N. Harrasser, F. Lenze, and J. Hamel, “Ballenhohlfuß,” Orthopade, vol. 50, no. 1, pp. 75–85, Jan. 2021, doi: 10.1007/s00132-020-04053-w.
Akram Ali Attaib Beshna, “Options for Management Choice Evidence-Based Treatment of Cavus Foot Deformity,” European Journal of Molecular & Clinical Medicine, vol. 08, no. 03, 2021.
J. Grice, H. Willmott, and H. Taylor, “Assessment and management of cavus foot deformity,” Orthop Trauma, vol. 30, no. 1, pp. 68–74, Feb. 2016, doi: 10.1016/j.mporth.2016.02.001.
J. Gil-Castillo, F. Alnajjar, A. Koutsou, D. Torricelli, and J. C. Moreno, “Advances in neuroprosthetic management of foot drop: a review,” J Neuroeng Rehabil, vol. 17, no. 1, p. 46, Dec. 2020, doi: 10.1186/s12984-020-00668-4.
Крамаренко Г. Н., “Наш опыт хирургического лечения поперечного плоскостопия и Hallux Valgus,” Ортопед., травматол. , pp. 11–15, 1973.
R. W. Haines and A. McDougall, “The anatomy of hallux valgus,” J Bone Joint Surg Br, vol. 36-B, no. 2, pp. 272–293, May 1954, doi: 10.1302/0301-620X.36B2.272.
Вреден Р.Р., “Hallux Valgus ,” pp. 117–119, 1925.
S. Barnett, J. L. Cunningham, and S. West, “A Comparison of vertical force and temporal parameters produced by an in-shoe pressure measuring system and a force platform.” [Online]. Available: www.elsevier.com/locate/clinbiomech
J. Schnepp, “L’hallux valgus: bases pathogeniques et anatomopathogeniques. Therapeutique et indications,” Expansion scientifique Francaise, pp. 269–277, 1986.
A. E. Hunt and R. M. Smith, “Mechanics and control of the flat versus normal foot during the stance phase of walking,” Clinical Biomechanics, vol. 19, no. 4, pp. 391–397, May 2004, doi: 10.1016/j.clinbiomech.2003.12.010.
R. A. Mann and M. J. Coughlin, “Hallux valgus--etiology, anatomy, treatment and surgical considerations.,” Clin Orthop Relat Res, no. 157, pp. 31–41, Jun. 1981.
Батенкова Г.И., “К механогенезу распластанности переднего отдела стопы и hallux valgus,” Ортопед. травматол. , pp. 36–39, 1974.
J. N. Antrobus, “The Primary Deformity in Hallux Valgus and Metatarsus Primus Varus,” Clin Orthop Relat Res, vol. 184, no. NA;, p. 251???255, Apr. 1984, doi: 10.1097/00003086-198404000-00042.
Зайцева Е.И., “Отдаленные результаты хирургического лечения вальгусной деформации большого пальца стопы ,” Ортопед., травматол. , pp. 43–47, 1958.
Barouk L. S, “Hallux valgus congenital, symposium ,” Med. Chir. Pied, pp. 65–112, 1991.
J. M. Hiss, “Hallux valgus its cause and simplified treatment,” The American Journal of Surgery, vol. 11, no. 1, pp. 51–57, Jan. 1931, doi: 10.1016/S0002-9610(31)91059-3.
R. A. Mann, “Hallux valgus.,” Instr Course Lect, vol. 31, pp. 180–200, 1982.
C. M. J. Mann R. A., “Surgery of the Foot and Ankle ,” Philadelphia: Elsevier Saunders, vol. 9, 2007.
J. J. Del Vecchio and M. Dalmau-Pastor, “Anatomy, Biomechanics, and Pathogenesis of the Lesser Toes Deformities,” Foot Ankle Clin, vol. 29, no. 4, pp. 557–569, Dec. 2024, doi: 10.1016/j.fcl.2024.03.002.
K. Malhotra, K. Davda, and D. Singh, “The pathology and management of lesser toe deformities,” EFORT Open Rev, vol. 1, no. 11, pp. 409–419, Nov. 2016, doi: 10.1302/2058-5241.1.160017.
J. F. Doty, M. J. Coughlin, L. Weil, and C. Nery, “Etiology and Management of Lesser Toe Metatarsophalangeal Joint Instability,” Foot Ankle Clin, vol. 19, no. 3, pp. 385–405, Sep. 2014, doi: 10.1016/j.fcl.2014.06.013.
Л.С.Н. Косарева М.А., “Проблемы хирургического лечения молоткообразной деформации пальцев стопы (обзор литературы),” Acta Biomed Sci, pp. 235–242, 2020.
Dudley J. Morton, “Metatarsus atavicus: The Identification of a Distinctive Type of Foot Disorder,” J Bone Joint Surg, 1927.
Morton D. J., “Foot disorders in general practice,” J Am Med Assoc, pp. 1112–1119, 1937.
M. J. Coughlin and F. M. Thompson, “The high price of high-fashion footwear.,” Instr Course Lect, vol. 44, pp. 371–7, 1995.
Л.С.Н. Усольцев И.В., “Хирургическое лечение тяжёлых деформаций пальцев стопы при ревматоидном артрите,” Acta Biomed Sci, pp. 123–127, 2019.
D. Rodríguez-Sanz et al., “Foot disorders in the elderly: A mini-review,” Disease-a-Month, vol. 64, no. 3, pp. 64–91, Mar. 2018, doi: 10.1016/j.disamonth.2017.08.001.
Батенкова Г.И, “К механогенезу распластанности переднего отдела стопы и hallux valgus ,” Ортопед. травматол, pp. 36–39, 1974.
H. J. Visser, J. Wolfe, R. Kouri, and R. Aviles, “Neurologic Conditions Associated with Cavus Foot Deformity,” Clin Podiatr Med Surg, vol. 38, no. 3, pp. 323–342, Jul. 2021, doi: 10.1016/j.cpm.2021.03.001.
R. M. Schwend and J. C. Drennan, “Cavus Foot Deformity in Children,” Journal of the American Academy of Orthopaedic Surgeons, vol. 11, no. 3, pp. 201–211, May 2003, doi: 10.5435/00124635-200305000-00007.
B. Qin, S. Wu, and H. Zhang, “Evaluation and Management of Cavus Foot in Adults: A Narrative Review,” J Clin Med, vol. 11, no. 13, p. 3679, Jun. 2022, doi: 10.3390/jcm11133679.
A. S. Eleswarapu, B. Yamini, and R. J. Bielski, “Evaluating the Cavus Foot,” Pediatr Ann, vol. 45, no. 6, Jun. 2016, doi: 10.3928/00904481-20160426-01.
A. J. Rosenbaum, J. Lisella, N. Patel, and N. Phillips, “The Cavus Foot,” Medical Clinics of North America, vol. 98, no. 2, pp. 301–312, Mar. 2014, doi: 10.1016/j.mcna.2013.10.008.
P. Wicart, “Cavus foot, from neonates to adolescents,” Orthopaedics & Traumatology: Surgery & Research, vol. 98, no. 7, pp. 813–828, Nov. 2012, doi: 10.1016/j.otsr.2012.09.003.
G. P. Guyton, “Peroneal Tendon Injury Associated with the Cavus Foot,” in The Peroneal Tendons, Cham: Springer International Publishing, 2020, pp. 357–372. doi: 10.1007/978-3-030-46646-6_22.
L. A. Forrester et al., “Perfusion is Not Measurably Decreased in Idiopathic Clubfoot.,” Bull Hosp Jt Dis (2013), vol. 76, no. 3, pp. 203–206, Sep. 2018.
B. T. Williams, S. Li, and M. S. Myerson, “Managing the Severe Cavus Foot Deformity in Global Humanitarian Programs.,” Instr Course Lect, vol. 73, pp. 247–261, 2024.
M. P. Nogueira, F. Farcetta, and A. Zuccon, “Cavus Foot,” Foot Ankle Clin, vol. 20, no. 4, pp. 645–656, Dec. 2015, doi: 10.1016/j.fcl.2015.07.007.
P. Kumari, “Congenital Clubfoot: A Comprehensive Review,” Orthopedics and Rheumatology Open Access Journal, vol. 8, no. 1, Jul. 2017, doi: 10.19080/OROAJ.2017.08.555728.
J. Kernohan, B. Levack, and J. Wilson, “Entrapment of the superficial peroneal nerve. Three case reports,” J Bone Joint Surg Br, vol. 67-B, no. 1, pp. 60–61, Jan. 1985, doi: 10.1302/0301-620X.67B1.3968146.
R. K. Nath and C. Somasundaram, “Incidence, Etiology, and Risk Factors Associated with Foot Drop.,” Eplasty, vol. 23, p. e16, 2023.
A. Carolus, D. Mesbah, and C. Brenke, “Focusing on foot drop: Results from a patient survey and clinical examination,” The Foot, vol. 46, p. 101693, Mar. 2021, doi: 10.1016/j.foot.2020.101693.
J. Ma et al., “Risk Factors Analysis for Foot Drop Associated with Lumbar Disc Herniation: An Analysis of 236 Patients,” World Neurosurg, vol. 110, pp. e1017–e1024, Feb. 2018, doi: 10.1016/j.wneu.2017.11.154.
A. Ghai, S. Hooda, P. Kumar, R. Kumar, and P. Bansal, “Bilateral foot drop following lower limb orthopedic surgery under spinal anesthesia,” Canadian Journal of Anesthesia/Journal canadien d’anesthésie, vol. 52, no. 5, pp. 550–550, May 2005, doi: 10.1007/BF03016543.
P. Aqueveque, P. Ortega, E. Pino, F. Saavedra, E. Germany, and B. Gómez, “After Stroke Movement Impairments: A Review of Current Technologies for Rehabilitation,” in Physical Disabilities - Therapeutic Implications, InTech, 2017. doi: 10.5772/67577.
A. Dubin, “Gait,” Medical Clinics of North America, vol. 98, no. 2, pp. 205–211, Mar. 2014, doi: 10.1016/j.mcna.2013.10.002.
T. Akbas, R. R. Neptune, and J. Sulzer, “Neuromusculoskeletal Simulation Reveals Abnormal Rectus Femoris-Gluteus Medius Coupling in Post-stroke Gait,” Front Neurol, vol. 10, Apr. 2019, doi: 10.3389/fneur.2019.00301.
K. A. Shorter, A. Wu, and A. D. Kuo, “The high cost of swing leg circumduction during human walking,” Gait Posture, vol. 54, pp. 265–270, May 2017, doi: 10.1016/j.gaitpost.2017.03.021.
V. A. Stanhope, B. A. Knarr, D. S. Reisman, and J. S. Higginson, “Frontal plane compensatory strategies associated with self-selected walking speed in individuals post-stroke,” Clinical Biomechanics, vol. 29, no. 5, pp. 518–522, May 2014, doi: 10.1016/j.clinbiomech.2014.03.013.
Беленький А.Г., “Плоскостопие: проявление и диагностика ,” Consilium medicum, pp. 618–622, 2005.
К.Ю.Ф. Черкес-Заде Д.И., Хирургия стопы . 2002.
D. Karasick and K. L. Wapner, “Hallux valgus deformity: preoperative radiologic assessment.,” American Journal of Roentgenology, vol. 155, no. 1, pp. 119–123, Jul. 1990, doi: 10.2214/ajr.155.1.2112832.
Л.М.П. Карданов А.А., Оперативное лечение деформаций первого луча стопы: история и современные аспекты . 2008.
M. R. A. Coughlin MJ, “Lesser toe deformities,” Surgery of the Foot and Ankle, pp. 341–412, 1993.
C. Y. K. Tang, K. H. Ng, and J. Lai, “Adult flatfoot,” The BMJ, vol. 368, Feb. 2020, doi: 10.1136/bmj.m295.
A. Almaaw, “Flatfoot Prevalence in Riyadh City Saudi Arabia And Its Association with Obesity, Using Three Footprint Indices; Clark’s Angle, Chippaux-Smirak Index, and Staheli Index,” Orthopedics and Rheumatology Open Access Journal, vol. 15, no. 2, Nov. 2019, doi: 10.19080/OROAJ.2019.15.555909.
J. W. Suh, W. J. Choi, and J. W. Lee, “Diagnosis and Treatment of Cavus Foot,” Journal of Korean Foot and Ankle Society, vol. 20, no. 2, p. 55, 2016, doi: 10.14193/jkfas.2016.20.2.55.
C. Peishun, Z. Haiwang, L. Taotao, G. Hongli, M. Yu, and Z. Wanrong, “Changes in Gait Characteristics of Stroke Patients with Foot Drop after the Combination Treatment of Foot Drop Stimulator and Moving Treadmill Training,” Neural Plast, vol. 2021, pp. 1–5, Nov. 2021, doi: 10.1155/2021/9480957.
I. Aprile et al., “Multicenter study of peroneal mononeuropathy: clinical, neurophysiologic, and quality of life assessment,” Journal of the Peripheral Nervous System, vol. 10, no. 3, pp. 259–268, Sep. 2005, doi: 10.1111/j.1085-9489.2005.10304.x.
J. L. Thomas et al., “Diagnosis and Treatment of Forefoot Disorders. Section 1: Digital Deformities,” The Journal of Foot and Ankle Surgery, vol. 48, no. 2, pp. 230–238, Mar. 2009, doi: 10.1053/J.JFAS.2008.12.003.
G. V. Yu, M. S. Judge, J. R. Hudson, and F. E. Seidelmann, “Predislocation Syndrome,” J Am Podiatr Med Assoc, vol. 92, no. 4, pp. 182–199, Apr. 2002, doi: 10.7547/87507315-92-4-182.
V. Dhukaram, S. Hossain, J. Sampath, and J. L. Barrie, “Correction of hammer toe with an extended release of the metatarsophalangeal joint,” J Bone Joint Surg, vol. 84, no. 7, pp. 986–990, Sep. 2002, doi: 10.1302/0301-620X.84B7.12811.
C. Saro, B. Andren, Z. Wildemyr, and L. Felländer-Tsai, “Outcome after Distal Metatarsal Osteotomy for Hallux Valgus: A Prospective Randomized Controlled Trial of Two Methods,” Foot Ankle Int, vol. 28, no. 7, pp. 778–787, Jul. 2007, doi: 10.3113/FAI.2007.0778.
M. J. Coughlin and C. P. Jones, “Hallux valgus: Demographics, etiology, and radiographic assessment,” Foot Ankle Int, vol. 28, no. 7, pp. 759–777, Jul. 2007, doi: 10.3113/FAI.2007.0759.
L. Berti, G. Celin, P. Caravaggi, S. Giannini, and A. Leardini, “Biomechanical assessment of two different surgical treatments for the correction of flat foot,” J Foot Ankle Res, vol. 7, no. S1, Jan. 2014, doi: 10.1186/1757-1146-7-s1-a52.
C. C. Akoh and P. Phisitkul, “Clinical Examination and Radiographic Assessment of the Cavus Foot,” Foot Ankle Clin, vol. 24, no. 2, pp. 183–193, Jun. 2019, doi: 10.1016/j.fcl.2019.02.002.
A.-L. Ménard, M. Begon, J. Barrette, and M.-L. Nault, “Cavus Foot in Soccer Players: Increased Prevalence in Experienced Players and Risk Factor for Injury,” J Am Podiatr Med Assoc, vol. 113, no. 6, Nov. 2023, doi: 10.7547/21-095.
C.-H. Jeon, N.-S. Chung, Y.-S. Lee, K.-H. Son, and J.-H. Kim, “Assessment of Hip Abductor Power in Patients With Foot Drop,” Spine (Phila Pa 1976), vol. 38, no. 3, pp. 257–263, Feb. 2013, doi: 10.1097/BRS.0b013e318268c8bc.
C. Poage, C. Roth, and B. Scott, “Peroneal Nerve Palsy,” Journal of the American Academy of Orthopaedic Surgeons, vol. 24, no. 1, pp. 1–10, Jan. 2016, doi: 10.5435/JAAOS-D-14-00420.
Маркс В.О., Ортопедическая диагностика. 1978.
E. Dalton McGlamry, “Comprehensive Textbook of Foot Surgery,” Baltimore: Williams & Wilkins, vol. 1, pp. 345–360, 1987.
H.-J. Trnka, B. Kabon, R. Zettl, A. Kaider, M. Salzer, and P. Ritschl, “Helal metatarsal osteotomy for the treatment of metatarsalgia: a critical analysis of results,” Orthopedics, vol. 19, no. 5, pp. 457–461, May 1996, doi: 10.3928/0147-7447-19960501-17.
R. H. Hardy and J. C. R. Clapham, “Observations on hallux valgus,” J Bone Joint Surg Br, vol. 33-B, no. 3, pp. 376–391, Aug. 1951, doi: 10.1302/0301-620X.33B3.376.
Miller M. D., Thompson S. R., Hart J. A., “Miller’s Review of Orthopaedics,” Philadelphia: Elsevier, 8th ed., 2019.
T. J. Shelton et al., “The Influence of Percentage Weight-Bearing on Foot Radiographs,” Foot Ankle Spec, vol. 12, no. 4, pp. 363–369, Aug. 2019, doi: 10.1177/1938640018810412.
Процко В.Г., “Хирургическое лечение плосковальгусной деформации стоп у взрослых. Автореферат на соискание ученой степени доктора медицинских наук.,” 2019.
M. W. Steel, K. A. Johnson, M. A. DeWitz, and D. M. Ilstrup, “Radiographic Measurements of the Normal Adult Foot,” Foot Ankle, vol. 1, no. 3, pp. 151–158, Nov. 1980, doi: 10.1177/107110078000100304.
G. Scott, D. W. Wilson, and G. Bentley, “Roentgenographic assessment in hallux valgus.,” Clin Orthop Relat Res, no. 267, pp. 143–7, Jun. 1991.
G. Laporta, T. Melillo, and D. Olinsky, “X-ray evaluation of hallux abducto valgus deformity,” J Am Podiatr Med Assoc, vol. 64, no. 8, pp. 544–566, Aug. 1974, doi: 10.7547/87507315-64-8-544.
C. Polichetti et al., “Adult Acquired Flatfoot Deformity: A Narrative Review about Imaging Findings,” Diagnostics, vol. 13, no. 2, p. 225, Jan. 2023, doi: 10.3390/diagnostics13020225.
P. Gowda, A. Kohli, and A. Chhabra, “Two-Dimensional and 3-Dimensional MRI Assessment of Progressive Collapsing Foot Deformity—Adult Acquired Flat Foot Deformity,” Foot Ankle Clin, vol. 28, no. 3, pp. 551–566, Sep. 2023, doi: 10.1016/j.fcl.2023.04.009.
С.Н.А. Лунева И.Е., “Нейропатия малоберцового нерва: общие подходы к диагностике и терапии,” Нервно-мышечные болезни , pp. 29–36, 2022.
P. R. Cavanagh, J. S. Ulbrecht, W. Zanine, R. L. Welling, D. Leschinsky, and C. van Schie, “A Method for the Investigation of the Effects of Outsole Modifications in Therapeutic Footwear,” Foot Ankle Int, vol. 17, no. 11, pp. 706–708, Nov. 1996, doi: 10.1177/107110079601701111.
A. Rozema, J. S. Ulbrecht, S. E. Pammer, and P. R. Cavanagh, “In-Shoe Plantar Pressures During Activities of Daily Living: Implications for Therapeutic Footwear Design,” Foot Ankle Int, vol. 17, no. 6, pp. 352–359, Jun. 1996, doi: 10.1177/107110079601700611.
M. Herchenröder, D. Wilfling, and J. Steinhäuser, “Evidence for foot orthoses for adults with flatfoot: a systematic review,” J Foot Ankle Res, vol. 14, no. 1, Jan. 2021, doi: 10.1186/s13047-021-00499-z.
J. Ying, Y. Xu, B. István, and F. Ren, “Adjusted Indirect and Mixed Comparisons of Conservative Treatments for Hallux Valgus: A Systematic Review and Network Meta-Analysis.,” Int J Environ Res Public Health, vol. 18, no. 7, Apr. 2021, doi: 10.3390/ijerph18073841.
G. Balasankar, A. Luximon, and A. Al-Jumaily, “Current conservative management and classification of club foot: A review,” J Pediatr Rehabil Med, vol. 9, no. 4, pp. 257–264, Nov. 2016, doi: 10.3233/PRM-160394.
S. Tejero et al., “Conservative Treatment of Ankle Osteoarthritis,” J Clin Med, vol. 10, no. 19, p. 4561, Sep. 2021, doi: 10.3390/jcm10194561.
G. Colò, M. Leigheb, M. F. Surace, F. Fusini. “The efficacy of shoes modification and orthotics in hallux valgus deformity: a comprehensive review of literature”. Musculoskeletal surgery, vol. 108, no. 4, pp. 395–402, doi: 10.1007/s12306-024-00839-9.
S. Hara, M. Kitano, and S. Kudo, “The effects of short foot exercises to treat flat foot deformity: A systematic review,” J Back Musculoskelet Rehabil, vol. 36, no. 1, pp. 21–33, Jan. 2023, doi: 10.3233/BMR-210374.
B. Unver, E. U. Erdem, and E. Akbas, “Effects of Short-Foot Exercises on Foot Posture, Pain, Disability, and Plantar Pressure in Pes Planus,” J Sport Rehabil, vol. 29, no. 4, pp. 436–440, May 2020, doi: 10.1123/jsr.2018-0363.
T. Brijwasi and P. Borkar, “A comprehensive exercise program improves foot alignment in people with flexible flat foot: a randomised trial,” J Physiother, vol. 69, no. 1, pp. 42–46, Jan. 2023, doi: 10.1016/j.jphys.2022.11.011.
N. Utsahachant, P. Sakulsriprasert, K. Sinsurin, M. P. Jensen, and S. Sungkue, “Corrigendum to ‘Effects of short foot exercise combined with lower extremity training on dynamic foot function in individuals with flexible flatfoot: A randomized controlled trial’ [Gait & Posture 104 (2023) 109–115/doi: 10.1016/j.gaitpost.2023.06.013. Epub 2023 Jun 22],” Gait Posture, vol. 119, p. 135, Jun. 2025, doi: 10.1016/j.gaitpost.2025.03.005.
H. A. C. Jacob, “Forces acting in the forefoot during normal gait – an estimate,” Clinical Biomechanics, vol. 16, no. 9, pp. 783–792, Nov. 2001, doi: 10.1016/S0268-0033(01)00070-5.
W. M. Glasoe, V. Phadke, F. A. Pena, D. J. Nuckley, and P. M. Ludewig, “An Image-Based Gait Simulation Study of Tarsal Kinematics in Women With Hallux Valgus,” Phys Ther, vol. 93, no. 11, pp. 1551–1562, Nov. 2013, doi: 10.2522/ptj.20130025.
J. Shamus, E. Shamus, R. N. Gugel, B. S. Brucker, and C. Skaruppa, “The Effect of Sesamoid Mobilization, Flexor Hallucis Strengthening, and Gait Training on Reducing Pain and Restoring Function in Individuals With Hallux Limitus: A Clinical Trial,” Journal of Orthopaedic & Sports Physical Therapy, vol. 34, no. 7, pp. 368–376, Jul. 2004, doi: 10.2519/jospt.2004.34.7.368.
F. Alam, S. Raza, J. A. Moiz, P. Bhati, S. Anwer, and A. Alghadir, “Effects of selective strengthening of tibialis posterior and stretching of iliopsoas on navicular drop, dynamic balance, and lower limb muscle activity in pronated feet: A randomized clinical trial,” Phys Sportsmed, vol. 47, no. 3, pp. 301–311, Jul. 2019, doi: 10.1080/00913847.2018.1553466.
K. Okamura, K. Egawa, T. Ikeda, K. Fukuda, and S. Kanai, “Relationship between foot muscle morphology and severity of pronated foot deformity and foot kinematics during gait: A preliminary study,” Gait Posture, vol. 86, pp. 273–277, May 2021, doi: 10.1016/j.gaitpost.2021.03.034.
S. T. Hawson, “Physical Therapy Post–Hallux Abducto Valgus Correction,” Clin Podiatr Med Surg, vol. 31, no. 2, pp. 309–322, Apr. 2014, doi: 10.1016/j.cpm.2014.01.002.
A. Dimeglio and F. Canavese, “The French functional physical therapy method for the treatment of congenital clubfoot,” Journal of Pediatric Orthopaedics B, vol. 21, no. 1, pp. 28–39, Jan. 2012, doi: 10.1097/BPB.0b013e32834ee5f8.
P. G. Plapler and D. Ling, “Treatment of Lesser Toe Deformities Based on Physical Therapy,” Foot Ankle Clin, vol. 29, no. 4, pp. 605–615, Dec. 2024, doi: 10.1016/j.fcl.2024.03.005.
M. Patil, M. S. Kulkarni, A. Sinha, and R. R. Ghorpade, “Biomechanical variations in patients with flatfoot deformity: Impact of gender, age, and BMI on foot kinetics and kinematics,” J Orthop, vol. 57, pp. 90–97, Nov. 2024, doi: 10.1016/j.jor.2024.06.018.
S. Boussaid et al., “Foot Functional Disability in Rheumatoid Arthritis: The Involvement of Body Mass Index,” Curr Rheumatol Rev, vol. 19, no. 3, pp. 373–379, Aug. 2023, doi: 10.2174/1573397119666221124152856.
J. Drzal-Grabiec et al., “The foot deformity versus postural control in females aged over 65 years.,” Acta Bioeng Biomech, vol. 16, no. 4, pp. 75–82, 2014.
A. Jafarnezhadgero, M. Madadi-Shad, S. M. Alavi-Mehr, and U. Granacher, “The long-term use of foot orthoses affects walking kinematics and kinetics of children with flexible flat feet: A randomized controlled trial,” PLoS One, vol. 13, no. 10, p. e0205187, Oct. 2018, doi: 10.1371/journal.pone.0205187.
M. N. Khan, B. C. Jacobs, and S. Ashbaugh, “Considerations in Footwear and Orthotics,” Primary Care: Clinics in Office Practice, vol. 40, no. 4, pp. 1001–1012, Dec. 2013, doi: 10.1016/j.pop.2013.08.013.
J. Boudarham, D. Pradon, N. Roche, D. Bensmail, and R. Zory, “Effects of a dynamic-ankle-foot orthosis (Liberté®) on kinematics and electromyographic activity during gait in hemiplegic patients with spastic foot equinus,” NeuroRehabilitation, vol. 35, no. 3, pp. 369–379, Nov. 2014, doi: 10.3233/NRE-141128.
J. F. Doty, R. G. Alvarez, T. B. Ervin, A. Heard, J. Gilbreath, and N. S. Richardson, “Biomechanical Evaluation of Custom Foot Orthoses for Hallux Valgus Deformity,” The Journal of Foot and Ankle Surgery, vol. 54, no. 5, pp. 852–855, Sep. 2015, doi: 10.1053/j.jfas.2015.01.011.
“Коксартроз. Клинические рекомендации.,” 2024.
“Гонартроз. Клинические рекомендации.,” 2024.
J. Boyd and R. Chmielewski, “Prevention of Infection in Foot and Ankle Surgery,” Clin Podiatr Med Surg, vol. 36, no. 1, pp. 37–58, Jan. 2019, doi: 10.1016/j.cpm.2018.08.007.
M. R. K. Modha, C. Morriss‐Roberts, M. Smither, J. Larholt, and I. Reilly, “Antibiotic prophylaxis in foot and ankle surgery: a systematic review of the literature,” J Foot Ankle Res, vol. 11, no. 1, Jan. 2018, doi: 10.1186/s13047-018-0303-0.
N. Huang et al., “Postoperative Infection and Revision Surgery Rates in Foot and Ankle Surgery Without Routine Prescription of Prophylactic Antibiotics,” JAAOS: Global Research and Reviews, vol. 7, no. 3, Mar. 2023, doi: 10.5435/JAAOSGlobal-D-23-00015.
J. Cheng, L. Zhang, J. Zhang, K. Asadi, and R. Farzan, “RETRACTED: Prevalence of surgical site infection and risk factors in patients after foot and ankle surgery: A systematic review and meta‐analysis,” Int Wound J, vol. 21, no. 1, Jan. 2024, doi: 10.1111/iwj.14350.
P. Butterworth, A. Terrill, A. Barwick, and R. Hermann, “The use of prophylactic antibiotics in podiatric foot and ankle surgery,” Infect Dis Health, vol. 22, no. 1, pp. 6–11, Mar. 2017, doi: 10.1016/j.idh.2017.01.002.
A. L. Akinyoola, O. O. Adegbehingbe, and A. Odunsi, “Timing of Antibiotic Prophylaxis in Tourniquet Surgery,” The Journal of Foot and Ankle Surgery, vol. 50, no. 4, pp. 374–376, Jul. 2011, doi: 10.1053/j.jfas.2011.04.008.
Брико Н.И., “Клинические рекомендации. Профилактика инфекций области хирургического вмешательства. ,” Ремедиум Н. Новгород, 2018, 2018.
Backes M, “WIFI Collaboration Group. Effect of Antibiotic Prophylaxis on Surgical Site Infections Following Removal of Orthopedic Implants Used for Treatment of Foot, Ankle, and Lower Leg Fractures: A Randomized Clinical Trial.,” JAMA, pp. 2438–2445, 2017.
R. Radl, N. Kastner, C. Aigner, H. Portugaller, H. Schreyer, and R. Windhager, “Venous thrombosis after hallux valgus surgery,” The Journal of Bone and Joint Surgery-American Volume, vol. 85, no. 7, pp. 1204–1208, Jul. 2003, doi: 10.2106/00004623-200307000-00004.
J. Mangwani, N. Sheikh, M. Cichero, and D. Williamson, “What is the evidence for chemical thromboprophylaxis in foot and ankle surgery? Systematic review of the English literature,” The Foot, vol. 25, no. 3, pp. 173–178, Sep. 2015, doi: 10.1016/j.foot.2014.07.007.
A. G. Witteveen, C. J. Hofstad, and G. M. Kerkhoffs, “Hyaluronic acid and other conservative treatment options for osteoarthritis of the ankle,” Cochrane Database of Systematic Reviews, vol. 2015, no. 10, Oct. 2015, doi: 10.1002/14651858.CD010643.pub2.
R. J. Petrella and A. Cogliano, “Intra-articular Hyaluronic Acid Treatment for Golfer’s Toe,” Phys Sportsmed, vol. 32, no. 7, pp. 41–45, Jul. 2004, doi: 10.3810/psm.2004.07.453.
T. Iannitti, D. Lodi, and B. Palmieri, “Intra-Articular Injections for the Treatment of Osteoarthritis,” Drugs R D, vol. 11, no. 1, pp. 13–27, Mar. 2011, doi: 10.2165/11539760-000000000-00000.
O. Mei-Dan, M. Carmont, L. Laver, G. Mann, N. Maffulli, and M. Nyska, “Intra-articular Injections of Hyaluronic Acid in Osteoarthritis of the Subtalar Joint: A Pilot Study,” The Journal of Foot and Ankle Surgery, vol. 52, no. 2, pp. 172–176, Mar. 2013, doi: 10.1053/j.jfas.2012.12.008.
S.-F. Sun, Y.-J. Chou, C.-W. Hsu, and W.-L. Chen, “Hyaluronic acid as a treatment for ankle osteoarthritis,” Curr Rev Musculoskelet Med, vol. 2, no. 2, pp. 78–82, Jun. 2009, doi: 10.1007/s12178-009-9048-5.
F. Ferreira Gomes, I. M. de Castro Junior, J. Antônio M. Guimarães, and A. Cordeiro, “Pharmacological treatment withcorticoid or hyaluronic acid injections into subtalar joint via lateral access v1,” Feb. 02, 2023. doi: 10.17504/protocols.io.ewov1o5zplr2/v1.
I. Repetto, B. Biti, P. Cerruti, R. Trentini, and L. Felli, “Conservative Treatment of Ankle Osteoarthritis: Can Platelet-Rich Plasma Effectively Postpone Surgery?,” The Journal of Foot and Ankle Surgery, vol. 56, no. 2, pp. 362–365, Mar. 2017, doi: 10.1053/j.jfas.2016.11.015.
Nibin Sunny, Saurabh Agarwal, Mahesh Navadaya, and Mayank Kumar Singh, “Role of platelet-rich plasma in insertion tendinitis,” Asian J Med Sci, vol. 15, no. 7, pp. 133–136, Jul. 2024, doi: 10.71152/ajms.v15i7.4101.
H. Miranda-Grajales, “Platelet-Rich Plasma,” in Treatment of Chronic Pain Conditions, New York, NY: Springer New York, 2017, pp. 183–184. doi: 10.1007/978-1-4939-6976-0_50.
Y. S. Kim, H. J. Lee, Y. J. Choi, Y. Il Kim, and Y. G. Koh, “Does an Injection of a Stromal Vascular Fraction Containing Adipose-Derived Mesenchymal Stem Cells Influence the Outcomes of Marrow Stimulation in Osteochondral Lesions of the Talus?,” Am J Sports Med, vol. 42, no. 10, pp. 2424–2434, Oct. 2014, doi: 10.1177/0363546514541778.
P. Bora and A. S. Majumdar, “Adipose tissue-derived stromal vascular fraction in regenerative medicine: a brief review on biology and translation,” Stem Cell Res Ther, vol. 8, no. 1, p. 145, Dec. 2017, doi: 10.1186/s13287-017-0598-y.
E. B. Lander, M. H. Berman, and J. R. See, “Safety of stromal vascular fraction cells applications in chronic pain,” Tech Reg Anesth Pain Manag, vol. 19, no. 1–2, pp. 10–13, Jan. 2015, doi: 10.1053/j.trap.2016.09.002.
J. K. Henry, R. Shakked, and S. J. Ellis, “Adult-Acquired Flatfoot Deformity,” Foot Ankle Orthop, vol. 4, no. 1, Jan. 2019, doi: 10.1177/2473011418820847.
E. Vulcano, J. T. Deland, and S. J. Ellis, “Approach and treatment of the adult acquired flatfoot deformity,” Curr Rev Musculoskelet Med, vol. 6, no. 4, pp. 294–303, Dec. 2013, doi: 10.1007/s12178-013-9173-z.
Maestro M, “Alghorythm of treatment Hallux Valgus ,” pp. 56–66, 2007.
Карданов А.А., “Наш опыт хирургического лечения валыусного отклонения первого пальца стопы посредством остеотомии SCARF ,” Травматология и ортопедия России, pp. 37–43, 2008.
Киреев В.С., “Исследование мобильности первой плюсневой кости при хирургической коррекции деформаций переднего отдела стопы с использованием scarf-остеотомиим,” Вестник медицинского института «РЕАВИЗ»: реабилитация, врач и здоровье., pp. 126–130, 2019.
S. E. Smith, K. B. Landorf, P. A. Butterworth, and H. B. Menz, “Scarf versus Chevron Osteotomy for the Correction of 1–2 Intermetatarsal Angle in Hallux Valgus: A Systematic Review and Meta-analysis,” The Journal of Foot and Ankle Surgery, vol. 51, no. 4, pp. 437–444, Jul. 2012, doi: 10.1053/j.jfas.2012.02.016.
Карданов А.А., Оперативное лечение деформаций первого луча стопы: история и современные аспекты . 2008.
Gudas C. J., “The complex deformity known as hallux abducto valgus,” Comprehensive textbook of hallux abducto valgusreconstruction, p. 453, 1992.
Бережной С.Ю., “Чрескожная модификация артродеза первого плюснеклиновидного сустава: проспективное исследование,” Травматология и ортопедия России, pp. 51–58, 2012.
D. H. Do, J. J. Sun, and D. K. Wukich, “Modified Lapidus Procedure and Hallux Valgus: A Systematic Review and Update on Triplanar Correction,” Orthopedic Clinics of North America, vol. 53, no. 4, pp. 499–508, Oct. 2022, doi: 10.1016/J.OCL.2022.05.005.
Д.С. Бобров, Л.Ю. Слиняков, А.Д. Ченский, М.И. Матвиенко, М.Ю. Холодаев, and Д. Хурцилава, “Деформирующий остеоартроз первого плюснефалангового сустава, или ригидный 1 палец стопы: клиника, диагностика и лечение (аналитический обзор литературы),” 2014.
M. D. Dujela, T. Langan, J. M. Cottom, W. T. DeCarbo, J. E. McAlister, and C. F. Hyer, “Lapidus Arthrodesis,” Clin Podiatr Med Surg, vol. 39, no. 2, pp. 187–206, Apr. 2022, doi: 10.1016/j.cpm.2021.11.009.
Д.В. Ильченко, “Хирургическое лечение третьей стадии Hallux rigidus, суставсберегающий подход и отдаленные результаты,” 2020.
T. R. Love, A. S. Whynot, I. Farine, M. Lavoie, L. Hunt, and A. Gross, “Keller Arthroplasty: A Prospective Review,” Foot Ankle, vol. 8, no. 1, pp. 46–54, Aug. 1987, doi: 10.1177/107110078700800110.
R. G. Taylor, “The treatment of claw toes by multiple transfers of flexor into extensor tendons,” J Bone Joint Surg Br, vol. 33-B, no. 4, pp. 539–542, Nov. 1951, doi: 10.1302/0301-620X.33B4.539.
K. Brevig and S. G. Barbari, “[Clawtoes treated by tendon transposition].,” Tidsskr Nor Laegeforen, vol. 105, no. 8, pp. 581–4, Mar. 1985.
Losa Iglesias , “Meta-analysis of Flexor Tendon Transfer for the Correction of Lesser Toe Deformities,” J Am Podiatr Med Assoc, vol. 102, no. 5, pp. 359–368, Sep. 2012, doi: 10.7547/1020359.
B. Baravarian, J. Thompson, and D. Nazarian, “Plantar Plate Tears: A Review of the Modified Flexor Tendon Transfer Repair for Stabilization,” Clin Podiatr Med Surg, vol. 28, no. 1, pp. 57–68, Jan. 2011, doi: 10.1016/j.cpm.2010.11.002.
Harold Kitaoka, Master Techniques in Orthopaedic Surgery: The Foot and Ankle. 2013.
C. Nery, M. J. Coughlin, D. Baumfeld, and T. S. Mann, “Lesser Metatarsophalangeal Joint Instability: Prospective Evaluation and Repair of Plantar Plate and Capsular Insufficiency,” Foot Ankle Int, vol. 33, no. 4, pp. 301–311, Apr. 2012, doi: 10.3113/FAI.2012.0301.
Бобров Д.С., “Перегрузочная метатарзалгия: патогенез, биомеханика и хирургическое лечение (аналитический обзор литературы),” Вестник РАМН, pp. 53–58, 2017.
M. J. Coughlin, “Lesser Toe Deformities,” Orthopedics, vol. 10, no. 1, pp. 63–75, Jan. 1987, doi: 10.3928/0147-7447-19870101-13.
T. Deltombe, T. Gavray, O. Van Roy, D. Wautier, and T. Gustin, “Medico-Surgical Management of the Spastic Equinovarus Foot Deformity in Adults: A Retrospective Series of 622 Patients,” J Int Soc Phys Rehabil Med, vol. 5, no. 4, pp. 156–160, Dec. 2022, doi: 10.4103/ijprm.JISPRM-000182.
V. Thamkunanon and N. Kamisan, “Approach to bone procedure in fixed equinovarus deformity in cerebral palsy,” J Orthop, vol. 15, no. 4, pp. 1008–1012, Dec. 2018, doi: 10.1016/j.jor.2018.09.001.
M. Lucas et al., “Outcomes of equinus/varus foot surgery in patients with spastic paresis: A retrospective study on 126 patients,” Ann Phys Rehabil Med, vol. 61, pp. e367–e368, Jul. 2018, doi: 10.1016/j.rehab.2018.05.853.
E. Allart, N. Sturbois-Nachef, M. Salga, C. Rosselin, L. Gatin, and F. Genêt, “Neuro-Orthopedic Surgery for Equinovarus Foot Deformity in Adults: A Narrative Review,” The Journal of Foot and Ankle Surgery, vol. 61, no. 3, pp. 648–656, May 2022, doi: 10.1053/j.jfas.2021.11.012.
S. Gursu et al., “Talectomy and Tibiocalcaneal Arthrodesis With Intramedullary Nail Fixation for Treatment of Equinus Deformity in Adults,” Foot Ankle Int, vol. 36, no. 1, pp. 46–50, Jan. 2015, doi: 10.1177/1071100714550649.
E. Giannotti, A. Merlo, P. Zerbinati, P. Prati, S. Masiero, and D. Mazzoli, “Safety and long-term effects on gait of hemiplegic patients in equinovarus foot deformity surgical correction followed by immediate rehabilitation: a prospective observational study,” Eur J Phys Rehabil Med, vol. 55, no. 2, May 2019, doi: 10.23736/S1973-9087.18.05290-5.
T. J. Boffeli, R. C. Collier, E. F. Neubauer, and D. S. Malay, “Surgical Outcomes After Minimally Invasive Release of Stroke-Related Equinovarus Contracture of the Foot and Ankle,” The Journal of Foot and Ankle Surgery, vol. 58, no. 6, pp. 1108–1117, Nov. 2019, doi: 10.1053/j.jfas.2019.01.019.
C. Ortiz and E. Wagner, “Tendon Transfers in Cavovarus Foot,” Foot Ankle Clin, vol. 19, no. 1, pp. 49–58, Mar. 2014, doi: 10.1016/j.fcl.2013.10.004.
I. A. Sarikaya, S. Ertan Birsel, A. Seker, O. A. Erdal, B. Gorgun, and M. Inan, “The split transfer of tibialis anterior tendon to peroneus tertius tendon for equinovarus foot in children with cerebral palsy,” Acta Orthop Traumatol Turc, vol. 54, no. 3, pp. 262–268, Jun. 2020, doi: 10.5152/j.aott.2020.03.571.
L. M. Fortier, M. Markel, B. G. Thomas, W. F. Sherman, B. H. Thomas, and A. D. Kaye, “An Update on Peroneal Nerve Entrapment and Neuropathy,” Orthop Rev (Pavia), vol. 13, no. 2, Jun. 2021, doi: 10.52965/001c.24937.
J. Souter, K. Swong, M. McCoyd, N. Balasubramanian, M. Nielsen, and V. C. Prabhu, “Surgical Results of Common Peroneal Nerve Neuroplasty at Lateral Fibular Neck,” World Neurosurg, vol. 112, pp. e465–e472, Apr. 2018, doi: 10.1016/j.wneu.2018.01.061.
D. Morimoto et al., “Microsurgical Decompression for Peroneal Nerve Entrapment Neuropathy,” Neurol Med Chir (Tokyo), vol. 55, no. 8, pp. 669–673, 2015, doi: 10.2176/nmc.oa.2014-0454.
B. S. Dhinsa, L. Hussain, and S. Singh, “The management of dorsal peroneal nerve compression in the midfoot,” The Foot, vol. 35, pp. 1–4, Jun. 2018, doi: 10.1016/j.foot.2017.12.005.
L. Head, K. Hicks, G. Wolff, and K. Boyd, “Clinical Outcomes of Nerve Transfers in Peroneal Nerve Palsy: A Systematic Review and Meta-Analysis,” J Reconstr Microsurg, vol. 35, no. 01, pp. 057–065, Jan. 2019, doi: 10.1055/s-0038-1667047.
K. M. Schweitzer and C. P. Jones, “Tendon Transfers for the Drop Foot,” Foot Ankle Clin, vol. 19, no. 1, pp. 65–71, Mar. 2014, doi: 10.1016/j.fcl.2013.12.002.
C. Jeng and M. Myerson, “The uses of tendon transfers to correct paralytic deformity of the foot and ankle,” Foot Ankle Clin, vol. 9, no. 2, pp. 319–337, Jun. 2004, doi: 10.1016/j.fcl.2004.03.003.
A. Elsner, A. Barg, S. A. Stufkens, and B. Hintermann, “Lambrinudi Arthrodesis with Posterior Tibialis Transfer in Adult Drop-Foot,” Foot Ankle Int, vol. 31, no. 1, pp. 30–37, Jan. 2010, doi: 10.3113/FAI.2010.0030.
Овечкин А.М., “Послеоперационное обезболивание. Клинические рекомендации ,” Вестник интенсивной терапии имени А. И. Салтанова. , 2019.
N. H. Waldron, C. A. Jones, T. J. Gan, T. K. Allen, and A. S. Habib, “Impact of perioperative dexamethasone on postoperative analgesia and side-effects: systematic review and meta-analysis,” Br J Anaesth, vol. 110, no. 2, pp. 191–200, Feb. 2013, doi: 10.1093/bja/aes431.
A. Coviello et al., “Dexamethasone versus Dexmedetomidine as Adjuvants in Ultrasound Popliteal Sciatic Nerve Block for Hallux Valgus Surgery: A Mono-Centric Retrospective Comparative Study,” Drug Des Devel Ther, vol. Volume 18, pp. 1231–1245, Apr. 2024, doi: 10.2147/DDDT.S442808.
“White Book on Physical and Rehabilitation Medicine in Europe. Introductions, Executive Summary, and Methodology,” Eur J Phys Rehabil Med, vol. 54, no. 2, Mar. 2018, doi: 10.23736/S1973-9087.18.05143-2.
Иванова Г.Е., “Как организовать медицинскую реабилитацию?”, Вестник восстановительной медицины, 2018.
Н.А. Амосова, “Лечебная физическая культура в системе медицинской реабилитации: национальное руководство,” Москва : Общество с ограниченной ответственностью Издательская группа “ГЭОТАР-Медиа,” 2022.
“Физиотерапия: национальное руководство,” М. : ГЭОТАР-Медиа, 2009.
Ушаков А.А., “Практическая физиотерапия,” М.: Медицинское информационное агентство, 2009.
R. Schuh, S. G. Hofstaetter, S. B. Adams, F. Pichler, K.-H. Kristen, and H.-J. Trnka, “Rehabilitation After Hallux Valgus Surgery: Importance of Physical Therapy to Restore Weight Bearing of the First Ray During the Stance Phase,” Phys Ther, vol. 89, no. 9, pp. 934–945, Sep. 2009, doi: 10.2522/ptj.20080375.
Д.В. Ильченко, “Методы реабилитации после оперативного лечения статических деформаций стопы,” Vestnik Of Experimental And Clinical Surgery, 2017.
L. Chen, L. Ye, H. Liu, P. Yang, and B. Yang, “Extracorporeal Shock Wave Therapy for the Treatment of Osteoarthritis: A Systematic Review and Meta‐Analysis,” Biomed Res Int, vol. 2020, no. 1, Jan. 2020, doi: 10.1155/2020/1907821.
K. Janczewska, R. Klimkiewicz, A. Kubsik-Gidlewska, A. Jankowska, P. Klimkiewicz, and M. Woldańska-Okońska, “[New physical methods in osteoarthritis treatment].,” Wiad Lek, vol. 70, no. 3 pt 2, pp. 644–648, 2017.
C. Wang, J. Ko, W. Chou, J. Cheng, and Y. Kuo, “Extracorporeal shockwave therapy for treatment of keloid scars,” Wound Repair and Regeneration, vol. 26, no. 1, pp. 69–76, Jan. 2018, doi: 10.1111/wrr.12610.
N. Gili, K. Micallef Stafrace, F. Laybats, and T. Mifsud, “The Role of Extracorporeal Shock Wave Therapy in Keloids and Hypertrophic Scars: A Systematic Review,” Cureus, Oct. 2024, doi: 10.7759/cureus.71869.
Lee JJ, Ricks TR, Garg S, Alegun JO, Li B, Klein LR, Caronia CG. Perioperative Antibiotic Choice Does Not Affect Wound Complications in the Operative Treatment of Ankle Fractures. Cureus. 2024 Nov 13;16(11):e73625. doi: 10.7759/cureus.73625.
Korwin-Kochanowska K, Potié A, El-Boghdadly K, et al. PROSPECT guideline for hallux valgus repair surgery: a systematic review and procedure-specific postoperative pain management recommendations. Reg Anesth Pain Med. 2020;45(9):702-708. doi: 10.1136/rapm-2020-101479,
Xie J, Zhu J, Xu Y, et al. Pain management of Hallux Valgus surgery is achieved by cocktail therapy. Evid Based Complement Alternat Med. 2022;2022:1084815. doi: 10.1155/2022/1084815,
Waldron N, Jones C, Gan T, et al. Impact of perioperative dexamethasone on postoperative analgesia and side-effects: systematic review and meta-analysis. Br J Anaesth. 2012;110:191–200
Hsu JR, Mir H, Wally MK, Seymour RB; Orthopaedic Trauma Association Musculoskeletal Pain Task Force. Clinical Practice Guidelines for Pain Management in Acute Musculoskeletal Injury. J Orthop Trauma. 2019;33(5):e158-e182. doi: 10.1097/BOT.0000000000001430].
Eyal Izak, Einat Kodesh Walking with unilateral ankle-foot unloading: a comparative biomechanical analysis of three assistive devices. J Neuroeng Rehabil 2024 Apr 30;21(1):67. doi: 10.1186/s12984-024-01333-w
Okamura K, Fukuda K, Oki S, Ono T, Tanaka S, Kanai S Gait Posture. 2020 Jan;75:40-45. doi: 10.1016/j.gaitpost.2019.09.030. Epub 2019 Sep 29.PMID: 31590069 Clinical Trial.
Goo YM, Kim TH, Lim JY J Phys Ther Sci. 2016 Mar;28(3):911-5. doi: 10.1589/jpts.28.911. Epub 2016 Mar 31.PMID: 27134383
Jung D, Yi C, Choi WJ, You JSH. Effect of dynamic guidance-tubing short foot gait exercise on muscle activity and navicular movement in people with flexible flatfeet. NeuroRehabilitation. 2020;47(2):217-226. doi: 10.3233/NRE-203106.PMID: 32741785
Huang C, Chen LY, Liao YH, Masodsai K, Lin YY. Int. J. Environ Res. Public Health. 2022 Sep 22;19(19):11994. doi: 10.3390/ijerph191911994.PMID: 36231295
Chul Hyun Park1, Min Cheol Chang Forefoot disorders and conservative treatment Affiliations Expand PMID: 31620619 PMCID: PMC6784640 DOI: 10.12701/yujm.2019.00185
Puszczałowska-Lizis E, Dąbrowiecki D, Jandziś S, Żak M. Foot Deformities in Women Are Associated with Wearing High-Heeled Shoes. Med Sci Monit. 2019 Oct 16;25:7746-7754. doi: 10.12659/MSM.917983.PMID: 31701921
P.M.C. Dearden, R. Ray, P.W. Robinson, et al. Clinical and Radiological Outcomes of Forefoot Offloading Versus Rigid Flat Shoes in Patients Undergoing Surgery of the First Ray // Foot and Ankle International. – 2019. – Vol. 40, № 10. – P. 1189-1194. – DOI: 10.1177/1071100719858621
Pfammatter C, Hambrecht J, Kalbas Y, Neuhaus V, Hierholzer C, Canal C. A single-centre, retrospective study on the impact of omitting preoperative antibiotic prophylaxis on wound infections in minor orthopedic implant removals. Eur J Trauma Emerg Surg. 2025 Feb 7;51(1):94.
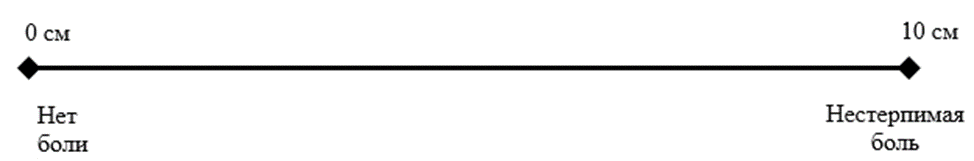 Ключ: ВАШ представляет собой линию 10 см (100 мм), на которой пациенту предлагается сделать отметку, соответствующую интенсивности боли, испытываемой в данный момент (или в течение определенного времени, например, за последнюю неделю), пациент делает выбор между «нет боли» и «невыносимая боль». Далее измеряют сантиметром расстояние между началом шкалы («нет боли») и отметкой пациента, сантиметры затем переводят в баллы (1 см = 10мм= 1 баллу).
Ключ: ВАШ представляет собой линию 10 см (100 мм), на которой пациенту предлагается сделать отметку, соответствующую интенсивности боли, испытываемой в данный момент (или в течение определенного времени, например, за последнюю неделю), пациент делает выбор между «нет боли» и «невыносимая боль». Далее измеряют сантиметром расстояние между началом шкалы («нет боли») и отметкой пациента, сантиметры затем переводят в баллы (1 см = 10мм= 1 баллу).