Schwartz B, Facklam RR, Breiman RF. Changing epidemiology of group A streptococcal infection in the USA. Lancet 1990; 336:1167–71.
Bisno AL., Group A streptococcal infections and acute rheumatic fever. N Engl J 1991; 325:783–93.
No authors, Stroke Prevention in Atrial Fibrillation Study: final results. Circulation 1991; 84:527–39.
Carroll JD, Feldman T. Percutaneous mitral balloon valvotomy andthe new demographics of mitral stenosis. JAMA 1993; 270:1731–6.
Manning WJ, Silverman DI, Keighley CS, Oettgen P, Douglas PS.Transesophageal echocardiographically facilitated early cardioversionfrom atrial fibrillation using short-term anticoagulation: finalresults of a prospective 4.5-year study. J Am Coll Cardio. 1995; 25:1354–61.
Tuzcu EM, Block PC, Griffin BP, Newell JB, Palacios IF. Immediateand longterm outcome of percutaneous mitral valvotomy inpatients 65 years and older. Circulation 1992; 85:963–71.
Nishimura R.A., Rihal CS, Tajik AJ, Holmes DR Jr. Accurate measurement of the transmitral gradient in patients with mitralstenosis: a simultaneous catheterization and Doppler echocardiographicstudy. J Am Coll Cardiol 1994; 24:152–8.
Cohen DJ, Kuntz RE, Gordon SP, et al. Predictors of long-termoutcome after percutaneous balloon mitral valvuloplasty. N EnglJ Med 1992; 327:1329–35.
Snopek G, Pogorzelska H, Rywik TM, Browarek A, Janas J,Korewicki J. Usefulness of endothelin-1 concentration in capillaryblood in patients with mitral stenosis as a predictor of regression ofpulmonary hypertension after mitral valve replacement or,» or valvuloplasty. Am J Cardiol 2002;90:188–9.
Gordon SP, Douglas PS, Come PC, Manning WJ. Two dimensionaland Doppler echocardiographic determinants of thenatural history of mitral valve narrowing in patients with rheumaticmitral stenosis: implications for follow-up. J Am Coll Cardiol 1992; 19:, 968-73.
Flachskampf FA, Weyman AE, Guerrero JL, Thomas JD. Influenceof orifice geometry and flow rate on effective valve area: an invitro study. J Am Coll Cardiol 1990;15:1173–80.
Tamai J, Nagata S, Akaike M, et al. Improvement in mitral flowdynamics during exercise after percutaneous transvenous mitralcommissurotomy: noninvasive evaluation using continuous waveDoppler technique. Circulation 1990;81:46–51.
Guilherme L. Molecular mimicry in the autoimmune pathogenesis of rheumatic heart disease / L. Guilherme, J. Kalil, M. Cunningham // Autoimmunity. – 2006. – Vol. 39. – Vol. 1. – P. 31−39.
Bouleti C, Iung B, Himbert D, Brochet E, Messika-Zeitoun D, Detaint D, Garbarz E, Cormier B, Vahanian A. Reinterventions after percutaneous mitral commissurotomy during long-term follow-up, up to 20 years: the role of repeat percutaneous mitral, commissurotomy. Eur Heart J 2013; 34:1923–1930.
Leavitt JI, Coats MH, Falk RH. Effects of exercise on transmitralgradient and pulmonary artery pressure in patients with mitralstenosis or a prosthetic mitral valve: a Doppler echocardiographicstudy. J Am Coll Cardiol 1991; 17:1520–6.
Cheriex EC, Pieters FA, Janssen JH, de Swart H, Palmans-Meulemans A. Value of exercise Doppler-echocardiography inpatients with mitral stenosis. Int J Cardiol 1994; 45:219–26.
No authors, Complications and mortality of percutaneous balloon mitral commissurotomy: a report from the National Heart, Lung, and BloodInstitute Balloon Valvuloplasty Registry. Circulation 1992; 85:2014–24.
Cannan CR, Nishimura RA, Reeder GS, et al. Echocardiographicassessment of commissural calcium: a simple predictor of outcomeafter percutaneous mitral balloon valvotomy. J Am Coll Cardiol 1997; 29:175–80.
Padial L.R., Freitas N, Sagie A, et al. Echocardiography can predictwhich patients will develop severe mitral regurgitation after percutaneousmitral valvulotomy. J Am Coll Cardiol 1996; 27:1225–31.
Коваленко В.Н. Ревматические болезни: номенклатура, классификация, стандарты диагностики и лечения / В.Н. Коваленко , Н.М. Шуба — К.: ООО Катран групп, 2002-214с.
Cieslewicz G, Juszczyk G, Foremny J, et al. Inhaled corticosteroidimproves bronchial reactivity and decreases symptoms in patients with mitral stenosis. Chest 1998; 114:1070–4.
Nishimura RA, O’Gara PT, Bavaria JE, Brindis RG, Carroll JD, Kavinsky CJ, Lindman BR, Linderbaum JA, Little SH, Mack MJ, Mauri L, Miranda WR, Shahian DM, Sundt TM III. 2018 AATS/ACC/ASE/SCAI/STS expert consensus systems of care document: a proposal, to optimize care for patients with valvular heart disease: a joint report of the American Association for Thoracic Surgery, American College of Cardiology, American Society of Echocardiography, Society for Cardiovascular Angiography and Interventions, and, Society of Thoracic Surgeons. J Thorac Cardiovasc Surg. 2019;157(6):e327-e354.
Рыбка М.М., Хинчагов Д.Я. Под ред. Л.А. Бокерия. Протоколы анестезиологического обеспечения кардиохирургических операций, выполняемых при ишемической болезни сердца, патологии клапанного аппарата, нарушениях ритма, гипертрофической кардиомиопатии, аневризмах восходящего отдела аорты у пациентов различных возрастных групп. Методические рекомендации. М.: НЦССХ им. А. Н. Бакулева РАМН; 2015.
Сторожаков Г.И., Гендлин Г. Е., Миллер О.А. Болезни клапанов сердца. – М., Практика, 2012. – 200 с.
Тактика врача-кардиолога: практическое руководство/под ред. Ж.Д. Кобалава. – М., ГЭОТАР-Медиа, 2021. – 320 с.
Shaw T.R., Sutaria N, Prendergast B. Clinical and haemodynamicprofiles of young, middle aged, and elderly patients with mitralstenosis undergoing mitral balloon valvotomy. Heart 2003; 89:1430–6.
Арутюнов Г.П., Рылова А.К., Колесникова Е.А., Костюкевич О.И., Евзерихина А.В. Кардиореабилитация. – М.: МЕДпремм-информ, 2013. – 336с.
Какучая Т.Т. Современные аспекты кардиореабилитации. М.: НЦССХ им. А.Н. Бакулева, 2015, 254 с.
Alan S., Ulgen MS, Ozdemir K, Keles T, Toprak N. Reliability andefficacy of metoprolol and diltiazem in patients having mild tomoderate mitral stenosis with sinus rhythm. Angiology 2002; 53:575–81.
Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am, Coll Cardiol 2020; Dec 17;
Г.Е. Ройтберг, А.В. Струтынский. Внутренние болезни. Сердечно-сосудистая система. 2017 г. Стр. 680.
Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. European Heart Journal. 2022;43(7):561-632.
Nunes MCP, Tan TC, Elmariah S, et al. The echo score revisited: impact of incorporating commissural morphology and leaflet displacement to the prediction of outcome for patients undergoing percutaneous mitral valvuloplasty. Circulation. 2014;129:886–95.
Baumgartner H, Hung J, Bermejo J, et al. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. Eur J Echocardiogr. 2009; 10:1–25.
Ellis K., Ziada KM, Vivekananthan D, et al. Transthoracic echocardiographic predictors of left atrial appendage thrombus. Am J Cardiol. 2006;97:421–5.
Nina C Wunderlich , Roy Beigel, Robert J Siegel. Management of mitral stenosis using 2D and 3D echo-Doppler imaging. JACC Cardiovasc Imaging. 2013 Nov; 6(11):1191-205.
S S Shakil, D F Osmany, A K Biswas, S M Iqbal, S Nahar, M T Chowdhury, M Asaduzzaman, C M Ahmed. 3D Echocardiography Is More Efficient In Detail Assessment of Calcification in Chronic Rheumatic Mitral Stenosis. Mymensingh Med J. 2020 Jul; 29(3):579-588.
Helmut Baumgartner, Judy Hung, Javier Bermejo, John B. Chambers, Arturo Evangelista, Brian P. Griffin, Bernard Iung, Catherine M. Otto, Patricia A. Pellikka, and Miguel Quin˜ones. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations, for clinical practice. European Journal of Echocardiography (2009) 10, 1–25.
Grimaldi A, Olivotto I, Figini F, et al. Dynamic assessment of “valvular reserve capacity” in patients with rheumatic mitral stenosis. Eur Heart J Cardiovasc Imaging. 2012; 13:476–82.
Kadriye Orta Kılıçkesmez 1, Serdar Küçükoğlu. Value of stress echocardiography in mitral stenosis. Anadolu Kardiyol Derg. 2013 May; 13(3):257-60.
Julien Magne, Patrizio Lancellotti, Luc A Pierard. Stress echocardiography and mitral valvular heart disease. Cardiol Clin. 2013 May; 31(2):311-21.
Cemil Izgi 1, Nihal Ozdemir, Cihan Cevik, Olcay Ozveren, Ruken Bengi Bakal, Cihangir Kaymaz, Mehmet Ozkan. Mitral valve resistance as a determinant of resting and stress pulmonary artery pressure in patients with mitral stenosis: a dobutamine stress, study. J Am Soc Echocardiogr. 2007 Oct;20(10):1160-6.
E. Picano, P. Pibarot, P. Lancelotti, et al. The emerging role of exercise testing and stress echocardiography in valvular heart disease. J Am Coll Cardiol, 54 (2009), pp. 2251-2260.
Patrizio Lancellotti, Raluca Dulgheru, Yun Yun Go, Tadafumi Sugimoto, Stella Marchetta, Cécile Oury, Madalina Garbi. Stress echocardiography in patients with native valvular heart disease. Heart. 2018 May; 104(10):807-813.
Linda D Gillam, Leo Marcoff. Stress Echocardiography. Circ Cardiovasc Imaging. 2019 Jun; 12(6):e009319.
James L Gentry, Parth K Parikh, Alaa Alashi, A Marc Gillinov, Gosta B Pettersson, L Leonardo Rodriguez, Zoran B Popovic, Kimi Sato, Richard A Grimm, Samir R Kapadia, E Murat Tuzcu, Lars G Svensson, Brian P Griffin, Milind Y Desai. Characteristics and, Outcomes in a Contemporary Group of Patients With Suspected Significant Mitral Stenosis Undergoing Treadmill Stress Echocardiographyп, Circ Cardiovasc Imaging. 2019 Jun;12(6):e009062. doi: 10.1161/CIRCIMAGING.119.009062.
Suh WM, Kern MJ. Addressing the hemodynamic dilemma of combined mitral and aortic stenosis. Catheter Cardiovasc Interv. 2008; 71:944–9.
Reis G, Motta MS, Barbosa MM, et al. Dobutamine stress echocardiography for noninvasive assessment and risk stratification of patients with rheumatic mitral stenosis. J Am Coll Cardiol. 2004; 43:393–401.
Roshdy HS, Meshrif AM, El-Dosouky II. Value of the mitral valve resistance in evaluation of symptomatic patients with mild and moderate mitral stenosis—a dobutamine stress echocardiographic study. Echocardiography. 2014; 31:347–52.
Ahmad Al-Taweel, Mohamed Faher Almahmoud, Yasmine Khairandish, Masood Ahmad. Degenerative mitral valve stenosis: Diagnosis and management. 2019 Oct; 36(10):1901-1909.
Nikhil Prakash Patil , Karuna Katti. Chronic mitral stenosis.Circulation. 2011 Jun 21; 123(24):2897.
Andreas H Mahnken 1, Georg Mühlenbruch, Marco Das, Joachim E Wildberger, Harald P Kühl, Rolf W Günther, Malte Kelm, Ralf Koos. MDCT detection of mitral valve calcification: prevalence and clinical relevance compared with echocardiography. AJR Am J Roentgenol. 2007 May;188(5):1264-9.
Ozgül Uçar 1, Murat Vural, Zehra Cetfïn, Serkan Gökaslan, Tugba Gürsoy, Lale Paşaoğlu, Suha Koparal, Sinan Aydoğlu. Assessment of planimetric mitral valve area using 16-row multidetector computed tomography in patients with rheumatic mitral stenosis. J Heart Valve Dis. 2011 Jan;20(1):13-7.
Basil Al-Sabeq 1, Mohammed A Chamsi-Pasha. Imaging in mitral stenosis.Curr Opin Cardiol. 2020 Sep; 35(5):445-453.
Steven M Hollenberg. Valvular Heart Disease in Adults: Etiologies, Classification, and Diagnosis. FP Essent. 2017 Jun; 457:11-16.
Jason M Tarkin, Andrej Ćorović, Christopher Wall, Deepa Gopalan, James Hf Rudd. Positron emission tomography imaging in cardiovascular disease. Heart. 2020 Nov; 106(22):1712-1718.
Melvin D Cheitlin, Stress echocardiography in mitral stenosis: when is it useful? J Am Coll Cardiol. 2004 Feb 4; 43(3):402-4.
Alexander Lembcke 1, Tahir Durmus, Yvonne Westermann, Anja Geigenmueller, Benjamin Claus, Craig Butler, Holger Thiele. Assessment of mitral valve stenosis by helical MDCT: comparison with transthoracic doppler echocardiography and cardiac catheterization. AJR Am J Roentgenol. 2011 Sep;197(3):614-22.
Alec Vahanian, Friedhelm Beyersdorf, Fabien Praz, Milan Milojevic, Stephan Baldus, Johann Bauersachs, Davide Capodanno, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease: Developed by the Task Force for the management of, valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS), European Heart Journal, 2021.
Rigolin VH, Higgenbotham MB, Robiolio PA, et al. Effect of inadequate cardiac output reserve on exercise tolerance in patients with moderate mitral stenosis. Am J Cardiol. 1997; 80:236–40.
Laufer-Perl M, Gura Y, Shimiaie J, et al. Mechanisms of effort intolerance in patients with rheumatic mitral stenosis: combined echocardiography and cardiopulmonary stress protocol. J Am Coll Cardiol Img. 2017; 10:622–33.
Kitzman DW, Upadhya B, Zhao D. New concepts in an old disease: exercise intolerance in moderate mitral stenosis. J Am Coll Cardiol Img. 2017; 10:634–6.
Saggu DK, Narain VS, Dwivedi SK, et al. Effect of ivabradine on heart rate and duration of exercise in patients with mild-to-moderate mitral stenosis: a randomized comparison with metoprolol. J Cardiovasc Pharmacol. 2015; 65:552–4.
Parakh N, Chaturvedi V, Kurian S, et al. Effect of ivabradine vs atenolol on heart rate and effort tolerance in patients with mild to moderate mitral stenosis and normal sinus rhythm. J Card Fail. 2012; 18:282–8.
Agrawal V., Kumar N., Lohiya B., et al. «Metoprolol vs ivabradine in patients with mitral stenosis in sinus rhythm» Int J Cardiol. 2016; 221:562–6.
Yusuf J, Goyal M, Mukhopadhyay S, et al. Effect of heart rate control on coagulation status in patients of rheumatic mitral stenosis with atrial fibrillation–a pilot study. Indian Heart J. 2015; S40–5, 67.
Caldeira D, David C, Sampaio C. Rate versus rhythm control in atrial fibrillation and clinical outcomes: updated systematic review and meta-analysis of randomized controlled trials. Arch Cardiovasc Dis. 2012; 10.1016/j.acvd.2011.11, 105: 226–238.
Chen SJ, Yin YH, Dong Y et al. Efficacy of rate and rhythm control strategy in patients with atrial fibrillation: meta-analysis. Zhonghua Xin Xue Guan Bing Za Zhi. 2012; 40:68–72.
Al-Khatib SM, Allen LaPointe NM, Chatterjee R et al. Rate- and rhythm-control therapies in patients with atrial fibrillation: a systematic review. Ann Intern Med. 2014; 160:760–773.
Chatterjee S, Sardar P, Lichstein E et al. Pharmacologic rate versus rhythm-control strategies in atrial fibrillation: an updated comprehensive review and meta-analysis. PACE. 2013; 36:122–133.
January CT, Wann LS, Alpert JS et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm, Society. J Am Coll Cardiol. 2014;64: e1–76. doi: 10.1016/j.jacc.2014.03.022.
Tse HF, Lam YM, Lau CP et al. Comparison of digoxin versus low-dose amiodarone for ventricular rate control in patients with chronic atrial fibrillation. Clin Exp Pharmacol Physiol. 2001; 28:446-450.
Connolly SJ, Ezekowitz MD, Yusuf S et al. RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009; 361:1139–1151.
Giugliano RP, O’Gara PT. DOACs in Patients with mitral stenosis and atrial fibrillation: time for a randomized clinical trial. J Am Coll Cardiol. 2019; 73:1132–4.
Omran H, Rang B, Schmidt H, et al. Incidence of left atrial thrombi in patients in sinus rhythm and with a recent neurologic deficit. Am Heart J. 2000; 140:658–62.
Kim JY, Kim S-H, Myong J-P, et al. Outcomes of direct oral anticoagulants in patients with mitral stenosis. J Am Coll Cardiol. 2019; 73:1123–31.
Granger CB, Alexander JH, McMurray JJ et al. ARISTOTLE Committees and Investigators. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011; 365:981–992.
Patel MR, Mahaffey KW, Garg J et al. ROCKET AF Investigators. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011; 365:883–891.
Connolly SJ, Pogue J, Eikelboom J et al. ACTIVE W Investigators. Benefit of oral anticoagulant over antiplatelet therapy in atrial fibrillation depends on the quality of international normalized ratio control achieved by centers and countries,» as measured by time in therapeutic range. Circulation. 2008;118:2029–2037.
Wan Y, Heneghan C, Perera R et al. Anticoagulation control and prediction of adverse events in patients with atrial fibrillation: a systematic review. Circ Cardiovasc Qual Outcomes. 2008; 1:84–91.
De Caterina R, Husted S, Wallentin L et al. Vitamin K antagonists in heart disease: current status and perspectives (Section III). Position paper of the ESC Working Group on Throm-bosis—Task Force on Anticoagulants in Heart Disease. Thromb Haemost. 2013, 110:1087–1107.
Vestergaard AS, Skjøth F, Larsen TB, Ehlers LH. The importance of mean time in thera-peutic range for complication rates in warfarin therapy of patients withatrial fibrillation: A systematic review and meta-regression analysis. PLoS One. 2017, 12:e0188482. doi: 10.1371/journal.pone.0188482.
Liu S, Li X, Shi Q et al. Outcomes associated with warfarin time in therapeutic range among US veterans with nonvalvular atrial fibrillation. Curr Med Res Opin. 2018; 34:415–421.
Björck F, Renlund H, Lip GY et al. Outcomes in a Warfarin-Treated Population With Atrial Fibrillation. JAMA Cardiol. 2016; 1:172–180.
Кропачева Е.С., Боровков Н. Н., Вавилова Т. В. и др. Быстрые темпы насыщения варфарином—предиктор развития чрезмерной гипокоагуляции. Модернизация алгоритма подбора дозы варфарина // Атеротромбоз. — 2015. — № 1. — С. 74–86.
Pan KL, Singer DE, Ovbiagele B et al. Effects of non-vitamin K antagonist oral anticoagulants versus warfarin in patients with atrial fibrillation and valvular heart disease: a systematic review and meta-analysis. J Am Heart Assoc. 2017; 6:e005835.
Renda G, Ricci F, Giugliano RP, De Caterina R. Non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation and valvular heart disease. J Am Coll Cardiol. 2017; 69:1363–1371.
Noseworthy PA, Yao X, Shah ND, Gersh BJ. Comparative effectiveness and safety of non-vitamin K antagonist oral anticoagulants versus warfarin in patients with atrial fibrillation and valvular heart disease. Int J Cardiol. 2016; 209:181–183.
McDonagh T.A., Metra M., Adamo M., Gardner R.S., Baumbach A., Michael Bohm, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. European Heart Journal. 2021; 42 (36): 3599-3726.
Borer JS, Sharma A. Drug Therapy for Heart Valve Diseases. Circulation. 2015;132(11):1038-45.
McMurray JJV., Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA, Ponikowski P, Sabatine MS, Anand IS, Bělohlávek J, Böhm M, Chiang C-E, Chopra VK, de Boer RA, Desai AS, Diez M, Drozdz J, Dukát A, Ge J, Howlett JG, Katova T, Kitakaze M, Ljungman CEA, Merkely B, Nicolau JC, O’Meara E, Petrie MC, Vinh PN, Schou M, Tereshchenko S, Verma S, Held C, DeMets DL, Docherty KF, Jhund PS, Bengtsson O, Sjöstrand M, Langkilde A-M Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. September 19, 2019. doi: 10.1056/NEJMoa1911303.
Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P, Januzzi J, Verma S, Tsutsui H, Brueckmann M, Jamal W, Kimura K, Schnee J, Zeller C, Cotton D, Bocchi E, Bohm M, Choi DJ, Chopra V, Chuquiure E, Giannetti N, Janssens S, Zhang J, Gonzalez Juanatey JR, Kaul S, Brunner-La Rocca HP, Merkely B, Nicholls SJ, Perrone S, Pina I, Ponikowski P, Sattar N, Senni M, Seronde MF, Spinar J, Squire I, Taddei S, Wanner C, Zannad F, EMPERORReduced Trial Investigators. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020; 383:1413-1424.
Zannad F, Ferreira JP, Pocock SJ, Anker SD, Butler J, Filippatos G, Brueckmann M, Ofstad AP, Pfarr E, Jamal W, Packer M. SGLT2 inhibitors in patients with heart failure with reduced ejection fraction: a meta-analysis of the EMPEROR-Reduced and DAPA-HF trials. Lancet. 2020;396(10254):819-829. doi: 10.1016/S0140-6736(20)31824-9.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJV, Mebazaa A, Mindham R, Muneretto C, Francesco Piepoli M, Price S, Rosano GMC, Ruschitzka F, Skibelund AK; ESC Scientific Document Group. 2023 Focused Update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2023 Oct 1;44(37):3627-3639. doi: 10.1093/eurheartj/ehad195.
Hammermeister K, Sethi GK, Henderson WG, Grover FL, Oprian C,Rahimtoola SH. Outcomes 15 years after valve replacement with a mechanicalversus a bioprosthetic valve: final report of the Veterans Affairs randomizedtrial. J Am CollCardiol 2000;36:1152–1158.
Oxenham H, Bloomfield P, Wheatley DJ, Lee RJ, Cunningham J, Prescott RJ,Miller HC.Twenty year comparison of a Bjork-Shiley mechanical heart valve with porcine bioprostheses. Heart 2003;89:715–721.
Stassano P, Di Tommaso L, Monaco M, IorioF, Pepino P, Spampinato N, VosaC. Aortic valve replacement: a prospective randomized evaluation of mechanicalversus biological valves in patients ages 55 to 70 years. J Am CollCardiol2009;54:1862–1868.
Craver JM, Cohen C, Weintraub WS. Case-matched comparison of mitral valve replacement and repair. Ann ThoracSurg 1990;49:964–9.
Tokmakoglu H, Vural KM, Ozatik MA, Cehreli S, Sener E,Tasdemir O. Closed commissurotomy versus balloon valvuloplasty for rheumatic mitral stenosis. J Heart Valve Dis 2001; 10:281–7.
Gibson CM, Mehran R, Bode C, Halperin J, Verheugt FW, Wildgoose P, Birmingham M, Ianus J, Burton P, van Eickels M, Korjian S, Daaboul Y, Lip GY, Cohen M, Husted S, Peterson ED, Fox KA. Prevention of bleeding in patients with atrial fibrillation undergoing PCI. N Engl J Med 2016;375:2423–2434.
Dewilde WJ, Oirbans T, Verheugt FW, Kelder JC, De Smet BJ, Herrman JP, Adriaenssens T, Vrolix M, Heestermans AA, Vis MM, Tijsen JG, van‘t Hof AW, ten Berg JM, WOEST study investigators. Use of clopidogrel with or without aspirin in patients taking oral anticoagulant therapy and undergoing percutaneous coronary intervention: an open-label, randomised, controlled trial. Lancet 2013;381:1107–1115.
Eikelboom JW, Connolly SJ, Brueckmann M, Granger CB, Kappetein AP, Mack MJ, Blatchford J, Devenny K, Friedman J, Guiver K, Harper R, Khder Y, Lobmeyer MT, Maas H, Voigt JU, Simoons ML, Van de Werf F, RE-ALIGN. Investigators. Dabigatran versus warfarin in patients with mechanical heart valves. N Engl J Med 2013;369:1206–1214.
Itthidet Kamthornthanakarn, Rungroj Krittayaphong. Optimal INR level for warfarin therapy after mechanical mitral valve replacement. BMC Cardiovasc Disord. 2019 Apr 25; 10.1186/s12872-019-1078-3., 19(1):97.
Fiedler KA, Maeng M, Mehilli J, Schulz-Schupke S, Byrne RA, Sibbing D, Hoppmann P, Schneider S, Fusaro M, Ott I, Kristensen SD, Ibrahim T, Massberg S, Schunkert H, Laugwitz KL, Kastrati A, Sarafoff N. Duration of triple therapy in patients requiring oral anticoagulation after drug-eluting stent implantation: the ISAR-TRIPLE Trial. J Am Coll Cardiol 2015;65:1619–1629.
Brennan JM, Edwards FH, Zhao Y, O’Brien S, Booth ME, Dokholyan RS, Douglas PS, Peterson ED, DEcIDE AVR Research Team. Early anticoagulation of bioprosthetic aortic valves in older patients: results from the Society of Thoracic Surgeons Adult. Cardiac Surgery National Database. J Am Coll Cardiol 2012;60:971-977.
Merie C, Kober L, Skov Olsen P, Andersson C, Gislason G, Skov Jensen J, Torp-Pedersen C. Association of warfarin therapy duration after bioprostheticaortic valve replacement with risk of mortality, thromboembolic complications and bleeding. JAMA 2012;308:2118-2125.
Christersson C, James SK, Lindhagen L, Ahlsson A, Friberg O, Jeppsson A, Stahle E. Comparison of warfarin versus antiplatelet therapy after surgical bioprosthetic aortic valve replacement. Heart 2020; 106:838-844.
Rafiq S, Steinbruchel DA, Lilleor NB, Moller CH, Lund JT, Thiis JJ, Kober L, Olsen PS. Antithrombotic therapy after bioprosthetic aortic valve implantation: Warfarin versus aspirin, a randomized controlled trial. 2017 Feb; 150:104-110.
Dunning J, Versteegh M, Fabbri A, Pavie A, Kolh P, Lockowandt U, Nashef SA. EACTS Audit and Guidelines Committee. Guideline on antiplatelet and anticoagulation management in cardiac surgery. Eur J Cardiothorac Surg 2008; 34:73–92.
Cannegieter SC, Rosendaal FR, Briet E. Thromboembolic and bleeding complications in patients with mechanical heart valve prostheses. Circulation 1994; 89:635-641.
Heneghan C, Ward A, Perera R, Self-Monitoring Trialist C, Bankhead C, Fuller A, Stevens R, Bradford K, Tyndel S, Alonso-Coello P, Ansell J, Beyth R, Bernardo A, Christensen TD, Cromheecke ME, Edson RG, Fitzmaurice D, Gadisseur AP, Garcia-Alamino JM, Jacobson A, Kaatz S, Kamali F, Khan TI, Knight E, Kortke H, Levi M, Matchar D, Menendez-Jandula B, Rakovac I, Schaefer C, Siebenhofer A, Souto JC, Sunderji R, Gin K, Shalansky K, Voller H, Wagner O, Zittermann A. Self-monitoring of oral anticoagulation:, systematic review and meta-analysis of individual patient data. Lancet 2012;379:322-334.
Massel DR, Little SH. Antiplatelet and anticoagulation for patients with prosthetic heart valves. Cochrane Database Syst Rev 2013:CD003464.
Hansen ML, Sorensen R, Clausen MT, Fog-Petersen ML, Raunso J, Gadsboll N, Gislason GH, Folke F, Andersen SS, Schramm TK, Abildstrom SZ, Poulsen HE, Kober L, Torp-Pedersen C. Risk of bleeding with single, dual, or triple therapy with warfarin, aspirin, and clopidogrel in patients with atrial fibrillation. Arch Intern Med 2010;170:1433.
Raffaele De Caterina, Stefan Agewall, Felicita Andreotti et all. Great Debate: Triple antithrombotic therapy in patients with atrial fibrillation undergoing coronary stenting should be limited to 1 week. European Heart Journal, Volume 43, Issue 37, 1 October 2022, Pages 3512–3527.
Sardo S, Osawa EA, Finco G, Gomes Galas FRB, de Almeida JP, Cutuli SL, Frassanito C, Landoni G, Hajjar LA. Nitric Oxide in Cardiac Surgery: A Meta-Analysis of Randomized Controlled Trials. J Cardiothorac Vasc Anesth. 2018 Dec; 32(6):2512-2519. doi: 10.1053/j.jvca.2018.02.003.
Tessler J, Bordoni B. Cardiac Rehabilitation. 2022 May 23. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 30725881.
Lowe G, Twaddle S. The Scottish Intercollegiate Guidelines Network (SIGN): an update. Scott Med J. 2005 May;50(2):51-2. doi: 10.1177/003693300505000202. PMID: 15977513.
Ambrosetti M., Abreu A., Corrà U., et al. Secondary prevention through comprehensive cardiovascular rehabilitation: From knowledge to implementation. 2020 update. A position paper from the Secondary Prevention and Rehabilitation Section,» of the European Association of Preventive Cardiology. European Journal of Preventive Cardiology. 2021; 28: 460-495. doi: 10.1177/2047487320913379.
Butchart E.G., Gohlke-Barwolf C., Antunes M.J., et al. Recommendations for the management of patients after heart valve surgery. Eur Heart J. 2005; 10.1093/eurheartj/ehi426., 26(22):2463–2471.
Sibilitz K.L., Berg S.K., Tang L.H., et al. Exercise-based cardiac rehabilitation for adults after heart valve surgery. Cochrane Database Syst Rev. 2016; 3:CD010876; doi:10.1002/14651858.CD010876.
Butchart EG, Gohlke-Barwolf C, Antunes MJ, et al. Recommendations for the management of patients after heart valve surgery. Eur Heart J 2005;26: 2463–2471. Eur Heart J. 2005;26: 2463–2471 doi:10.1093/eurheartj/ehi426
Anderson L., Sharp G.A., Norton R.J., et al. Home-based versus centre-based cardiac rehabilitation. Cochrane Database of Systematic Reviews. 2017; 10.1002/14651858.CD007130.pub4, 6: CD007130.
Thomas R.J., Beatty A.L., Beckle T.M., et al. Home-based cardiac rehabilitation: a scientific statement from the American Association of Cardiovascular and Pulmonary Rehabilitation. The American Heart Association, and the American College of Cardiology. Circulation. 2019;140:e69-e89. doi: 10.1161/CIR.0000000000000663.
Kraal J.J., Van den Akker-Van Marle M.E., Abu-Hanna A., et al. Clinical and cost-effectiveness of home-based cardiac rehabilitation compared to conventional, centre-based cardiac rehabilitation: results of the FIT@Home study. Eur J Prev Cardiol. 2017;24:1260-73. doi: 10.1177/2047487317710803.
Федеральный закон от 29.07.2017г., № 242-ФЗ "О внесении изменений в отдельные законодательные акты Российской Федерации по вопросам применения информационных технологий в сфере охраны здоровья" https://www.garant.ru/products/ipo/prime/doc/716328.
Kanejima Y, Shimogai T, Kitamura M, Ishihara K, Izawa KP. 13: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2020 Sep 28;17(19):7091.
Sahar W, Ajaz N, Haider Z, Jalal A. Effectiveness of Pre-operative Respiratory Muscle Training versus Conventional Treatment for Improving Post operative Pulmonary Health after Coronary Artery Bypass Grafting. Pak J Med Sci. 2020 Sep-Oct;36(6):1216-1219.
Borregaard B, Dahl JS, Riber LPS, Ekholm O, Sibilitz KL, Weiss M, Sørensen J, Berg SK, Møller JE. Effect of early, individualised and intensified follow-up after open heart valve surgery on unplanned cardiac hospital readmissions and all-cause mortality. Int J Cardiol. 2019 Aug 15;289:30-36.
Thomas R.J., Balady G., Banka G., et al. 2018 ACC/AHA Clinical Performance and Quality Measures for Cardiac Rehabilitation: A Report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. J Am Coll Cardiol. 2018;71(16):1814-1837. doi: 10.1016/j.jacc.2018.01.004. PMID: 29606402.
Иванова Г.Е., Мельникова Е.В., Шмонин А.А., Вербицкая Е.В., Аронов Д.М., Белкин А.А., Беляев А.Ф., Бодрова Р.А., Бубнова М.Г., Буйлова Т.В., Мальцева М.Н., Мишина И.Е., Нестерин К.В., Никифоров В.В., Прокопенко С.В., Сарана А.М., Стаховская Л.В., Суворов А.Ю., Хасанова Д.Р., Цыкунов М.Б. Применение международной классификации функционирования в процессе медицинской реабилитации. Вестник восстановительной медицины. 2018;6(88):2-77.
Wildner M, Quittan M, Portenier L, Wilke S, Boldt C, Stucki G, Kostanjsek N, Grill E. ICF Core Set for patients with cardiopulmonary conditions in early post-acute rehabilitation facilities. Disabil Rehabil. 2005 Apr 8-22;27(7-8):397-404.
Wyckoff MH, Greif R, Morley PT et al. Collaborators. 2022 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations: Summary From the Basic Life Support; Advanced Life Support; Pediatric Life Support; Neonatal Life Support; Education, Implementation, and Teams; and First Aid Task Forces. Circulation. 2022 Dec 20;146(25):e483-e557. doi: 10.1161/CIR.0000000000001095. Epub 2022 Nov 3. PMID: 36325905.
Sommaruga M., Angelino E., Della Porta P., et al. Best practice in psychological activities in cardiovascular prevention and rehabilitation: Position Paper. Monaldi Arch Chest Dis. 2018; 10.4081/monaldi.2018.966., 88(2): 966.
Visseren F.L.J., Mach F., Smulders Y.M., et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021; 10.1093/eurheartj/ehab484., 42(34):3227-3337.
Ambrosetti M., Abreu A., Cornelissen V., et al. Delphi consensus recommendations on how to provide cardiovascular rehabilitation in the COVID-19 era. Eur J Prev Cardiol. 2021; 33624042, 28(5):541-557. doi: 10.1093/eurjpc/zwaa080
Mezzani A., Hamm L.F., Jones A.M., et al. Aerobic exercise intensity assessment and prescription in cardiac rehabilitation: A joint position statement of the European association for cardiovascular prevention and rehabilitation, the American association of cardiovascular and pulmonary rehabilitation and the Canadian association of cardiac rehabilitation. Eur J Prev Cardiol. 2013; 20: 442–467. doi: 10.1177/2047487312460484
Fletcher G.F., Ades P.A., Kligfield P., et al. Exercise Standards for Testing and Training A Scientific Statement From the American Heart Association. Circulation. 2013; 10.1161/CIR.0b013e31829b5b44., 128:873-934.
Opasich C., De Feo S., Pinna G.D., et al. Distance walked in the 6-minute test soon after cardiac surgery: toward an efficient use in the individual patient. Chest. 2004; 15596676., 126(6):1796-801. doi: 10.1378/chest.126.6.1796.
Meurin P., Iliou M.C., Driss A.B., et al. Early exercise training after mitral valve repair: a multicentric prospective French study. Chest. 2005; 10.1378/chest.128.3.1638., 128(3):1638-44.
Nechwatal R.M., Cardiac rehabilitation after surgical and transcatheter valve replacement and repair. Dtsch Z Sportmed.2018; doi:10.5960/dzsm.2018.343, 69: 285-292.
Oyama J, Kudo Y, Maeda T, Node K, Makino N. Hyperthermia by bathing in a hot spring improves cardiovascular functions and reduces the production of inflammatory cytokines in patients with chronic heart failure. Heart Vessels. 2013 Mar;28(2):173-8. doi: 10.1007/s00380-011-0220-7. Epub 2012 Jan 11. PMID: 22231540.
The British Association for Cardiovascular Prevention and Rehabilitation. The BACPR Standards and Core Components for Cardiovascular Disease Prevention and Rehabilitation 2012 (2nd edition). The British Cardiovascular Society 2012.
Abraham LN, Sibilitz KL, Berg SK, Tang LH, Risom SS, Lindschou J, Taylor RS, Borregaard B, Zwisler AD. Exercise-based cardiac rehabilitation for adults after heart valve surgery. Cochrane Database Syst Rev. 2021 May 7;5(5):CD010876. doi: 10.1002/14651858.CD010876.pub3. PMID: 33962483; PMCID: PMC8105032.
Князева Т.А., Бадтиева В.А. Физиобальнеотерапия сердечно-сосудистых заболеваний. Практическое руководство. М. Медпресс-информ, 2008. – 272 с.
Приказ Министерства здравоохранения РФ от 28 сентября 2020 г. № 1029н “Об утверждении перечней медицинских показаний и противопоказаний для санаторно-курортного лечения".
Долецкий А.А., Свет А.В., Андреев Д.А., Санер Х.; под ред. А.Л. Сыркина. Кардиореабилитация. – М.: ООО «Медицинское информационное агентство», 2016. – 240с.
Кардиология: национальное руководство: под ред. Е. В. Шляхто. 2-е изд., перераб. И доп. М.: ГЭОТАР-Медиа, 2015. 800 с.
Руководство по кардиологии: под ред. акад. Е. И. Чазова. В 4 т. М.: Издательский дом «Практика», 2014.
Ниебауэр Дж. Кардиореабилитация: практическое руководство. – М.: Логосфера, 2012. – 312с.
Кардиореабилитация и вторичная профилактика: под ред. Профессора Д.М. Аронова. Издательская группа «ГЭОТАР-Медиа», 2021.
Wilkins GT, Weyman AE, Abascal VM, Block PC, Palacios IF. Percutaneous bal-loon dilatation of the mitral valve: an analysis of echocardiographic variablesrelated to outcome and the mechanism of dilatation. Br Heart J1988; 60:299–308.
Iung B, Cormier B, Ducimetiere P, Porte JM, Nallet O, Michel PL, Acar J,Vahanian A. Immediate results of percutaneous mitral commissurotomy. A pre-dictive model on a series of 1514 patients. Circulation 1996; 94:2124–2130.
Zigmond A.S., Snaith R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica. 1983;67 (6):361–370. doi:10.1111/j.16000447.1983.tb09716.x
Borg G.A. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377-381.
Borg G.A. Psychophysical scaling with applications in physical work and the perception of exertion. ScandJWorkEnvironHealth. 1990;16 (Suppl 1):55–58.
Munro J., Booth A., Nicholl J. Routine preoperative testing: a systematic review of the evidence //Health Technology Assessment (Winchester, England). – 1997. – Т. 1. – №. 12. – С. i-iv; 1. Macpherson D. S. Preoperative laboratory testing: should any tests be" routine" before surgery? //Medical Clinics of North America. 1993;77(2):289-308.
Mohan M. et al. Preoperative screening of HIV, HBV, HCV essential for surgical team and patients both–A research study in Department of Surgery, Tertiary Care Institute of North India, Rohilkhand Medical College and Hospital, Bareilly (UP) India //Int J Contemp Med Res (Online). 2018;5(7):G1-G4.
Сокольская М.А., Бокерия О.Л. Алгоритм предоперационного обследования и подготовка к операции пациентов с приобретенными пороками сердца //Бюллетень НЦССХ им. АН Бакулева РАМН. Сердечно-сосудистые заболевания. 2017;18(S6):46-46.
Заболотских И.Б. и др. Периоперационное ведение пациентов с сопутствующей патологией клапанного аппарата сердца //Вестник интенсивной терапии имени А.И. Салтанова. 2016;3:55-69.
Демин А.А., Кобалава Ж.Д., Скопин И.И. и др. Инфекционный эндокардит и инфекция внутрисердечных устройств. Клинические рекомендации 2021 // РКЖ. 2022.
№10.doi:10.15829/1560-4071-2022-5233.
Delgado V, Ajmone Marsan N, de Waha S, et al. ESC Scientific Document Group. 2023 ESC Guidelines for the management of endocarditis. Eur Heart J. 2023 Oct 14;44(39):3948-4042. doi: 10.1093/eurheartj/ehad193. Erratum in: Eur Heart J. 2023 Sep 20;: Erratum in: Eur Heart J. 2024 Jan 1;45(1):56. PMID: 37622656.
Çelik A, Altay H, Azap A, Çavuşoğlu Y, Nalbantgil S, Şenol E, Temizhan A, Yılmaz MB. Vaccination of adults with heart failure and chronic heart conditions: Expert opinion. Turk Kardiyol Dern Ars. 2018;46(8):723-734.
Roberto M. Lang, Michelle Bierig, Richard B. Devereux et al. Recommendations for the quantitative assessment of the structure and function of the heart chambers. Eur J Echocardiography (2006) 7, 79–108.
Landoni G. [и др.]. Volatile Anesthetics versus Total Intravenous Anesthesia for Cardiac Surgery // New England Journal of Medicine. 2019. № 13 (380).
2021 ESC/EACTS GUIDELINES FOR THE MANAGEMENT OF VALVULAR HEART DISEASE The Task Force for the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Russ J Cardiol. 2022;27(7):371–434.
Chakravarty T, Sondergaard L, Friedman J, De Backer O, Berman D, Kofoed KF, Jilaihawi H, Shiota T, Abramowitz Y, Jorgensen TH, Rami T, Israr S, Fontana G, de Knegt M, Fuchs A, Lyden P, Trento A, Bhatt DL, Leon MB, Makkar RR, Resolve, SAVORY Investigators. Subclinical leaflet thrombosis in surgical and . transcatheter bioprosthetic aortic valves: an observational study. Lancet 2017;389:2383-2392.
Karthikeyan G, Senguttuvan NB, Joseph J, Devasenapathy N, Bahl VK, Airan B. Urgent surgery compared with fibrinolytic therapy for the treatment of left-sided prosthetic heart valve thrombosis: a systematic review and meta-analysis of observational studies. Eur Heart J 2013;34:1557-1566.
De Backer O, Dangas GD, Jilaihawi H, Leipsic JA, Terkelsen CJ, Makkar R, Kini AS, Veien KT, Abdel-Wahab M, Kim WK, Balan P, Van Mieghem N, Mathiassen ON, Jeger RV, Arnold M, Mehran R, Guimaraes AHC, Norgaard BL, Kofoed KF, Blanke P, Windecker S, Sondergaard L, GALILEO-4D Investigators. Reduced leaflet motion after transcatheter aortic-valve replacement. N Engl J Med 2020;382:130-139.
Alkhouli M, Rihal CS, Zack CJ, Eleid MF, Maor E, Sarraf M, Cabalka AK, Reeder GS, Hagler DJ, Maalouf JF, Nkomo VT, Schaff HV, Said SM. Transcatheter and surgical management of mitral paravalvular leak: long-term outcomes. JACC Cardiovasc Interv 2017;10:1946-1956.
Siddiqi TJ, Usman MS, Shahid I, Ahmed J, Khan SU, Ya'qoub L, Rihal CS, Alkhouli M. Utility of the CHA2DS2-VASc score for predicting ischaemic stroke in patients with or without atrial fibrillation: a systematic review and meta-analysis. Eur J Prev Cardiol. 2022 Mar 30;29(4):625-631.
Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010 Feb;137(2):263-72.
Gerber MA, Baltimore RS, Eaton CB, Gewitz M, Rowley AH, Shulman ST, Taubert KA. Prevention of rheumatic fever and diagnosis and treatment of acute Streptococcal pharyngitis: a scientific statement from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young, the Interdisciplinary Council on Functional Genomics and Translational Biology, and the Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Academy of Pediatrics. Circulation. 2009 Mar 24;119(11):1541-51.
Дроздов Д.В., Макаров Л.М., Баркан В.С., и др. Регистрация электрокардиограммы покоя в 12 общепринятых отведениях взрослым и детям 2023. Методические рекомендации. Российский кардиологический журнал. 2023;28(10):5631. doi:10.15829/1560-4071-2023-5631
Мацкеплишвили С.Т., Саидова М.А., Мироненко М.Ю., и др. Выполнение стандартной трансторакальной эхокардиографии. Методические рекомендации 2024. Российский кардиологический журнал. 2025;30(2):6271. https://doi.org/10.15829/1560-4071-2025-6271.
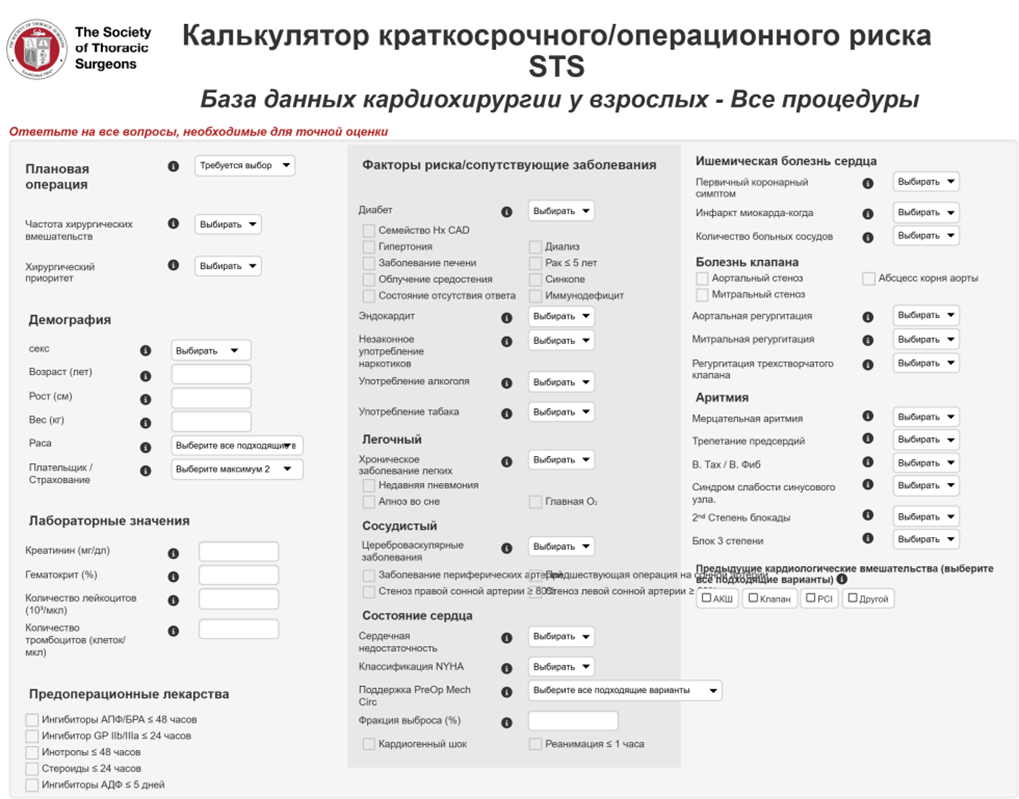
STS Short-term / Operative Risk Calculator Adult Cardiac Surgery Database - All Procedures https://acsdriskcalc.research.sts.org/
EuroSCORE is the world's best-known cardiac surgery risk stratification model https://euroscore.org/
Barili F, Pacini D, Capo A, Rasovic O, Grossi C, Alamanni F, et al. Does EuroSCORE II per-form better than its original versions? A multicentre validation study. European heart journal. 2013;34(1):22-9.
Shahian DM, Jacobs JP, Badhwar V, Kurlansky PA, Furnary AP, Cleveland JC, Jr., et al. The Society of Thoracic Surgeons 2018 adult cardiac surgery risk models: part 1-background, design con-siderations, and model development. The Annals of thoracic surgery. 2018;105(5):1411-8.
Kundi H, Popma JJ, Reynolds MR, Strom JB, Pinto DS, Valsdottir LR, et al. Frailty and related outcomes in patients undergoing transcatheter valve therapies in a nationwide cohort. European heart journal. 2019;40(27):2231-9.
Hosler QP, Maltagliati AJ, Shi SM, Afilalo J, Popma JJ, Khabbaz KR, et al. A practical two-stage frailty assessment for older adults undergoing aortic valve replacement. J Am Geriatr Soc. 2019;67(10):2031-7.
Dent E, Martin FC, Bergman H, Woo J, Romero-Ortuno R, Walston JD. Management of frailty: opportunities, challenges, and future directions. Lancet (London, England). 2019;394(10206):1376-86.
Goldfarb M, Lauck S, Webb JG, Asgar AW, Perrault LP, Piazza N, et al. Malnutrition and mor-tality in frail and non-frail older adults undergoing aortic valve replacement. Circulation. 2018;138(20):2202-11.
Yanagisawa R, Tanaka M, Yashima F, Arai T, Kohno T, Shimizu H, et al. Frequency and conse-quences of cognitive impairment in patients underwent transcatheter aortic valve implantation. The American journal of cardiology. 2018;122(5):844-50.
Gunter RL, Kilgo P, Guyton RA, Chen EP, Puskas JD, Cooper WA, et al. Impact of preopera-tive chronic lung disease on survival after surgical aortic valve replacement. The Annals of thoracic surgery. 2013;96(4):1322-8.
Allende R, Webb JG, Munoz-Garcia AJ, de Jaegere P, Tamburino C, Dager AE, et al. Advanced chronic kidney disease in patients undergoing transcatheter aortic valve implantation: insights on clin-ical outcomes and prognostic markers from a large cohort of patients. European heart journal. 2014;35(38):2685-96.
Tirado-Conte G, Rodés-Cabau J, Rodríguez-Olivares R, Barbanti M, Lhermusier T, Amat-Santos I, et al. Clinical outcomes and prognosis markers of patients with liver disease undergoing transcatheter aortic valve replacement: a propensity score-matched analysis. Circ Cardiovasc Interv. 2018;11(3):e005727.
Rossebo A.B., Pedersen T.R., Boman K., Brudi P., Chambers J.B., Egstrup K., Gerdts E., Gohlke-Barwolf C., Holme I., Kesaniemi Y.A., Malbecq W., Nienaber C.A., Ray S., Skjaerpe T., Wachtell K., Willenheimer R., SEAS Investigators. Intensive lipid lowering with simvastatin and ezetimibe in aortic stenosis. N Engl J Med 2008;359:1343–1356.
Демин А.А., Кобалава Ж.Д., Скопин И.И., и др. Инфекционный эндокардит и инфекция внутрисердечных устройств. Клинические рекомендации 2021. Российский кардиологический журнал. 2022;27(10):5233. https://doi.org/10.15829/1560-4071-2022-5233
Кобалава Ж.Д., Конради А.О., догода С.В., и др. Артериальная гипертензия у взрослых. Клинические рекомендации 2024. Российский кардиологический журнал. 2024;29(9):6117. https://doi.org/10.15829/1560-4071-2024-6117
Ежов М.В., Кухарчук В.В., Сергиенко И.В., и др. Нарушения липидного обмена. Клинические рекомендации 2023. Российский кардиологический журнал. 2023;28(5):5471. https://doi.org/10.15829/1560-4071-2023-5471
Галявич А.С., Терещенко С.Н., Ускач Т.М., и др. Хроническая сердечная недостаточность. Клинические рекомендации 2024. Российский кардиологический журнал. 2024;29(11):6162. https://doi.org/10.15829/1560-4071-2024-6162
Аверков О.В., Арутюнян Г.К., Дупляков Д.В., и др. Острый инфаркт миокарда с подъемом сегмента ST электрокардиограммы. Клинические рекомендации 2024. Российский кардиологический журнал. 2025;30(3):6306. https://doi.org/10.15829/1560-4071-2025-6306
Барбараш О.Л., Карпов Ю.А., Панов А.В., и др. Стабильная ишемическая болезнь сердца. Клинические рекомендации 2024. Российский кардиологический журнал. 2024;29(9):6110. https://doi.org/10.15829/1560-4071-2024-6110

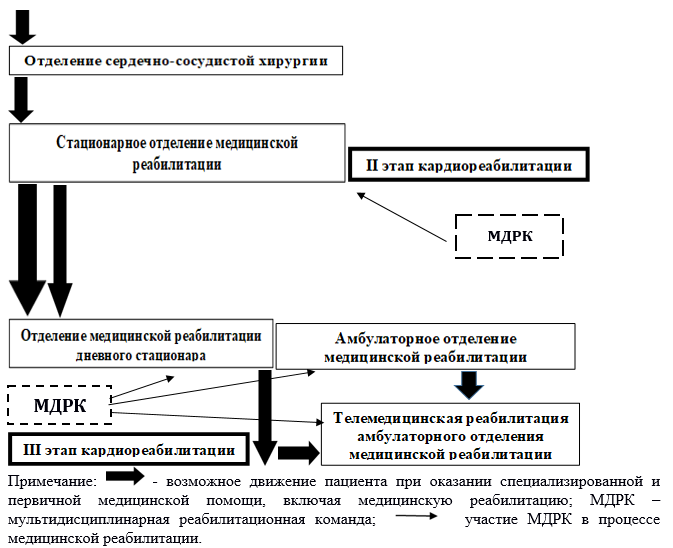
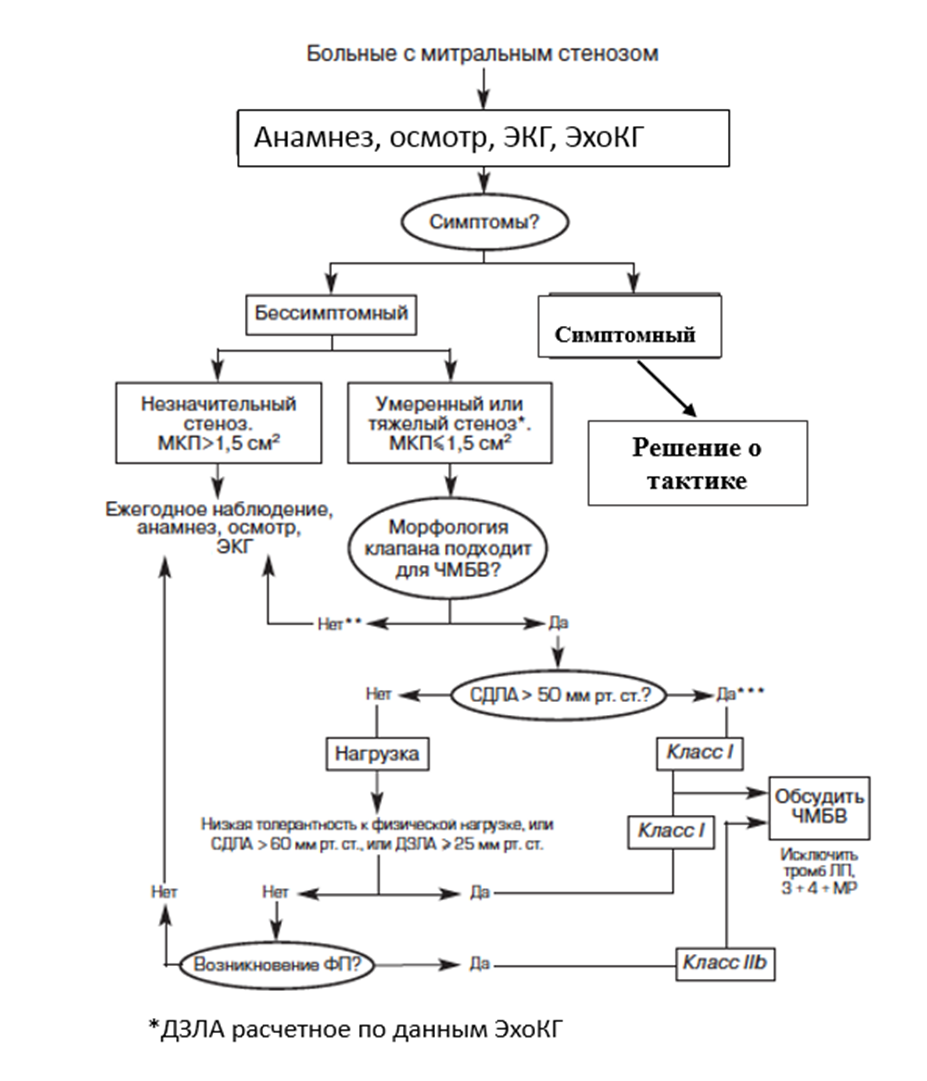 Приложение Б1. Алгоритм организации кардиологической реабилитации у пациентов с митральным стенозом (Рисунок П1.)
Приложение Б1. Алгоритм организации кардиологической реабилитации у пациентов с митральным стенозом (Рисунок П1.)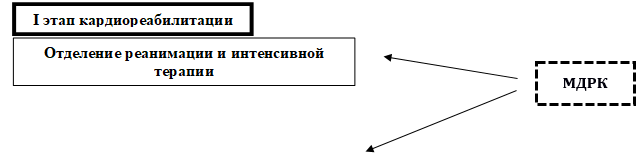
 Интерпретация:
Интерпретация: