020. -№17(2). - С. 137-147.
Patel M.S.,Berg A.M., Vincent R.N., Mahle W.T. Serum parameters and echocardiographic predictors of death or need for transplant in newborns, children, and young adults with heart failure // Am J Cardiol. -2010. -Vol.105. -P. 1798-1801. doi: 10.1016/j.amjcard.2010.01.357
Brambatti M, Matassini MV, Adler ED, Klingel K, Camici PG, Ammirati E. Eosinophilic myocarditis: characteristics, treatment, and outcomes // J Am Coll Cardiol. – 2017. -Vol.70. -P. 2363–2375.
Lippi G, Salvagno GL, Guidi GC. Cardiac troponins in pediatric myocarditis // Pediatrics. -2008. -Vol.121(4). -P. 864. doi: 10.1542/peds.2008-0031
Kühl U., Pauschinger M., et.al. High prevalence of viral genomes and multiple viral infections in the myocardium of adults with "idiopathic" left ventricular dysfunction // Circulation. -2005 Feb 22. -Vol.111(7). -P. 887-93. doi.org/10.1161/01.CIR.0000155616.07901.35
Masarone D, Valente F, Rubino M, Vastarella R, et.al. Pediatric Heart Failure: A Practi-cal Guide to Diagnosis and Management // Pediatr Neonatol. -2017 Aug. -Vol. 58(4). -P. 303-312. doi: 10.1016/j.pedneo.2017.01.001
Kirk R, Dipchand AI, Rosenthal DN, et al. The International Society for Heart and Lung Transplantation Guidelines for the management of pediatric heart failure: Executive summary // J Heart Lung Transplant. – 2014. -Vol.33. -P. 888-909. doi: 10.1016/j.healun.2014.06.002
JCS Joint Working Group. Guidelines for diagnosis and treatment of myocarditis (JCS 2009): digest version // Circ. J. Off. J. Jpn. Circ. Soc. -2011. -Vol.75 (3). -P. 734–743. doi: 10.1253/circj.cj-88-0008
McNamara D M. Heart Failure as a Consequence of Viral and Nonviral Myocarditis Heart Failure: A Companion to Braunwald's Heart Disease // Elsevier. -2020. -Vol.28. -P. 376-384.e3
Vigneswaran TV, Brown JR, Breuer J, Burch M. Parvovirus B19 myocarditis in children: an observational study // Arch Dis Child. -2016 Feb. -Vol.101(2). -P. 177-80. doi: 10.1136/archdischild-2014-308080
Tuthar D, Dodd DA, Godown J. Identifying Non-invasive Tools to Distinguish Acute Myocarditis from Dilated Cardiomyopathy in Children // PediatrCardiol. -2018.-Vol. 39(6). -P. 1134–8.
Foerster SR, Canter CE, Cinar A, et al Ventricular remodeling and survival are more favorable for myocarditis than for idiopathic dilated cardiomyopathy in childhood // Circ Heart Fail. – 2010. -Vol.3. -P. 689–697. doi: 10.1161/CIRCHEARTFAILURE.109.902833
Felker GM, Boehmer JP, Hruban RH et al Echocardiographic fndings in fulminant and acute myocarditis // J Am Coll Cardiol. -2000. -Vol. 36(1). -P. 227-32. doi: 10.1016/s0735-1097(00)00690-2.
Gursu HA, Cetin AE, Kibar AE, et al The assessment of treatment outcomes in patients with acute viral myocarditis by speckle tracking and tissue Doppler methods // Echocardiography. -2019. -Vol.36. -P. 1666–1674. doi: 10.1111/echo.14449.
Wisotzkey BL, Soriano, BD, Albers, EL, et al Diagnostic role of strain imaging in atypical myocarditis by echocardiography and cardiac MRI // Pediatr Radiol. -2018. -Vol.48. -P.835–842. doi: 10.1007/s00247-017-4061-0
Khoo NS, Smallhorn, JF, Atallah, J, et al Altered left ventricular tissue velocities, deformation and twist in children and young adults with acute myocarditis and normal ejection fraction // J Am Soc Echocardiogr. -2012. -Vol.25. -P. 294–303. doi: 10.1016/j.echo.2011.10.010
Banka P, Robinson JD, Uppu SC, Harris MA, et al. Cardiovascular magnetic resonance techniques and findings in children with myocarditis: a multicenter retrospective study // Journal of cardiovascular magnetic resonance: official journal of the Society for Cardiovascular Magnetic Resonance. -2015. -Vol.17. -P. 96. doi: 10.1186/s12968-015-0201-6.
Friedrich MG, Sechtem U, Schulz-Menger J, et al.; International Consensus Group on Cardiovascular Magnetic Resonance in Myocarditis. Cardiovascular magnetic resonance in myocarditis: a JACC white paper // J Am Coll Cardiol. -2009. -Vol.53. -P. 1475–1487. doi: 10.1016/j.jacc.2009.02.007
Pan JA, Lee YJ, Salerno M. Diagnostic performance of extracellular volume, native T1, and T2 mapping versus lake louise criteria by cardiac magnetic resonance for detection of acute myocarditis: a meta-analysis // Circ Cardiovasc Imaging. -2018. -Vol.11. -e007598. doi: 10.1161/CIRCIMAGING.118.007598
Wei S, Fu J, Chen L, Yu S. Performance of Cardiac Magnetic Resonance Imaging for Diagnosis of Myocarditis Compared with Endomyocardial Biopsy: A Meta-Analysis // Med Sci Monit. -2017. -Vol.23. -P. 3687-3696. doi: 10.12659/msm.902155
Kotanidis CP, Bazmpani MA, Haidich AB, Karvounis C, Antoniades C, Karamitsos TD. Diagnostic accuracy of cardiovascular magnetic resonance in acute myocarditis: A Sys-tematic Review and Meta-Analysis // J Am Coll Cardiol Img. -2018. -Vol.11(11). -P. 1583–90. doi: 10.1016/j.jcmg.2017.12.008
Ferreira VM, Schulz-Menger J, Holmvang G, Kramer CM, Carbone I, Sechtem U, Kin-dermann I, Gutberlet M, Cooper LT, Liu P, et al. Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations // J Am Coll Cardiol. -2018. -Vol.72. -P. 3158–3176.
Messroghli DR, Moon JC, Ferreira VM, Grosse-Wortmann L, He T, Kellman P, et al. Clinical recommendations for cardiovascular magnetic resonance mapping of T1, T2, T2* and extracellular volume: a consensus statement by the Society for Cardiovascular Mag-netic Resonance (SCMR) endorsed by the European Association for Cardiovascular Im-aging (EACVI) // J Cardiovasc Magn Reson. -2017. -Vol.19(1). -P. 75.
Cornicelli M.D., Rigsby, C.K., Rychlik, K. et al. Diagnostic performance of cardiovascular magnetic resonance native T1 and T2 mapping in pediatric patients with acute myo-carditis // J Cardiovasc Magn Reson. -2019. -Vol.21 (1). -P. 40. doi: 10.1186/s12968-019-0550-7
Luetkens JA, Faron A, Isaak A, Dabir D, Kuetting D, et al. Comparison of original and 2018 lake louise criteria for diagnosis of acute myocarditis: results of a validation cohort // Radiology: Cardiothoracic Imaging. -2019. -Vol.1. -e190010. doi.org/10.1148/ryct.2019190010
Francone M, et al. CMR sensitivity varies with clinical presentation and extent of cell ne-crosis in biopsyproven acute myocarditis // JACC Cardiovasc. Imaging. -2014. -Vol.7. -P. 254–263. doi: 10.1016/j.jcmg.2013.10.011
Małek ŁA, Kamińska H, Barczuk-Falęcka M, et al. Children With Acute Myocarditis Often Have Persistent Subclinical Changes as Revealed by Cardiac Magnetic Resonance // J Magn Reson Imaging. -2020 Aug. -Vol.52(2). -P. 488-496.
Aquaro GD, Ghebru Habtemicael Y, Camastra G, Monti L, Dellegrottaglie S, Moro C, Lanzillo C, Scatteia A, Di Roma M, Pontone G, et al.; “Cardiac Magnetic Resonance” Working Group of the Italian Society of Cardiology. Prognostic value of repeating cardi-ac magnetic resonance in patients with acute myocarditis // J Am Coll Cardiol. -2019. -Vol.74. -P. 2439–2448.
Gräni C, Eichhorn C, Bière L, Murthy VL, Agarwal V, Kaneko K, Cuddy S, Aghayev A, Steigner M, Blankstein R, et al. Prognostic value of cardiac magnetic resonance tissue characterization in risk stratifying patients with suspected myocarditis // J Am Coll Cardi-ol. -2017. -Vol.70. -P. 1964–1976. DOI: 10.1016/j.jacc.2017.08.050
Berg J, et al. Cardiac magnetic resonance imaging in myocarditis reveals persistent disease activity despite normalization of cardiac enzymes and inflammatory parameters at 3-month follow-up //Circ. Heart. -2017. -Vol.10. -e004262. doi: 10.1161/CIRCHEARTFAILURE.117.004262
Rangamani S, Varghese J, Li L, Harvey L, et al. Safety of cardiac magnetic resonance and contrast angiography for neonates and small infants: a 10-year single-institution experience // Pediatr Radiol. -2012 Nov. -Vol.42(11). -P. 1339-46. DOI:10.1007/s00247-012-2452-9
Jain R, Petrillo-Albarano T, Parks WJ,. et al. Efficacy and safety of deep sedation by nonanesthesiologists for cardiac MRI in children // Pediatr Radiol. -2013 Mar. -Vol.43(5). -P. 605-11. doi: 10.1007/s00247-012-2566-0
Schmitz A, Weiss M, Kellenberger C, O'Gorman Tuura R, et al. Sedation for mag-netic resonance imaging using propofol with or without ketamine at induction in pediat-rics-A prospective randomized double-blinded study // Paediatr Anaesth. -2018 Mar. -Vol.28(3). -P. 264-274. doi: 10.1111/pan.13315
Bussani R, Silvestri F, Perkan A, et al. Endomyocardial Biopsy. 2019 May 18. In: Sinagra G, Merlo M, Pinamonti B, editors. Dilated Cardiomyopathy: From Genetics to Clinical Management [Internet] //. Cham (CH): Springer. -2019. -Chapter 9.
Katzmann JL, Schlattmann P, Rigopoulos AG, et al Metaanalysis on the im-munohistological detection of inflammatory cardiomyopathy in endomyocardial biopsies // Heart Fail Rev. -2020 Mar. -Vol.25(2). -P. 277-294. doi: 10.1007/s10741-019-09835-9
Baughman KL. Diagnosis of myocarditis: death of Dallas criteria // Circulation. -2006 Jan 31. -Vol.113(4). -P. 593-5. doi.org/10.1161/CIRCULATIONAHA.105.589663
Cooper LT, Baughman KL, Feldman AM, et al American Heart Association; American College of Cardiology; European Society of Cardiology; Heart Failure Society of America; Heart Failure Association of the European Society of Cardiology. The role of endomyocardial biopsy in the management of cardiovascular disease: a scientific state-ment from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology. Endorsed by the Heart Failure Society of America and the Heart Failure Association of the European Society of Cardiology // J Am Coll Cardi-ol. -2007 Nov 6. -Vol.50(19). -P. 1914-31. doi: 10.1016/j.jacc.2007.09.008
Bowles N.E., Ni J., Kearney D.L., et al. Detection of viruses in myocardial tissues by polymerase chain reaction: evidence of adenovirus as a common cause of myocarditis in children and adults // J Am Coll Cardiol. -2003. -Vol.42. -P. 466-472. doi: 10.1016/s0735-1097(03)00648-x.
Ponikowski P, Voors A, Anker S, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treat-ment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC // Eur Heart J. -2016 Jul 14. -Vol.37(27). -P. 2129-2200. doi.org/10.1093/eurheartj/ehw128
Ahmed H, VanderPluym C. Medical management of pediatric heart failure // Car-diovasc Diagn Ther. -2021. -Vol.11(1). -P.323-335. doi: 10.21037/cdt-20-358
Das BB. Current State of Pediatric Heart Failure // Children (Basel). -2018. -Vol.5(7). -P.88. doi: 10.3390/children5070088
Laghlam D, Benghanem S, Ortuno S, et al. Management of cardiogenic shock: a narrative review. // Ann Intensive Care. – 2024. -Vol.14(1). -P.45. doi: 10.1186/s13613-024-01260-y
Wooldridge G, Hitayezu J, Venkatasubbu P. Paediatric cardiogenic shock. // Up-date in Anaesthesia. -2021 doi: 10.1029/WFSA-D-19-00022
Koentartiwi D, Candini N, Suwarnianty R. Management of cardiogenic shock in pediatric patients. // Islamic Health Journal. -2020. -Vol.9 (2) -P. 60-82. doi:10.33474/jki.v9i2.8891
Rossano JW, Kim JJ, Decker JA, et al. Prevalence, morbidity, and mortality of heart failurerelated hospitalizations in children in the United States: a population-based study // J Card Fail. -2012. -Vol.18. -P. 459-70. doi: 10.1016/j.cardfail.2012.03.001
Chioncel O, Parissis J, Mebazaa A, Thiele H et al. Epidemiology, pathophysiology and contemporary management of cardiogenic shock - a position statement from the Heart Failure Association of the European Society of Cardiology // Eur J Heart Fail. -2020 Aug. -Vol.22(8). P. 1315-1341. doi: 10.1002/ejhf.1922
Law YM, Lal AK, Chen S, Čiháková D et al. American Heart Association Pediatric Heart Failure and Transplantation Committee of the Council on Lifelong Congenital Heart Disease and Heart Health in the Young and Stroke Council. Diagnosis and Man-agement of Myocarditis in Children: A Scientific Statement From the American Heart Association // Circulation. -2021 Aug 10. -Vol.144(6). -e123-135. doi: 10.1161/CIR.0000000000001001
Caviedes B P, et al. Dilated cardiomyopathy and severe heart failure. An update for pediatricians // Arch Argent Pediatr. - 2018 Jun 1. -Vol.116(3). -e421-428. doi: 10.5546/aap.2018.eng.e421.
Miller TL, Neri D, Extein J, Somarriba G, Strickman-Stein N. Nutrition in Pediat-ric Cardiomyopathy // Prog Pediatr Cardiol. -2007. -Vol. 24(1). P. 59-71. doi: 10.1016/j.ppedcard.2007.08.007
Лазарев В.В. Особенности детского организма / В.В. Лазарев // Интенсивная терапия: Национальное руководство / под ред. Б.Р. Гельфанда, А.И. Салтанова. -Москва: ГЭОТАРМедиа, 2009. -С. 490-505
Matsumori A, Igata H, Ono K, Iwasaki A, Miyamoto T, Nishio R, Sasayama S. High doses of digitalis increase the myocardial production of proinflammatory cytokines and worsen myocardial injury in viral myocarditis: a possible mechanism of digitalis toxicity // Jpn Circ J. -1999. -Vol.63. -P. 934–940.2 doi: 10.1253/jcj.63.934
Савенкова М.C., Вашура Л.В., Абдулаев А.К., Анджель А.Е., Балакирева Г.М., Румянцева И.Г., Кузнецова Е.С. Значение герпесвирусных инфекций у детей // Педиатрия. Журнал им. Г. Н. Сперанского. -2016. -№2. -С. 134-141
Pinninti SG, Kimberlin DW. Preventing herpes simplex virus in the newborn // Clin Perinatol. -2014 Dec. -Vol.41(4). -P. 945-55. doi: 10.1016/j.clp.2014.08.012.
120 Harris JB, Holmes AP. Neonatal Herpes Simplex Viral Infections and Acy-clovir: An Update // J Pediatr Pharmacol Ther. -2017. -Vol.22(2). -P. 88-93. doi: 10.5863/1551-6776-22.2.88.
Васичкина Е.С., Балыкова Л.А., Басаргина Е.Н., Брегель Л.В., Дегтярева Е.А., Ковалев И.А., Котлукова Н.П., Леонтьева И.В., Яковлева Л.В., Грознова О.С. Миокардиты у детей. Современные подходы к лечению и реабилитации. // Вопросы практической педиатрии. - 2024; -№19(6). -С. 110–122. doi: 10.20953/1817-7646-2024-6-110-122
Lim Y, Lyall H. Congenital cytomegalovirus - who, when, what-with and why to treat? // J Infect. -2017 Jun. -74 Suppl 1. -S89-S94. doi: 10.1016/S0163-4453(17)30197-4
122 Luck SE, Wieringa JW, Blázquez-Gamero D, Henneke P, et al. ACTM; ES-PID Congenital CMV Group Meeting, Leipzig 2015. Congenital Cytomegalovirus: A Eu-ropean Expert Consensus Statement on Diagnosis and Management // Pediatr Infect Dis J. -2017 Dec. -Vol.36(12). -P. 1205-1213. doi: 10.1097/INF.0000000000001763.
Rawlinson WD, Boppana SB, Fowler KB, Kimberlin DWet al.Congenital cytomegalovirus infection in pregnancy and the neonate: consensus recommendations for prevention, diagnosis, and therapy // Lancet Infect Dis. -2017 Jun. -Vol.17(6). -e177-188. doi: 10.1016/S1473-3099(17)30143-3
Maisch B, Pankuweit S. Current treatment options in (peri)myocarditis and inflammatory cardiomyopathy // Herz. -2012. -Vol.37. -P. 644–656. doi: 10.1007/s00059-012-3679-9.
Понежева Ж.Б., Гришаева А.А., Попова Т.И. Клинические формы вирусной инфекции Эпштейна — Барр // РМЖ. -2019. -№10. -C.36-41.
Шестакова И.В. Лечить или не лечить Эпштейна-Барр вирусную инфекцию: подробный обзор различных тактик // Инфекционные болезни: Новости. Мнения. Обучение. -2013. -№3 (4). -С. 12-23
Никитина И.Л., Вершинина Т.Л. Миокардит у детей: проблемы и решения. // Медицинский Совет. -2017. -№1ю -С. 238-245. doi:10.21518/2079-701X-2017-1-238-245
Dennert R, Velthuis S, Schalla S, et al. Intravenous immunoglobulin therapy for patients with idiopathic cardiomyopathy and endomyocardial biopsy-proven high PVB19 viral load //Antivir Ther. -2010. -Vol.15 (2). -P. 193–201. doi: 10.3851/IMP1516
Чернова Т.М., Тимченко В.Н., Павлова Е.Б., Баракина Е.В., Субботина М.Д. Парвовирусная В19 инфекция: Лекция // Детские инфекции. -2022. -№3. -С. 39-46
Kuhl U., Lassner D., von Schlippenbach J., et al. Interferon- beta improves sur-vival in enterovirus- associated cardiomyopathy // J. Am.Coll. Cardiol. -2012. – Vol.60. -P. 1295–1296. doi: 10.1016/j.jacc.2012.06.026
Schultheiss HP. et al. Betaferon in chronic viral cardiomyopathy (BICC) trial: ef-fects of interferon- β treatment in patients with chronic viral cardiomyopathy // Clin. Res. Cardiol. -2016. -Vol. 105. -P. 763–773. doi: 10.1007/s00392-016-0986-9
Costanzo-Nordin MR, Reap EA, O’Connell JB, Robinson JA, Scanlon PJ. A non-steroid antiinflammatory drug exacerbates Coxsackie B3 murine myocarditis // J Am Coll Cardiol. -1985. -Vol.6. -P. 1078–1082. doi: 10.1016/s0735-1097(85)80312-0
Khatib R, Reyes MP, Smith F, Khatib G, Rezkalla S. Enhancement of coxsackievirus B4 virulence by indomethacin // J Lab Clin Med. -1990. -Vol.116. -P. 662–670.
Lin MS., Tseng YH., Chen MY. et al. Inhospital and postdischarge outcomes of pediatric acute myocarditis underwent after highdose steroid or intravenous immuno-globulin therapy // BMC Cardiovasc Disorders 19. -2019.
Prasad AN, Chaudhary S. Intravenous immunoglobulin in children with acute my-ocarditis and/or early dilated cardiomyopathy // Indian Pediatr. -2014. -Vol.51(7). -P. 583–4. doi: 10.1007/s13312-014-0456-2
Kim HS, Sohn S, Park JY, Seo JW. Fulminant myocarditis successfully treated with high dose immunoglobulin // Int J Cardiol. -2004. -Vol.96(3). -P. 485–6. doi: 10.1016/j.ijcard.2003.05.037
Tsai YG, Ou TY, Wang CC, Tsai MC et.al. Intravenous gammaglobulin therapy in myocarditis complicated with complete heart block: report of one case // Acta Paediatr Taiwan. -2001. -Vol.42(5). -P. 311–3.
Xin Huang, Yufei Sun, Guanhua Su, Yu Li, Xinxin Shuai, Intravenous Immunoglobulin Therapy for Acute Myocarditis in Children and Adults // International Heart Journal. -2019. -Vol. 60 (2). -P. 359-365. doi: 10.1536/ihj.18-299
Drucker NA, Colan SD, Lewis AB, Beiser AS, Wessel DL, Takahashi M, Baker AL, Perez-Atayde AR, Newburger JW. Gamma-globulin treatment of acute myocarditis in the pediatric population // Circulation. -1994. -Vol.89. -P. 252–257.
Maisch B, Hufnagel G, Kölsch S, Funck R, Richter A, Rupp H, Herzum M, Pankuweit S. Treatment of inflammatory dilated cardiomyopathy and (peri)myocarditis with immunosuppression and i.v. immunoglobulins // Herz. -2004 Sep. -Vol.29(6). -P. 624-36.
Chan KY, Iwahara M, Benson LN, Wilson GJ, Freedom RM. Immunosuppressive therapy in the management of acute myocarditis in children: a clinical trial // J Am Coll Cardiol. -1991. -Vol.17(2). -P. 458–60. doi: 10.1016/s0735-1097(10)80115-9
Kleinert S, Weintraub RG, Wilkinson JL, Chow CW. Myocarditis in children with dilated cardiomyopathy: incidence and outcome after dual therapy immunosuppression // J Heart Lung Transplant. -1997. -Vol.16(12). -P. 1248–54.
Mason JW, O'Connell JB, Herskowitz A, Rose NR, McManus BM, Billingham ME. Moon TE. A clinical trial of immunosuppressive therapy for myocarditis. The myocarditis treatment trial investigators // N Engl J Med. -1995. -Vol.333(5). -P. 269–75. doi: 10.1056/NEJM199508033330501
Camargo PR, Snitcowsky R, da Luz PL, Mazzieri R, Higuchi ML, Rati M, Stolf N, Ebaid M, Pileggi F. Favorable effects of immunosuppressive therapy in children with dilated cardiomyopathy and active myocarditis // Pediatr Cardiol. -1995. -Vol.16(2). -P. 61–8. doi: 10.1007/BF00796819
Aziz KU, Patel N, Sadullah T, Tasneem H, Thawerani H, Talpur S. Acute viral myocarditis: role of immunosuppression: a prospective randomised study // Cardiol Young. -2010 Oct. -Vol.20(5). -P. 509-15.
Hia CP, Yip WC, Tai BC, Quek SC. Immunosuppressive therapy in acute myocarditis: an 18 year systematic review // Arch Dis Child. -2004. -Vol.89(6). -P. 580–4. doi: 10.1136/adc.2003.034686
Lu C, Qin F, Yan Y, Liu T, Li J, Chen H. Immunosuppressive treatment for myocarditis: a metaanalysis of randomized controlled trials // J Cardiovasc Med (Hager-stown). -2016. -Vol.17(8). -P. 631.
Chen HS, Wang W, Wu SN, Liu JP. Corticosteroids for viral myocarditis // Cochrane Database Syst Rev.- 2013. -Vol.2013 (10). doi: 10.1002/14651858.CD004471.pub3
Herda L.R. et al. Effects of immunoadsorption and subsequent immunoglobulin G substitution on cardiopulmonary exercise capacity in patients with dilated cardiomyopa-thy//Am. Heart J. -2010. -Vol.159(5). -P. 809-816. doi: 10.1016/j.ahj.2010.01.012
Bulut D. et al. Effect of protein A immunoadsorption on T cell activation in patients with inflammatory dilated cardiomyopathy // Clin. Res. Cardiol. Off. J. Ger. Card. Soc. -2010. -Vol.99(10). -P. 633-638. doi: 10.1007/s00392-010-0162-6
Maron BJ. et al. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Task Force 3: Hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy and other cardiomyopathies, and myocarditis: a scientific statement from the American Heart Association and American Col-lege of Cardiology // Circulation. -2015. -Vol.132 (22). -e.273-80. doi: 10.1161/CIR.0000000000000239
Bozkurt B. et al. Current diagnostic and treatment strategies for specific dilated cardiomyopathies: a scientific statement from the American Heart Association // Circula-tion. -2016. -Vol.134. -e579–646. doi.org/10.1161/CIR.0000000000000455
Леонтьева И.В. Современная стратегия лечения миокардитов у детей // Российский вестник перинатологии и педиатрии. -2022. -№67(1). -С.:28-38. doi: 10.21508/1027-4065-2022-67-1-28-38
Zeppenfeld К, Tfelt-Hansen J, de Riva M, et al. ESC Scientific Document Group , 2022 ESC Guidelines for the management of patients with ventricular arrhythmi-as and the prevention of sudden cardiac death: Developed by the task force for the man-agement of patients with ventricular arrhythmias and the prevention of sudden cardiac death of the European Society of Cardiology (ESC) Endorsed by the Association for Eu-ropean Paediatric and Congenital Cardiology (AEPC) // European Heart Journal. -2022. -Vol.43(40). -P. 3997–4126. doi:10.1093/eurheartj/ehac262
Brugada J, Blom N, Sarquella-Brugada G et al. Pharmacological and nonpharmacological therapy for arrhythmias in the pediatric population: EHRA and AEPC-Arrhythmia Working Group joint consensus statement. //EP Europace. -2013. -Vol.15(9). -P. 1337–1382. doi:10.1093/europace/eut082
Rizzo C, Carbonara R, Ruggieri R, Passantino A, Scrutinio D. Iron Deficiency: A New Target for Patients With Heart Failure // Front Cardiovasc Med. -2021. Vol. 8; 709872. -e1-10. doi: 10.3389/fcvm.2021.709872
Peretto G, Sala S, Camaschella C. Iron deficiency in chronic myocarditis: Assess-ment and prognostic significance. // Eur J Intern Med. – 2021. Vol 89. -P. 129-131. doi: 10.1016/j.ejim.2021.03.037.
Ogunbayo GO, Elayi SC, Ha LD, Olorunfemi O, Elbadawi A, Saheed D,Sorrell VL. Outcomes of heart block in myocarditis: a review of 31,760 patients // Heart Lung Circ. -2019. -Vol. 28. -P. 272–276. doi: 10.1016/j.hlc.2017.12.005
Li TT, Cheng J. Clinical analysis of temporary pacemaker implantation in 13 chil-dren. // Transl Pediatr. – 2022. -Vol 11(2). -P. 174-182. doi: 10.21037/tp-21-586
Batra AS, Epstein D, Silka MJ. The clinical course of acquired complete heart block in children with acute myocarditis. // Pediatr Cardiol. -2003. -Vol. 24(5). -P. 495-497. doi: 10.1007/s00246-002-0402-2
Gagliardi MG, Fierabracci A, Pilati M, et al. The impact of specific viruses on clin-ical outcome in children presenting with acute heart failure // Int J Mol Sci. – 2016. -Vol. 17(4). -P. 1–10. doi: 10.3390/ijms17040486
Kirk R, Naftel D, Hoffman TM, et al. Outcome of pediatric patients with dilated cardiomyopathy listed for transplant: a multi-institutional study // J Heart Lung Transpl. – 2009 Dec. -Vol.28 (12). -P. 1322-8. doi: 10.1016/j.healun.2009.05.027
Pietra BA, Kantor PF, Bartlett HL, et al. Early predictors of survival to and after heart transplantation in children with dilated cardiomyopathy // Circulation. -2012 Aug 28. -Vol. 126 (9). -P. 1079-86. doi: 10.1161/CIRCULATIONAHA.110.011999
Tikkanen AU, Berry E, LeCount E et al. Rehabilitation in Pediatric Heart Failure and Heart Transplant. // Front Pediatr. – 2021. -Vol. 9; 674156. doi: 10.3389/fped.2021.674156.
World Health Organization. International Classification of Functioning, Disability and Health: ICF. Geneva: WHO, 2001. — P. 3-29.
Piepoli MF, Conraads V, Corra` U. et al. Exercise training in heart failure: from theory to practice. A consensus document of the Heart Failure Association and the European Association for Cardiovascular Prevention and Rehabilitation // Eur. J. Heart. Fail. – 2011. – Nо. 13. – Р. 347–357.
Paridon SM, Alpert BS, Alpert BS. Clinical stress testing in the pediatric age group: a statement from the American Heart Association council on cardiovascular dis-ease in the young, committee on atherosclerosis, hypertension, and obesity in youth. Circulation. -2006. - Vol. 113(15). P. 1905–1920.
Giannitsi S, Bougiakli M, Bechlioulis A, et al. 6-minute walking test: a useful tool in the management of heart failure patients. // Ther Adv Cardiovasc Dis. -2019. -Vol. 13:1753944719870084. doi: 10.1177/1753944719870084.
McBride MG, Burstein DS, Edelson JB, Paridon SM. Cardiopulmonary Rehabilitation in Pediatric Patients With Congenital and Acquired Heart Disease. J Cardiopulm Rehabil Prev. - 2020. - Vol. 40(6). - P. 370-377. doi: 10.1097/HCR.0000000000000560.
Davies E.J. et al. Exercise training for systolic heart failure: Cochrane systematic review and meta-analysis // Eur. J. Heart Fail. -2010. -Vol.12(7). -P. 706–715. doi: 10.1093/eurjhf/hfq056
Ribeiro J.P., Chiappa G.R., Callegaro C.C. The contribution of inspiratory muscles function to exercise limitation in heart failure: pathophysiological mechanisms // Rev. Bras. Fisioter. Sao Carlos Sao Paulo Braz. -2012. -Vol.16(4). -P. 261–267. doi.org/10.1590/S1413-35552012005000034
Pandey A. et al. Exercise training in patients with heart failure and preserved ejec-tion fraction: metaanalysis of randomized control trials // Circ. Heart Fail. -2015 Jan. -Vol. 8 (1). – P. 33–40. doi: 10.1161/CIRCHEARTFAILURE.114.001615
Батышева Т.Т., Медико-психологическая помощь детям с нарушением психического развития в системе комплексной реабилитации // Методические рекомендации, г. Москва. -2018. -C. 5-568.
Таточенко В.К., Н.А. Озерецковский. Иммунопрофилактика-2020: справочник, 13-е издание, расширенное // Москва: Боргес. -2020. – C. 16 — 23.
Басаргина Е.Н., Миокардит у детей: трудности диагностики и лечения // журнал «Педиатрия». -г. Москва -2015. – N.94(2). - С.158- 160.
Басаргина Е.Н. Сердечная недостаточность. В кн.: М.А. Школьникова, Е.И. Алексеева, ред. Клинические рекомендации по детской кардиологии и ревматологии // М.: «ООО М-Арт». -2011. -C. 242–276.
Mirabel M. et al. Outcomes, longterm quality of life, and psychologic assessment of fulminant myocarditis patients rescued by mechanical circulatory support // Crit. Care Med. -2011. -Vol. 39 (5). -P. 1029–1035. doi: 10.1097/CCM.0b013e31820ead45
Hsu K.-H. et al. Extracorporeal membranous oxygenation support for acute fulminant myocarditis: analysis of a single center’s experience // Eur. J. Cardio-Thorac. Surg. Off. J. Eur. Assoc. Cardio-Thorac. Surg. – 2011. -Vol. 40 (3). - P. 682–688. doi: 10.1016/j.ejcts.2010.12.050
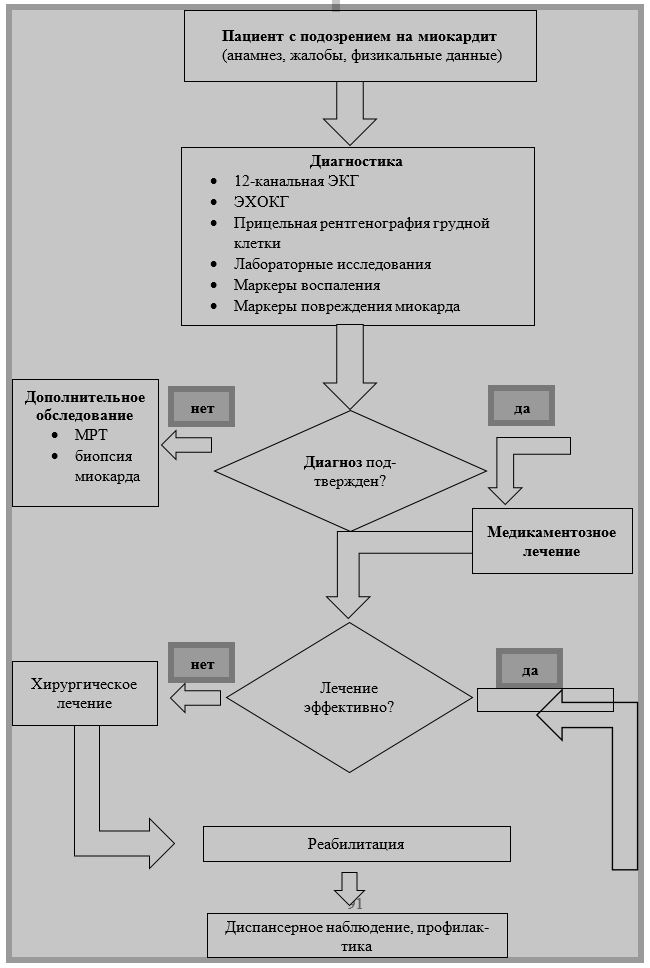
 Приложение Б2. Алгоритм ранней диагностики и ведения миокардита у детей
Приложение Б2. Алгоритм ранней диагностики и ведения миокардита у детей