Petty RE, Laxer RM, Lindsley CB, et al. Textbook of pediatric rheumatology. 8th ed. Philadelphia: Elsevier, Inc 2020.
Баранов А.А., Алексеева Е.И., editors. Ревматические болезни у детей. Москва: ПедиатрЪ 2016.
Martini G, Foeldvari I, Russo R, et al. Systemic sclerosis in childhood: Clinical and immunologic features of 153 patients in an international database. Arthritis Rheum. 2006;54:3971–8. doi: 10.1002/art.22207
Volkmann ER. Systemic sclerosis. 2023;401.
Williams JN, Speyer CB, Kreps DJ, et al. Spinal cord syndromes in patients with systemic lupus erythematosus: differentiating lupus myelitis, neuromyelitis optica, and multiple sclerosis. Lupus. 2019;28:1656–62. doi: 10.1177/0961203319886103
Zulian F. Immunopathogenesis of Juvenile Systemic Sclerosis. Front Immunol. 2019;10.
Foeldvari I, Torok KS, Anton J, et al. Proposed Response Parameters for Twelve‐Month Drug Trial in Juvenile Systemic Sclerosis: Results of the Hamburg International Consensus Meetings. Arthritis Care Res. 2023;75:2453–62. doi: 10.1002/acr.25171
Foeldvari I, Klotsche J, Torok KS, et al. Are diffuse and limited juvenile systemic sclerosis different in clinical presentation? Clinical characteristics of a juvenile systemic sclerosis cohort. J Scleroderma Relat Disord. 2019;4:49–61. doi: 10.1177/2397198318790494
Scalapino K, Arkachaisri T, Lucas M, et al. Childhood onset systemic sclerosis: classification, clinical and serologic features, and survival in comparison with adult onset disease. J Rheumatol. 2006;33:1004–13.
Foeldvari I, Culpo R, Sperotto F, et al. Consensus-based recommendations for the management of juvenile systemic sclerosis. Rheumatology. 2021;60:1651–8. doi: 10.1093/rheumatology/keaa584
Zulian F. Scleroderma in Children. Pediatr Clin North Am. 2005;52:521–45. doi: 10.1016/j.pcl.2005.02.001
Brennan P, Silman A, Black C, et al. Reliability of skin involvement measures in scleroderma. Rheumatology. 1992;31:457–60. doi: 10.1093/rheumatology/31.7.457
Foeldvari I, Torok KS. Review for best practice in clinical rheumatology juvenile systemic sclerosis – Updates and practice points. Best Pract Res Clin Rheumatol. 2021;35:101688. doi: 10.1016/j.berh.2021.101688
Li SC, O’Neil KM, Higgins GC. Morbidity and Disability in Juvenile Localized Scleroderma: The Case for Early Recognition and Systemic Immunosuppressive Treatment. J Pediatr. 2021;234:245-256.e2. doi: 10.1016/j.jpeds.2021.01.068
Gyger G, Baron M. Systemic Sclerosis. Rheum Dis Clin N Am. 2015;41:459–73. doi: 10.1016/j.rdc.2015.04.007
Kedia S, Chhaparia A, Garg P. Gastro-intestinal involvement in systemic sclerosis. Indian J Rheumatol. 2017;12:156. doi: 10.4103/0973-3698.219088
Emmanuel A. Current management of the gastrointestinal complications of systemic sclerosis. Nat Rev Gastroenterol Hepatol. 2016;13:461–72. doi: 10.1038/nrgastro.2016.99
Bagri NK, Raj D, Kaur J, et al. Juvenile systemic sclerosis: experience from a tertiary care center from India. Rheumatol Int. 2017;37:1687–91. doi: 10.1007/s00296-017-3793-3
Wielosz E, Majdan M. Haematological abnormalities in systemic sclerosis. Rheumatology. 2020;58:162–6. doi: 10.5114/reum.2020.96655
Тепаев Р.Ф. Синдром диссеминированного внутрисосудистого свертывания у детей. Диагностика и лечение. Педиатрическая Фармакология 2010;7:27–31.
Rajagopal R, Thachil J, Monagle P. Disseminated intravascular coagulation in paediatrics. Arch Dis Child. 2017;102:187–93. doi: 10.1136/archdischild-2016-311053
Ameri A, Anderson CM, Smith JH, et al. Thromboembolic Complications in a Pediatric Patient Population: Treatment with Direct Oral Anticoagulants. Monitoring of Treatment Efficiency with D-Dimer Levels and Safety Profile By Thromboelastogram. Blood. 2021;138:4270–4270. doi: 10.1182/blood-2021-146948
Leak A, Patel KJ, Tuddenham EG, et al. Axillary vein thrombosis in adolescent onset systemic sclerosis. Ann Rheum Dis. 1990;49:557–9. doi: 10.1136/ard.49.7.557
Клинический протокол. Ювенильный системный склероз URL: https://diseases.medelement.com/disease/ювенильный-системный-склероз/14875?ysclid=mcn36s8koe931448244.
Klein A, Molad Y. Hematological Manifestations among Patients with Rheumatic Diseases. Acta Haematol. 2021;144:403–12. doi: 10.1159/000511759
Monagle P, Chan AKC, Goldenberg NA, et al. Antithrombotic therapy in neonates and children: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e737S-e801S. doi: 10.1378/chest.11-2308
Tarango C, Manco-Johnson MJ. Pediatric Thrombolysis: A Practical Approach. Front Pediatr. 2017;5:260. doi: 10.3389/fped.2017.00260
Manco-Johnson MJ. How I treat venous thrombosis in children. Blood. 2006;107:21–9. doi: 10.1182/blood-2004-11-4211
Sepúlveda M P, Salgado U A, Barriga G J, et al. Usefulness of the thromboelastogram in children: correlation with habitual coagulation tests. Rev Chil Pediatr. 2019;90:617–23. doi: 10.32641/rchped.v90i6.930
Геморрагические и тромботические заболевания и синдромы у детей и подростков: патогенез, клиника, диагностика, терапия и профилактика : монография / Б.И. Кузник, В.Г. Стуров, Н.Ю. Левшин [и др.]. – 2-е изд., перераб. и доп. – Новосибирск : Наука, 2018. – 524 с.
Современные аспекты гемостазиологической диагностики у детей с тромбогеморрагическими осложнениями / А.А. Мартынов [и др.] // Практика педиатра. 2024. № 3. С. 53-60.
Тромбоэластография в клинической практике и диагностике: Методические рекомендации / Сыздыкова Б.С., Куанышев Е.Н. // Астана: АО «Национальный центр нейрохирургии», 2024. – 40с.
Montagnana M, Lippi G, Volpe A, et al. Evaluation of cardiac laboratory markers in patients with systemic sclerosis. Clin Biochem. 2006;39:913–7. doi: 10.1016/j.clinbiochem.2006.03.016
Breda, L., Nozzi, M., De Sanctis, S., & Chiarelli, F. (2010). Laboratory Tests in the Diagnosis and Follow-Up of Pediatric Rheumatic Diseases: An Update. Seminars in Arthritis and Rheumatism, 40(1), 53–72. doi:10.1016/j.semarthrit.2008.12.
Jeong JE, Kim SH. Clinical characteristics of juvenile systemic sclerosis in Korea: 31-year single-center study. J Rheum Dis. 2024;31:25–32. doi: 10.4078/jrd.2023.0046
Hachulla E, Agard C, Allanore Y, et al. French recommendations for the management of systemic sclerosis. Orphanet J Rare Dis. 2021;16:322. doi: 10.1186/s13023-021-01844-y
Hanson V, Kornreich HK, Drexler E, et al. Some Immunologic Considerations in Focal Scleroderma and Progressive Systemic Sclerosis in Children. Pediatr Res. 1974;8:806–9. doi: 10.1203/00006450-197409000-00006
Zulian F, Lanzoni G, Castaldi B, et al. Systemic sclerosis sine scleroderma in children. Rheumatology. 2022;61:2555–62. doi: 10.1093/rheumatology/keab738
Russo RA, Katsicas MM. Clinical characteristics of children with Juvenile Systemic Sclerosis: follow-up of 23 patients in a single tertiary center. Pediatr Rheumatol. 2007;5:6. doi: 10.1186/1546-0096-5-6
Jacquel L, Bechara R, Terzic J, et al. An updated overview of Juvenile systemic sclerosis in a French cohort. Pediatr Rheumatol. 2025;23:13. doi: 10.1186/s12969-024-01043-6
Михельсон В.А., В.А. Сидоров, and С.М. Степаненко. “Анестезия и интенсивная терапия в педиатрии.” М.:«Дель рус (2007).
Голуб И.Е.., Сорокина Л.В. Избранные вопросы по общей анестезиологии (методические рекомендации для клинических ординаторов, с правом переиздания). – 2005.
Handa R, Upadhyaya S, Kapoor S, et al. Tuberculosis and biologics in rheumatology: A special situation. Int J Rheum Dis. 2017;20:1313–25. doi: 10.1111/1756-185X.13129
Cantini F, Nannini C, Niccoli L, et al. Guidance for the management of patients with latent tuberculosis infection requiring biologic therapy in rheumatology and dermatology clinical practice. Autoimmun Rev. 2015;14:503–9. doi: 10.1016/j.autrev.2015.01.011
Овсянкина Е.С, Губкина М.Ф., Панова Л.В., Юхименко Н.В. Методы скрининга туберкулезной инфекции у детей и их роль в формировании групп риска и диагностике заболевания. Российский педиатрический журнал. 2017; 20 (2): 108-115. DOI: http://dx.doi.org/10.18821/1560-9561-2017-20 (2): 108-115.
Aksenova VA, Klevno NI, Kazakov AV, et al. Preventive Tuberculosis Services Reduces the Risk of Local Forms of Tuberculosis Development in Children on Immunosuppressive Therapy: Retrospective Cohort Study. Curr Pediatr. 2020;19:346–51. doi: 10.15690/vsp.v19i5.2210
Clemente D, Cuadros EN, Lovillo MC, et al. Position statement on infection screening, prophylaxis, and vaccination of pediatric patients with rheumatic diseases and immunosuppressive therapies, part 3: precautions in situations of surgery, fever, and opportunistic infections. Eur J Pediatr. 2023;183:915–27. doi: 10.1007/s00431-023-05295-4
Kwiatkowska B, Filipowicz‑Sosnowska A. Reactive arthritis. Pol Arch Intern Med. 2009;119:60–6. doi: 10.20452/pamw.606
Allen V, Longley N. Infections in immunosuppressed travellers with autoimmune inflammatory diseases—a narrative review and advice for clinical practice. Rheumatology. 2021;60:3969–76. doi: 10.1093/rheumatology/keab445
Whyte LA, Al-Araji RA, McLoughlin LM. Guidelines for the management of acute gastroenteritis in children in Europe. Arch Dis Child - Educ Pract Ed. 2015;100:308–12. doi: 10.1136/archdischild-2014-307253
Bockemühl J, Roggentin P. Enterale Yersiniosen. Klinische Bedeutung, Epidemiologie, Diagnostik und Prävention [Intestinal yersiniosis. Clinical importance, epidemiology, diagnosis, and prevention]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2004 Jul;47(7):685-91
Shi T, Huang L, Tian J. Prevalence of Epstein-Barr Viral DNA among children at a single hospital in Suzhou, China. J Pediatr (Rio J). 2022;98:142–6. doi: 10.1016/j.jped.2021.05.006
Soon GS, Laxer RM. Approach to recurrent fever in childhood. Can Fam Physician Med Fam Can. 2017;63:756–62.
Houen G, Trier NH. Epstein-Barr Virus and Systemic Autoimmune Diseases. Front Immunol. 2021;11:587380. doi: 10.3389/fimmu.2020.587380
Engelmann I, Petzold DR, Kosinska A, et al. Rapid quantitative PCR assays for the simultaneous detection of herpes simplex virus, varicella zoster virus, cytomegalovirus, Epstein-Barr virus, and human herpesvirus 6 DNA in blood and other clinical specimens. J Med Virol. 2008;80:467–77. doi: 10.1002/jmv.21095
Liu Z, Zhang P, Tang S, et al. Urine real-time polymerase chain reaction detection for children virus pneumonia with acute human cytomegalovirus infection. BMC Infect Dis. 2014;14:245. doi: 10.1186/1471-2334-14-245
A. Ross S, Novak Z, Pati S, et al. Overview of the Diagnosis of Cytomegalovirus Infection. Infect Disord - Drug Targets. 2011;11:466–74. doi: 10.2174/187152611797636703
Slots J, Slots H. Bacterial and viral pathogens in saliva: disease relationship and infectious risk. Periodontol 2000. 2011;55:48–69. doi: 10.1111/j.1600-0757.2010.00361.x
Strick LB, Wald A. Diagnostics for Herpes Simplex Virus: Is PCR the New Gold Standard? Mol Diagn Ther. 2006;10:17–28. doi: 10.1007/BF03256439
Vince A, Dusek D. Imunosupresija i virusne infekcije u reumatskim bolestima [Immunosupression and viral infections in rheumatic diseases]. Reumatizam. 2007;54(2):58-62. Croatian. PMID: 18351141.
Eisenstein EM, Wolf DG. Cytomegalovirus infection in pediatric rheumatic diseases: a review. Pediatr Rheumatol. 2010;8:17. doi: 10.1186/1546-0096-8-17
Looker KJ, Magaret AS, May MT, et al. Global and Regional Estimates of Prevalent and Incident Herpes Simplex Virus Type 1 Infections in 2012. PLOS ONE. 2015;10:e0140765. doi: 10.1371/journal.pone.0140765
McQuillan G, Kruszon-Moran D, Flagg EW, et al. Prevalence of Herpes Simplex Virus Type 1 and Type 2 in Persons Aged 14-49: United States, 2015-2016. NCHS Data Brief. 2018;1–8.
Xu F, Lee FK, Morrow RA, et al. Seroprevalence of Herpes Simplex Virus Type 1 in Children in the United States. J Pediatr. 2007;151:374–7. doi: 10.1016/j.jpeds.2007.04.065
Levin MJ, Weinberg A, Schmid DS. Herpes Simplex Virus and Varicella-Zoster Virus. Microbiol Spectr. 2016;4:4.3.49. doi: 10.1128/microbiolspec.DMIH2-0017-2015
Indolfi G, Easterbrook P, Dusheiko G, et al. Hepatitis B virus infection in children and adolescents. Lancet Gastroenterol Hepatol. 2019;4:466–76. doi: 10.1016/S2468-1253(19)30042-1
Mack CL, Adams D, Assis DN, et al. Diagnosis and Management of Autoimmune Hepatitis in Adults and Children: 2019 Practice Guidance and Guidelines From the American Association for the Study of Liver Diseases. Hepatology. 2020;72:671–722. doi: 10.1002/hep.31065
Indolfi G, Easterbrook P, Dusheiko G, et al. Hepatitis C virus infection in children and adolescents. Lancet Gastroenterol Hepatol. 2019;4:477–87. doi: 10.1016/S2468-1253(19)30046-9
Lampertico P, Agarwal K, Berg T, et al. EASL 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection. J Hepatol. 2017;67:370–98. doi: 10.1016/j.jhep.2017.03.021
Key recommendations. WHO Recommendations on the Diagnosis of HIV Infection in Infants and Children. World Health Organization 2010.
Okong׳o LO, Webb K, Scott C. HIV-associated juvenile systemic sclerosis: A case report. Semin Arthritis Rheum. 2015;44:411–6. doi: 10.1016/j.semarthrit.2014.08.005
Reust CE. Evaluation of primary immunodeficiency disease in children. Am Fam Physician. 2013;87:773–8.
Villard O, Cimon B, L’Ollivier C, et al. Serological diagnosis of Toxoplasma gondii infection. Diagn Microbiol Infect Dis. 2016;84:22–33. doi: 10.1016/j.diagmicrobio.2015.09.009
Cascio A., Colomba C. Childhood Mediterranean visceral leishmaniasis //Le Infezioni in Medicina. – 2003. – Т. 11. – №. 1. – С. 5-10.
Limper M, de Kruif MD, Duits AJ, et al. The diagnostic role of Procalcitonin and other biomarkers in discriminating infectious from non-infectious fever. J Infect. 2010;60:409–16. doi: 10.1016/j.jinf.2010.03.016
Kim YW, Kwon BS, Lim SY, et al. Diagnostic value of bronchoalveolar lavage and bronchial washing in sputum-scarce or smear-negative cases with suspected pulmonary tuberculosis: a randomized study. Clin Microbiol Infect. 2020;26:911–6. doi: 10.1016/j.cmi.2019.11.013
Barahona-Correa JE, De La Hoz A, López MJ, et al. Infections and systemic sclerosis: an emerging challenge. Rev Colomb Reumatol Engl Ed. 2020;27:62–84. doi: 10.1016/j.rcreue.2019.12.004
Fioretto JR, Borin FDC, Bonatto RC, et al. Procalcitonin in children with sepsis and septic shock. J Pediatr (Rio J). 2004;0. doi: 10.2223/JPED.1644
Fioretto JR, Martin JG, Kurokawa CS, et al. Comparison between procalcitonin and C-reactive protein for early diagnosis of children with sepsis or septic shock. Inflamm Res. 2010;59:581–6. doi: 10.1007/s00011-010-0161-0
Sakkas LI, Simopoulou T, Daoussis D, et al. Intestinal Involvement in Systemic Sclerosis: A Clinical Review. Dig Dis Sci. 2018;63:834–44. doi: 10.1007/s10620-018-4977-8
Robinson JL, Lee BE, Kothapalli S, et al. Use of Throat Swab or Saliva Specimens for Detection of Respiratory Viruses in Children. Clin Infect Dis. 2008;46:e61–4. doi: 10.1086/529386
Chien Y-L, Huang F-L, Huang C-M, et al. Clinical approach to fever of unknown origin in children. J Microbiol Immunol Infect. 2017;50:893–8. doi: 10.1016/j.jmii.2015.08.007
Ahmadinejad Z, Mansori S, Ziaee V, et al. Periodic Fever: a review on clinical, management and guideline for Iranian patients - part I. Iran J Pediatr 2014;24:1–13.
Weiss SL, Peters MJ, Alhazzani W, et al. Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Intensive Care Med. 2020;46:10–67. doi: 10.1007/s00134-019-05878-6
Howell MD, Davis AM. Management of Sepsis and Septic Shock. 2017;2.
Ören H, Cingöz I, Duman M, et al. Disseminated intravascular coagulation in pediatric patients: Clinical and Laboratory Features and Prognostic Factors Influencing the Survival. Pediatr Hematol Oncol. 2005;22:679–88. doi: 10.1080/08880010500278749
Misra R, Singh G, Aggarwal P, et al. Juvenile onset systemic sclerosis: a single center experience of 23 cases from Asia. Clin Rheumatol. 2007;26:1259–62. doi: 10.1007/s10067-006-0483-z
Panigada S, Ravelli A, Silvestri M, et al. HRCT and pulmonary function tests in monitoring of lung involvement in juvenile systemic sclerosis. Pediatr Pulmonol. 2009;44:1226–34. doi: 10.1002/ppul.21141
Takagi Y, Sasaki M, Eida S, et al. Comparison of salivary gland MRI and ultrasonography findings among patients with Sjögren’s syndrome over a wide age range. Rheumatology. 2022;61:1986–96. doi: 10.1093/rheumatology/keab560
Afzelius P, Nielsen M, Ewertsen C, et al. Imaging of the major salivary glands. Clin Physiol Funct Imaging. 2016;36:1–10. doi: 10.1111/cpf.12199
Pavlov‐Dolijanović S, Damjanov N, Ostojić P, et al. The Prognostic Value of Nailfold Capillary Changes for the Development of Connective Tissue Disease in Children and Adolescents with Primary Raynaud Phenomenon: A Follow‐up Study of 250 Patients. Pediatr Dermatol. 2006;23:437–42. doi: 10.1111/j.1525-1470.2006.00278.x
Pavlov-Dolijanovic S, Damjanov NS, Stojanovic RM, et al. Scleroderma pattern of nailfold capillary changes as predictive value for the development of a connective tissue disease: a follow-up study of 3,029 patients with primary Raynaud’s phenomenon. Rheumatol Int. 2012;32:3039–45. doi: 10.1007/s00296-011-2109-2
Navallas M, Inarejos Clemente EJ, Iglesias E, et al. Connective Tissue Disorders in Childhood: Are They All the Same? RadioGraphics. 2019;39:229–50. doi: 10.1148/rg.2019180078
Chapin R, Hant FN. Imaging of Scleroderma. Rheum Dis Clin N Am. 2013;39:515–46. doi: 10.1016/j.rdc.2013.02.017
Boutry N, Hachulla É, Zanetti-Musielak C, et al. Imaging features of musculoskeletal involvement in systemic sclerosis. Eur Radiol. 2007;17:1172–80. doi: 10.1007/s00330-006-0420-1
Ambartsumyan L, Zheng HB, Iyer RS, et al. Relationship Between Esophageal Abnormalities on Fluoroscopic Esophagram and Pulmonary Function Testing in Juvenile Systemic Sclerosis. Arthritis Care Res. 2019;71:1444–9. doi: 10.1002/acr.23778
Júnior JG, Mugii N, Inaoka PT, et al. Inflammatory myopathies overlapping with systemic sclerosis: a systematic review. Clin Rheumatol. 2022;41:1951–63. doi: 10.1007/s10067-022-06115-0
Danaoui K, Nassih H, Oujennane K, et al. Juvenile Systemic Sclerosis: About 9 Cases. Open J Pediatr. 2024;14:320–6. doi: 10.4236/ojped.2024.142031
Popescu NA, Manea D, Capitanescu G, et al. Respiratory Failure in a Rare Case of Juvenile Dermatomyositis - Systemic Scleroderma Overlap Syndrome. Maedica. 2020;15:394–400. doi: 10.26574/maedica.2020.15.3.394
Houssini G. S. et al. Juvenile overlap syndrome: Considering scleromyositis //J Clin Images Med Case Rep. – 2024. – Т. 5. – №. 4. – С. 2988.
Ruemmele FM, Veres G, Kolho KL, et al. Consensus guidelines of ECCO/ESPGHAN on the medical management of pediatric Crohn’s disease. J Crohns Colitis. 2014;8:1179–207. doi: 10.1016/j.crohns.2014.04.005
Turner D, Ruemmele FM, Orlanski-Meyer E, et al. Management of Paediatric Ulcerative Colitis, Part 1: Ambulatory Care—An Evidence-based Guideline From European Crohn’s and Colitis Organization and European Society of Paediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2018;67:257–91. doi: 10.1097/MPG.0000000000002035
Sierra D, Wood M, Kolli S, et al. Pediatric Gastritis, Gastropathy, and Peptic Ulcer Disease. Pediatr Rev. 2018;39:542–9. doi: 10.1542/pir.2017-0234
Tutar E, Kutluk G, Bayrak NA, et al. What is the diagnostic utility of endoscopic scoring systems in children? Turk J Gastroenterol. 2009;24:22–9. doi: 10.4318/tjg.2013.0700
Kröner PT, Tolaymat OA, Bowman AW, et al. Gastrointestinal Manifestations of Rheumatological Diseases. Am J Gastroenterol. 2019;114:1441–54. doi: 10.14309/ajg.0000000000000260
Kaniecki T, Abdi T, McMahan ZH. A practical approach to the evaluation and management of gastrointestinal symptoms in patients with systemic sclerosis. Best Pract Res Clin Rheumatol. 2021;35:101666. doi: 10.1016/j.berh.2021.101666
Gillett P, Hassall E. Pediatric gastrointestinal mucosal biopsy. Special considerations in children. Gastrointest Endosc Clin N Am. 2000;10:669–712, vi–vii.
Tringali A, Thomson M, Dumonceau J-M, et al. Pediatric gastrointestinal endoscopy: European Society of Gastrointestinal Endoscopy (ESGE) and European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) Guideline Executive summary. Endoscopy. 2016;49:83–91. doi: 10.1055/s-0042-111002
Păduraru, Gabriela, et al. “Digestive hemorrhage in pediatric pathology.” Romanian Journal of Pediatrics 61.3 (2012).
Foeldvari I. Juvenile Systemic Sclerosis. In: Sawhney S, Aggarwal A, eds. Pediatric Rheumatology. Singapore: Springer Singapore 2017:403–11.
Cimaz, Rolando, and Thomas JA Lehman, eds. Pediatrics in systemic autoimmune diseases. Elsevier, 2016.
Zulian F. Scleroderma in children. Best Pract Res Clin Rheumatol. 2017;31:576–95. doi: 10.1016/j.berh.2018.02.004
Allen-Rhoades W, Whittle SB, Rainusso N. Pediatric Solid Tumors in Children and Adolescents: An Overview. Pediatr Rev. 2018;39:444–53. doi: 10.1542/pir.2017-0268
García-Basteiro AL, DiNardo A, Saavedra B, et al. Point of care diagnostics for tuberculosis. Pulmonology. 2018;24:73–85. doi: 10.1016/j.rppnen.2017.12.002
Kowal-Bielecka O, Landewé R, Avouac J, et al. EULAR recommendations for the treatment of systemic sclerosis: a report from the EULAR Scleroderma Trials and Research group (EUSTAR). Ann Rheum Dis. 2009;68:620–8. doi: 10.1136/ard.2008.096677
Fonseca MB, Gomes FHR, Valera ET, et al. Signs and symptoms of rheumatic diseases as first manifestation of pediatric cancer: diagnosis and prognosis implications. Rev Bras Reumatol Engl Ed. 2017;57:330–7. doi: 10.1016/j.rbre.2017.01.007
Alias A, Rodriguez EJ, Bateman HE, et al. Rheumatology and oncology: an updated review of rheumatic manifestations of malignancy and anti-neoplastictherapy. Bull NYU Hosp Jt Dis. 2012;70:109–14.
Department of Radiology, National Institute of Geriatrics, Rheumatology and Rehabilitation, Warsaw, Poland, Idzior M, Sotniczuk M, et al. Ultrasonography, MRI and classic radiography of skin and MSK involvement in juvenile scleroderma. J Ultrason. 2020;20:311–7. doi: 10.15557/JoU.2020.0054
Loctin A, Bailly F, Laroche D, et al. Clinical interest of bone marrow aspiration in rheumatology: a practice-based observational study of 257 bone marrow aspirations. Clin Rheumatol. 2013;32:115–21. doi: 10.1007/s10067-012-2097-y
Zucker EJ, Lee EY, Restrepo R, et al. Hip Disorders in Children. Am J Roentgenol. 2013;201:W776–96. doi: 10.2214/AJR.13.10623
Li Q. et al. Quantifying the contribution of 18F-FDG PET to the diagnostic assessment of pediatric patients with fever of unknown origin: a systematic review and meta-analysis //Pediatric Radiology. – 2022. – С. 1-12.
Colamussi P, Prandini N, Cittanti C, et al. Scintigraphy in rheumatic diseases. Best Pract Res Clin Rheumatol. 2004;18:909–26. doi: 10.1016/j.berh.2004.07.003
Ćwikła JB. New imaging techniques in reumathology: MRI, scintigraphy and PET. Pol J Radiol. 2013;78:48–56. doi: 10.12659/PJR.889138
Grebenyuk V. et al. Fever of unknown origin: case reports from routine clinical practice and a review //Klinicka Mikrobiologie a Infekcni Lekarstvi. – 2021. – Т. 27. – №. 4. – С. 148-157.
Mozolová D, Rovenský J, Sipeki T. From “Sine Syndrome” to Sjögren’s Syndrome. In: Rovenský J, Herold M, Vašáková M, eds. Sine Syndromes in Rheumatology. Vienna: Springer Vienna 2014:31–6.
Lepri G, Catalano M, Bellando-Randone S, et al. Systemic Sclerosis Association with Malignancy. Clin Rev Allergy Immunol. 2022;63:398–416. doi: 10.1007/s12016-022-08930-4
Аксенова В.А., Барышников Л.А., Клевно Н.И., et al. Новые возможности скрининга и диагностики различных проявлений туберкулезной инфекции у детей и подростков в России. Вопросы Современной Педиатрии 2011;10:16–22.
Borowiec A, Dabrowski R, Wozniak J, et al. Cardiovascular assessment of asymptomatic patients with juvenile-onset localized and systemic scleroderma: 10 years prospective observation. Scand J Rheumatol. 2012;41:33–8. doi: 10.3109/03009742.2011.609489
Yuen, L. K., et al. “Case Report Two Cases of Juvenile Systemic Sclerosis and Literature Review.” HK J Paediatr (New Series) 12.3 (2007): 221-226.
Ocallaghan C. Renal manifestations of systemic autoimmune disease: diagnosis and therapy. Best Pract Res Clin Rheumatol. 2004;18:411–27. doi: 10.1016/j.berh.2004.03.002
Hashkes PJ, Laxer RM, Simon A, editors. Textbook of Autoinflammation. Cham: Springer International Publishing 2019.
Gualtierotti R, Parisi M, Ingegnoli F. Perioperative Management of Patients with Inflammatory Rheumatic Diseases Undergoing Major Orthopaedic Surgery: A Practical Overview. Adv Ther. 2018;35:439–56. doi: 10.1007/s12325-018-0686-0
Röher K, Trieschmann U, Leister N. Anästhesie und Analgosedierung für diagnostische Eingriffe bei Kindern. AINS - Anästhesiol · Intensivmed · Notfallmedizin · Schmerzther. 2023;58:409–20. doi: 10.1055/a-1925-7009
Dumas G, Arabi YM, Bartz R, et al. Diagnosis and management of autoimmune diseases in the ICU. Intensive Care Med. 2024;50:17–35. doi: 10.1007/s00134-023-07266-7
Janssen NM, Karnad DR, Guntupalli KK. Rheumatologic diseases in the intensive care unit: epidemiology, clinical approach, management, and outcome. Crit Care Clin. 2002;18:729–48. doi: 10.1016/S0749-0704(02)00025-8
Frye WS, Milojevic D. The Role of Psychology in Pediatric Rheumatic Diseases. Pediatr Clin North Am. 2022;69:965–74. doi: 10.1016/j.pcl.2022.05.009
Foeldvari I, Torok KS, Antón J, et al. Best clinical practice in the treatment of juvenile systemic sclerosis: expert panel guidance - the result of the International Hamburg Consensus Meeting December 2022. Expert Rev Clin Immunol. 2024;20:387–404. doi: 10.1080/1744666X.2023.2298354
Zulian F, Martini G. Childhood systemic sclerosis. Curr Opin Rheumatol. 2007;19:592–7. doi: 10.1097/BOR.0b013e3282f01625
Van Den Hoogen F, Khanna D, Fransen J, et al. 2013 Classification Criteria for Systemic Sclerosis: An American College of Rheumatology/European League Against Rheumatism Collaborative Initiative. Arthritis Rheum. 2013;65:2737–47. doi: 10.1002/art.38098
Koç R, Sönmez HE, Çakan M, et al. Drug reactions in children with rheumatic diseases receiving parenteral therapies: 9 years’ experience of a tertiary pediatric rheumatology center. Rheumatol Int. 2020;40:771–6. doi: 10.1007/s00296-019-04498-z
Lehrnbecher T, Groll AH. Infectious complications in the paediatric immunocompromised host: a narrative review. Clin Microbiol Infect. 2025;31:37–42. doi: 10.1016/j.cmi.2024.06.002
Bula-Rudas FJ, Rathore MH, Maraqa NF. Salmonella Infections in Childhood. Adv Pediatr. 2015;62:29–58. doi: 10.1016/j.yapd.2015.04.005
Daloglu H. Childhood Chlamydia Infections. In: Sarier M, ed. Infectious Diseases. IntechOpen 2023.
Weyant RB, Kabbani D, Doucette K, et al. Pneumocystis jirovecii: a review with a focus on prevention and treatment. Expert Opin Pharmacother. 2021;22:1579–92. doi: 10.1080/14656566.2021.1915989
Eroglu‐Ertugrul NG, Yalcin E, Oguz B, et al. The value of flexible bronchoscopy in pulmonary infections of immunosuppressed children. Clin Respir J. 2020;14:78–84. doi: 10.1111/crj.13103
Ers. Bronchoalveolar lavage in children. Eur Respir J. 2000;15:217–31. doi: 10.1183/09031936.00.15121700
Daelemans, Siel & Peeters, Linde & Wachter, Elke & Malfroot, Anne. (2019). Challenges in Diagnosing Mycobacterial Infections in Children.. 21. 194-199.
Xu D, Li S, Chen Z, et al. Detection of Mycoplasma pneumoniae in different respiratory specimens. Eur J Pediatr. 2011;170:851–8. doi: 10.1007/s00431-010-1360-y
Copete AR, Vera C, Herrera M, et al. Mycoplasma pneumoniae in Children With and Without Community-acquired Pneumonia. What do PCR and Serology Say? Pediatr Infect Dis J. 2020;39:e104–8. doi: 10.1097/INF.0000000000002636
Restrepo-Gualteros SM, Gutierrez MJ, Villamil-Osorio M, et al. Challenges and Clinical Implications of the Diagnosis of Cytomegalovirus Lung Infection in Children. Curr Infect Dis Rep. 2019;21:24. doi: 10.1007/s11908-019-0681-x
Gonski K, Cohn R, Widger J, et al. Utility of bronchoscopy in immunocompromised paediatric patients: Systematic review. Paediatr Respir Rev. 2020;34:24–34. doi: 10.1016/j.prrv.2020.02.003
Özkoç S, Bayram Deli̇Baş S. Investigation of Pneumocystis jirovecii Pneumonia and Colonization in Iatrogenically Immunosuppressed and Immunocompetent Patients. Mikrobiyol Bul. 2015;49:221–30. doi: 10.5578/mb.9344
Lachant DJ, Croft DP, McGrane Minton H, et al. The clinical impact of pneumocystis and viral PCR testing on bronchoalveolar lavage in immunosuppressed patients. Respir Med. 2018;145:35–40. doi: 10.1016/j.rmed.2018.10.021
Ramos JT, Romero CA, Belda S, et al. Clinical practice update of antifungal prophylaxis in immunocompromised children. Rev Espanola Quimioter Publicacion Of Soc Espanola Quimioter 2019;32:410–25.
Tragiannidis A, Kyriakidis I, Zündorf I, et al. Invasive fungal infections in pediatric patients treated with tumor necrosis alpha (TNF-α) inhibitors. Mycoses. 2017;60:222–9. doi: 10.1111/myc.12576
Tan TC, Noviani M, Leung YY, et al. The microbiome and systemic sclerosis: A review of current evidence. Best Pract Res Clin Rheumatol. 2021;35:101687. doi: 10.1016/j.berh.2021.101687
Barola S., Grossman O. K., Abdelhalim A. Urinary tract infections in children //StatPearls [Internet]. – StatPearls Publishing, 2024.
Lazzerini PE, Capecchi PL, Guideri F, et al. Comparison of Frequency of Complex Ventricular Arrhythmias in Patients With Positive Versus Negative Anti-Ro/SSA and Connective Tissue Disease. Am J Cardiol. 2007;100:1029–34. doi: 10.1016/j.amjcard.2007.04.048
Zulian F, Balzarin M, Birolo C. Recent advances in the management of juvenile systemic sclerosis. Expert Rev Clin Immunol. 2017;13:361–9. doi: 10.1080/1744666X.2017.1243467
Galindo-Zavala R, Bou-Torrent R, Magallares-López B, et al. Expert panel consensus recommendations for diagnosis and treatment of secondary osteoporosis in children. Pediatr Rheumatol. 2020;18:20. doi: 10.1186/s12969-020-0411-9
Buckley L, Guyatt G, Fink HA, et al. 2017 American College of Rheumatology Guideline for the Prevention and Treatment of Glucocorticoid-Induced Osteoporosis: ACR guideline for glucocorticoid-induced osteoporosis prevention and treatment. Arthritis Rheumatol. 2017;69:1521–37. doi: 10.1002/art.40137
Athreya, Balu H., and Carol B. Lindsley. “Managing children with rheumatic diseases.” Textbook of Pediatric Rheumatology E-Book (2010): 168.
Fc A. The Portuguese Society of Rheumatology position paper on the use of biosimilars – 2017 update. 2017.
Atzeni F, Sebastiani M, Ricci C, et al. Position paper of Italian rheumatologists on the use of biosimilar drugs.
Abad Hernández MÁ, Andreu JL, Caracuel Ruiz MÁ, et al. Position Paper From the Spanish Society of Rheumatology on Biosimilar Drugs. Reumatol Clínica Engl Ed. 2015;11:269–78. doi: 10.1016/j.reumae.2015.03.012
Huizinga TWJ, Torii Y, Muniz R. Adalimumab Biosimilars in the Treatment of Rheumatoid Arthritis: A Systematic Review of the Evidence for Biosimilarity. Rheumatol Ther. 2021;8:41–61. doi: 10.1007/s40744-020-00259-8
Dills R, Anderson LA, Pierce CA. The role of nonsteroidal anti-inflammatory drugs in pediatric patients. Pharmacol Res. 2012;65:5–8. doi: 10.1016/j.phrs.2011.08.010
Sherman JM, Sood SK. Current challenges in the diagnosis and management of fever. Curr Opin Pediatr. 2012;24:400–6. doi: 10.1097/MOP.0b013e32835333e3
Баранов А.А., Алексеева Е.И., editors. Ревматические болезни у детей. Москва: : ПедиатрЪ 2016.
Gupta P, Sachdev HP. Safety of oral use of nimesulide in children: systematic review of randomized controlled trials. Indian Pediatr. 2003 Jun;40(6):518-31. PMID: 12824661.
Guillaume-Czitrom S. Les anti-inflammatoires non stéroïdiens dans les rhumatismes inflammatoires chroniques de l’enfant [Non -steroidal anti-inflammatory drugs in chronic inflammatory arthritis in children]. La Lettre du Rhumatologue №379-380 - février-mars 2012.
Алексеева Е., Валиева С. Оценка эффективности, переносимости и безопасности нимесулида у детей с ювенильным артритом. Вопросы современной педиатрии. 2007;6(6):76-80.
Fernández‐Codina A, Walker KM, Pope JE, et al. Treatment Algorithms for Systemic Sclerosis According to Experts. Arthritis Rheumatol. 2018;70:1820–8. doi: 10.1002/art.40560
Hoyles RK, Ellis RW, Wellsbury J, et al. A multicenter, prospective, randomized, double-blind, placebo-controlled trial of corticosteroids and intravenous cyclophosphamide followed by oral azathioprine for the treatment of pulmonary fibrosis in scleroderma. Arthritis Rheum. 2006;54:3962–70. doi: 10.1002/art.22204
Zulian F, Tirelli F. Treatment in Juvenile Scleroderma. Curr Rheumatol Rep. 2020;22:45. doi: 10.1007/s11926-020-00910-x
Zulian F, Vallongo C, Patrizi A, et al. A long-term follow-up study of methotrexate in juvenile localized scleroderma (morphea). J Am Acad Dermatol. 2012;67:1151–6. doi: 10.1016/j.jaad.2012.03.036
Hashkes PJ, Becker ML, Cabral DA, et al. Methotrexate: new uses for an old drug. J Pediatr. 2014;164:231–6. doi: 10.1016/j.jpeds.2013.10.029
Volkmann ER, Tashkin DP, Li N, et al. Mycophenolate Mofetil Versus Placebo for Systemic Sclerosis–Related Interstitial Lung Disease: An Analysis of Scleroderma Lung Studies I and II. Arthritis Rheumatol. 2017;69:1451–60. doi: 10.1002/art.40114
Lee K-A, Kim BY, Choi SJ, et al. A Real-World Experience of Mycophenolate Mofetil for Systemic Sclerosis: A Retrospective Multicenter Observational Study. Arch Rheumatol. 2020;35:366–75. doi: 10.46497/ArchRheumatol.2020.7771
Ruaro B, Confalonieri M, Matucci-Cerinic M, et al. The Treatment of Lung Involvement in Systemic Sclerosis. Pharmaceuticals. 2021;14:154. doi: 10.3390/ph14020154
Weibel L. Diagnosis and management of morphoea in children: an overview. Clin Exp Dermatol. 2021;46:487–94. doi: 10.1111/ced.14562
Souza AWSD, Dantas JG, Montandon ACDOES, et al. Position statement of the Brazilian society of Rheumatology on mesna use as a preventive therapy for bladder disease in patients with systemic autoimmune diseases and systemic vasculitis under cyclophosphamide treatment. Adv Rheumatol. 2024;64:41. doi: 10.1186/s42358-024-00380-0
Adrovic A, Yildiz M, Haslak F, et al. Tocilizumab therapy in juvenile systemic sclerosis: a retrospective single centre pilot study. Rheumatol Int. 2021;41:121–8. doi: 10.1007/s00296-020-04732-z
Ogino MH, Tadi P. Cyclophosphamide. StatPearls. Treasure Island (FL): StatPearls Publishing 2024.
Sircar G, Goswami RP, Sircar D, et al. Intravenous cyclophosphamide vs rituximab for the treatment of early diffuse scleroderma lung disease: open label, randomized, controlled trial. Rheumatology. 2018;57:2106–13. doi: 10.1093/rheumatology/key213
Zulian F, Dal Pozzolo R, Meneghel A, et al. Rituximab for rapidly progressive juvenile systemic sclerosis. Rheumatology. 2020;59:3793–7. doi: 10.1093/rheumatology/keaa193
Jordan S, Distler JHW, Maurer B, et al. Effects and safety of rituximab in systemic sclerosis: an analysis from the European Scleroderma Trial and Research (EUSTAR) group. Ann Rheum Dis. 2015;74:1188–94. doi: 10.1136/annrheumdis-2013-204522
Sulieman SE, Metjian TA, Zaoutis TE, et al. Pneumocystis Pneumonia: Epidemiology and Options for Prophylaxis in Non-HIV Immunocompromised Pediatric Patients. Curr Fungal Infect Rep. 2014;8:45–55. doi: 10.1007/s12281-014-0177-y
Kalampokis I, Yi BY, Smidt AC. Abatacept in the treatment of localized scleroderma: A pediatric case series and systematic literature review. Semin Arthritis Rheum. 2020;50:645–56. doi: 10.1016/j.semarthrit.2020.03.020
Tang J, Zheng W, Yang B. P08 Successful treatment of paediatric morphoea with tofacitinib. Br J Dermatol. 2023;188:ljad113.036. doi: 10.1093/bjd/ljad113.036
Алексеева Е.И., Крехова Е.А., Криулин И.А., Криулина Т.Ю., Дворяковская Т.М., Исаева К.Б., Чистякова Е.Г., Чомахидзе А.М., Ломакина О.Л., Фетисова А.Н., Чибисова К.В., Цулукия И.Т., Шингарова М.Ш., Ботова М.С., Кондратьева Н.М., Кокина М.Ю., Румянцев М.А. Опыт применения ингибитора янус-киназ упадацитиниба у детей с ревматическими болезнями. Вопросы практической педиатрии. 2024; 19(2): 59–79. DOI: 10.20953/1817-7646-2024-2-59-79.
Walker KM, Pope J. Treatment of Systemic Sclerosis Complications: What to Use When First-Line Treatment Fails—A Consensus of Systemic Sclerosis Experts. Semin Arthritis Rheum. 2012;42:42–55. doi: 10.1016/j.semarthrit.2012.01.003
Shouval DS, Mukamel M, Zulian F, et al. Iloprost treatment for refractory Raynaud’s phenomenon in two infants. Clin Exp Rheumatol. 2008;26:S105-107.
Bartolone S, Trifiletti A, De Nuzzo G, et al. Efficacy evaluation of prostaglandin E1 against placebo in patients with progressive systemic sclerosis and significant Raynaud’s phenomenon. Minerva Cardioangiol. 1999;47:137–43.
Langevitz P, Buskila D, Lee P, et al. Treatment of refractory ischemic skin ulcers in patients with Raynaud’s phenomenon with PGE1 infusions. J Rheumatol. 1989;16:1433–5.
Juche A, Siegert E, Mueller-Ladner U, et al. Versorgungsrealität der stationären vasoaktiven Therapie mit Prostazyklinderivaten bei Patienten mit akralen Durchblutungsstörungen bei systemischer Sklerose in Deutschland. Z Für Rheumatol. 2020;79:1057–66. doi: 10.1007/s00393-019-00743-9
Гусева Н. Вазапростан в комплексном лечении системной склеродермии и синдрома Рейно / Н. Гусева // Врач. – 2006. – № 5. – С. 46-50.
Linnemann B, Erbe M. Raynaud’s phenomenon and digital ischaemia - pharmacologic approach and alternative treatment options. Vasa. 2016;45:201–12. doi: 10.1024/0301-1526/a000526
Distler JHW. Primäres und sekundäres Raynaud-Phänomen. Z Für Rheumatol. 2008;67:211–9. doi: 10.1007/s00393-008-0282-9
Adrovic A. Juvenile Scleroderma: A Referral Center Experience. Arch Rheumatol. 2018;33:344–51. doi: 10.5606/ArchRheumatol.2018.6578
Milan MJDC, Dans LF, Torres-Ticzon VMF. Acute limb ischemia in an adolescent with COVID-19 and systemic scleroderma: a case report. BMC Pediatr. 2022;22:737. doi: 10.1186/s12887-022-03761-w
Davuluri S, Lood C, Chung L. Calcinosis in systemic sclerosis. Curr Opin Rheumatol. 2022;34:319–27. doi: 10.1097/BOR.0000000000000896
Aleksandrov AA, Kisliak OA, Leontyeva IV. Clinical guidelines on arterial hypertension diagnosis, treatment and prevention in children and adolescents. Syst Hypertens. 2020;17:7–35. doi: 10.26442/2075082X.2020.2.200126
Garcia De La Pena-Lefebvre P, Rodriguez Rubio S, Valero Exposito M, et al. Long-term experience of bosentan for treating ulcers and healed ulcers in systemic sclerosis patients. Rheumatology. 2007;47:464–6. doi: 10.1093/rheumatology/ken001
Paul F, Cartron G. Infusion-related reactions to rituximab: frequency, mechanisms and predictors. Expert Rev Clin Immunol. 2019;15:383–9. doi: 10.1080/1744666X.2019.1562905
Кокина М.Ю., Фомина Д.С., Лебедкина М.C., Мутовина З.Ю., Жолобова Е.С., Курбанова С.Х., Наргизян А.К., Фетисова А.Н., Анджель А.Е., Дворяковская Т.М., Шилькрот И.Ю., Алексеева Е.И. Эффективность и безопасность применения двухкомпонентного препарата моноклональных антител к SARS-CoV-2 (тиксагевимаб + цилгавимаб) для доконтактной профилактики новой коронавирусной инфекции у иммунокомпрометированных пациентов детского возраста с ревматическими заболеваниями. Предварительные результаты первого в Российской Федерации проспективного наблюдательного когортного исследования. Вопросы практической педиатрии. 2023; 18(1): 16–26
Hsieh L-F, Mao H-F, Lu C-C, et al. Rheumatologic Rehabilitation. Braddom’s Physical Medicine and Rehabilitation. Elsevier 2021:606-626.e1.
Stucki G, Kroeling P. Physical therapy and rehabilitation in the management of rheumatic disorders. Best Pract Res Clin Rheumatol. 2000;14:751–71. doi: 10.1053/berh.2000.0111
Luttosch F, Baerwald C. Rehabilitation in der Rheumatologie. Internist. 2010;51:1239–45. doi: 10.1007/s00108-010-2626-1
Heijstek MW, Ott de Bruin LM, Bijl M, et al. EULAR recommendations for vaccination in paediatric patients with rheumatic diseases. Ann Rheum Dis. 2011;70:1704–12. doi: 10.1136/ard.2011.150193
Алексеева Е., Валиева С., Бзарова Т., Семикина Е., Исаева К., Лисицин А., Денисова Р., Чистякова Е., Слепцова Т., Митенко Е. Эффективность и безопасность отечественного рекомбинантного человеческого гранулоцитарного колониестимулирующего фактора при нейтропениях, развивающихся на фоне анти-в клеточной и иммуносупрессивной терапии у больных ювенильным ревматоидным артритом. Вопросы современной педиатрии. 2010;9(4):94-100.
Yilmaz D., Ritchey A. K. Severe neutropenia in children: a single institutional experience //Journal of Pediatric Hematology/Oncology. – 2007. – Т. 29. – №. 8. – С. 513-518.
Segel, G. B., & Halterman, J. S. (2008). Neutropenia in pediatric practice. Pediatrics in review, 29(1), 12.
Novelli, V., & Holzel, H. (1999). Safety and tolerability of fluconazole in children. Antimicrobial agents and chemotherapy, 43(8), 1955-1960.
Garcia-Lloret M, McGhee S, Chatila TA. Immunoglobulin Replacement Therapy in Children. Immunol Allergy Clin North Am. 2008;28:833–49. doi: 10.1016/j.iac.2008.07.001
Rodriguez MM, Wagner-Weiner L. Intravenous Immunoglobulin in Pediatric Rheumatology: When to Use It and What Is the Evidence. Pediatr Ann. 2017;46. doi: 10.3928/19382359-20161214-01
Scientific Centre of Children’s Health, Moscow, Russian Federation, Alexeeva EI, Denisova RV, et al. Intravenous Immunoglobulin in Pediatric Rheumatology Practice. Curr Pediatr Vopr Sovrem Pediatr. 2015;14:219–23. doi: 10.15690/vsp.v14i2.1290
Mulhearn B, Bruce IN. Indications for IVIG in rheumatic diseases. Rheumatology. 2015;54:383–91. doi: 10.1093/rheumatology/keu429
Prasad AN, Chaudhary S. Intravenous immunoglobulin in pediatrics: A review. Med J Armed Forces India. 2014;70:277–80. doi: 10.1016/j.mjafi.2013.05.011
Petty RE, Laxer RM, Lindsley CB, et al. Textbook of pediatric rheumatology. 8th ed. Philadelphia: Elsevier, Inc 2020.
Ospina FE, Echeverri A, Zambrano D, et al. Distinguishing infections vs flares in patients with systemic lupus erythematosus: Table 1. Rheumatology. 2016;kew340. doi: 10.1093/rheumatology/kew340
Demirkol D, Yildizdas D, Bayrakci B, et al. Hyperferritinemia in the critically ill child with secondary hemophagocytic lymphohistiocytosis/sepsis/multiple organ dysfunction syndrome/macrophage activation syndrome: what is the treatment? Crit Care. 2012;16:R52. doi: 10.1186/cc11256
El-Nawawy A, El-Kinany H, Hamdy El-Sayed M, et al. Intravenous Polyclonal Immunoglobulin Administration to Sepsis Syndrome Patients: A Prospective Study in a Pediatric Intensive Care Unit. J Trop Pediatr. 2005;51:271–8. doi: 10.1093/tropej/fmi011
Kaegi C, Wuest B, Schreiner J, et al. Systematic Review of Safety and Efficacy of Rituximab in Treating Immune-Mediated Disorders. Front Immunol. 2019;10:1990. doi: 10.3389/fimmu.2019.01990
Alexeeva EI, Valieva SI, Bzarova TM, et al. Efficacy and safety of repeat courses of rituximab treatment in patients with severe refractory juvenile idiopathic arthritis. Clin Rheumatol. 2011;30:1163–72. doi: 10.1007/s10067-011-1720-7
Rao S, Abzug MJ, Carosone-Link P, et al. Intravenous Acyclovir and Renal Dysfunction in Children: A Matched Case Control Study. J Pediatr. 2015;166:1462-1468.e4. doi: 10.1016/j.jpeds.2015.01.023
Kimberlin DW. Acyclovir Dosing in the Neonatal Period and Beyond. J Pediatr Infect Dis Soc. 2013;2:179–82. doi: 10.1093/jpids/pis138
Whitley RJ. Herpes simplex virus in children. Curr Treat Options Neurol. 2002;4:231–7. doi: 10.1007/s11940-002-0040-2
Antiviral Drugs in Children and Adolescents. Pediatr Infect Dis. 2020;1:123–8. doi: 10.5005/jp-journals-10081-1221
Zhang S, Zhu Y, Jin Y, et al. Difference between Acyclovir and Ganciclovir in the Treatment of Children with Epstein–Barr Virus-Associated Infectious Mononucleosis. Evid Based Complement Alternat Med. 2021;2021:1–6. doi: 10.1155/2021/8996934
Chellapandian D, Das R, Zelley K, et al. Treatment of Epstein Barr virus-induced haemophagocytic lymphohistiocytosis with rituximab-containing chemo-immunotherapeutic regimens. Br J Haematol. 2013;162:376–82. doi: 10.1111/bjh.12386
Selmi C, Gershwin ME. Diagnosis and classification of reactive arthritis. Autoimmun Rev. 2014;13:546–9. doi: 10.1016/j.autrev.2014.01.005
Jones NL, Koletzko S, Goodman K, et al. Joint ESPGHAN/NASPGHAN Guidelines for the Management of Helicobacter pylori in Children and Adolescents (Update 2016). J Pediatr Gastroenterol Nutr. 2017;64:991–1003. doi: 10.1097/MPG.0000000000001594
Kotilea K, Cadranel S, Salame A, et al. Efficacy and safety of bismuth‐based quadruple therapy for Helicobacter pylori eradication in children. Helicobacter. 2021;26:e12825. doi: 10.1111/hel.12825
Бельмер С.В., Корниенко Е.А., Волынец Г.В., Гурова М.М., Звягин А.А., Камалова А.А., Луппова Н.Е., Нижевич А.А., Новикова В.П., Печкуров Д.В., Приворотский В.Ф., Сатаев В.У., Тяжева А.А., Файзуллина Р.А., Хавкин А.И. Диагностика и лечение хеликобактерной инфекции у детей. Экспериментальная и клиническая гастроэнтерология. 2021;(9):119-127. https://doi.org/10.31146/1682-8658-ecg-193-9-119-127.
Рубрикатор клинических рекомендаций. Язвенная болезнь желудка и/или двенадцатиперстной кишки. URL: https://cr.minzdrav.gov.ru/view-cr/388_3.
What’s New Adult and Adolescent Opportunistic Infection. AIDSinfo. https://aidsinfo.nih.gov/guidelines/html/4/adult-and-adolescent-opportunistic-infection/392/whats-new (accessed 14 Apr 2020).
Pneumonia in Immunocompromised Patients: Overview, Causes of Pneumonia, HIV/AIDS. Published Online First: 26 June 2021.https://emedicine.medscape.com/article/807846-overview#a11.. (accessed 10 Aug 2021).
Douglas AP, Smibert OliviaC, Bajel A, et al. Consensus guidelines for the diagnosis and management of invasive aspergillosis, 2021. Intern Med J. 2021;51:143–76. doi: 10.1111/imj.15591
What’s New Adult and Adolescent Opportunistic Infection. AIDSinfo. https://aidsinfo.nih.gov/guidelines/html/4/adult-and-adolescent-opportunistic-infection/392/whats-new (accessed 14 Apr 2020).
Kutilek S, Plasilova I, Langer J. Ibandronate in the treatment of pediatric osteoporosis. Bone Abstr. Published Online First: 9 June 2015. doi: 10.1530/boneabs.4.P80
Лисицин А., Алексеева Е., Пинелис В., Баканов М., Валиева С., Бзарова Т. Опыт применения ибандроновой кислоты у больных с тяжелым течением ревматических болезней и системным остеопорозом. Вопросы современной педиатрии. 2010;9(1):116-121.
Bachrach LK, Ward LM. Clinical Review: Bisphosphonate Use in Childhood Osteoporosis. J Clin Endocrinol Metab. 2009;94:400–9. doi: 10.1210/jc.2008-1531
Денисова Р., Алексеева Е., Пинелис В., Баканов М., Валиева С., Бзарова Т., Исаева К., Морев С., Кузнецова Г. Эффективность и безопасность ибандроновой кислоты для внутривенного введения при тяжелом системном остеопорозе у больных ювенильным артритом. Вопросы современной педиатрии. 2011;10(6):83–88.
Trapani S, Grisolia F, Simonini G, et al. Incidence of occult cancer in children presenting with musculoskeletal symptoms: a 10-year survey in a pediatric rheumatology unit. Semin Arthritis Rheum. 2000;29:348–59. doi: 10.1053/sarh.2000.5752
Hernandez J, Polo R, Alvarez J, et al. [A “lupus-like” syndrome as the form of presentation of pulmonary adenocarcinoma]. An Med Interna Madr Spain 1984. 2000;17:558–9.
Calixto O-J, Franco J-S, Anaya J-M. Lupus mimickers. Autoimmun Rev. 2014;13:865–72. doi: 10.1016/j.autrev.2014.05.002
Ladouceur A, Tessier-Cloutier B, Clarke AE, et al. Cancer and Systemic Lupus Erythematosus. Rheum Dis Clin N Am. 2020;46:533–50. doi: 10.1016/j.rdc.2020.05.005
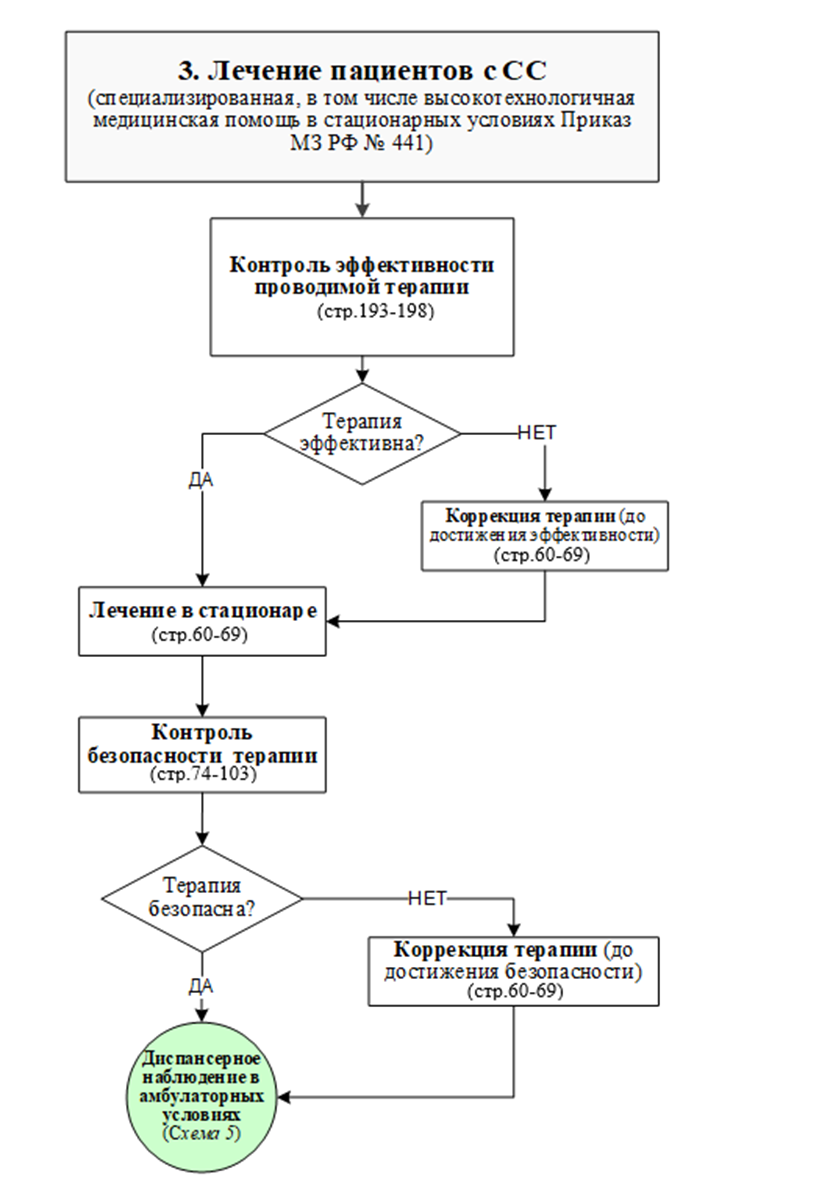
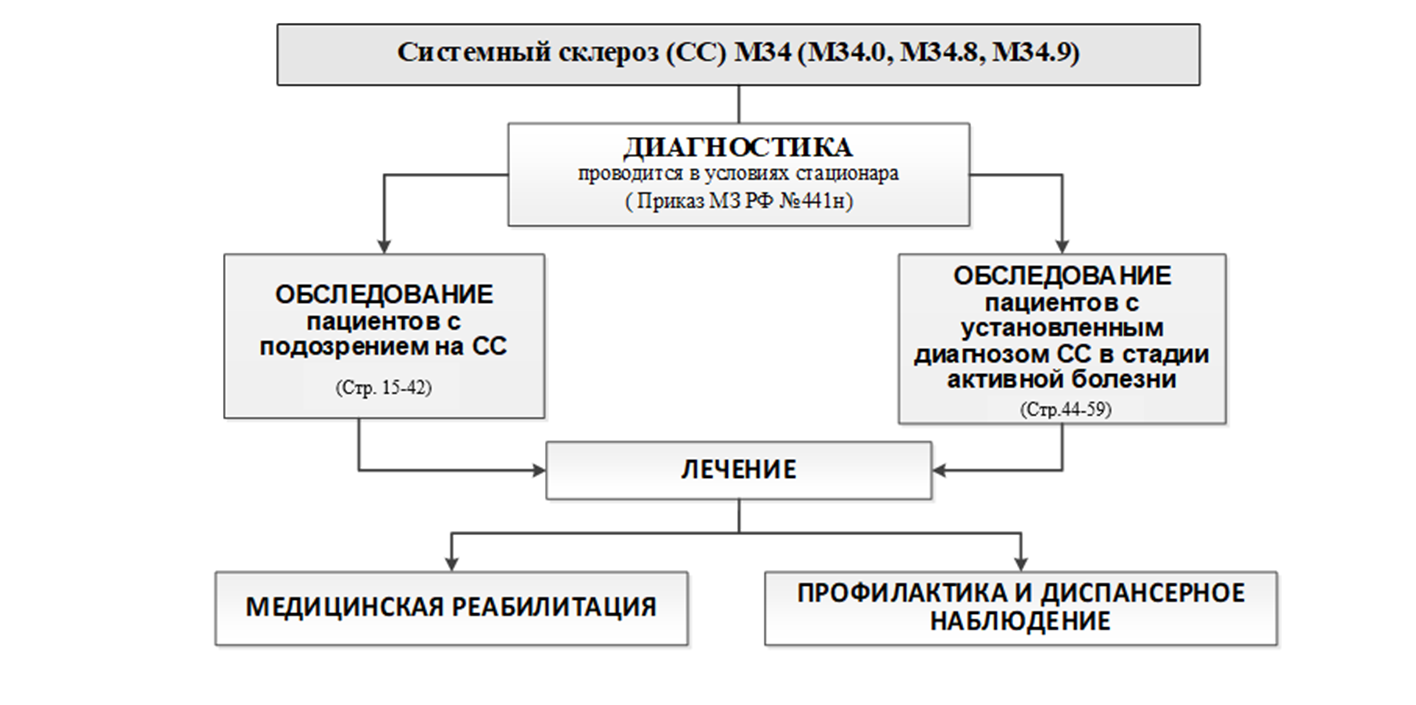 Схема 2
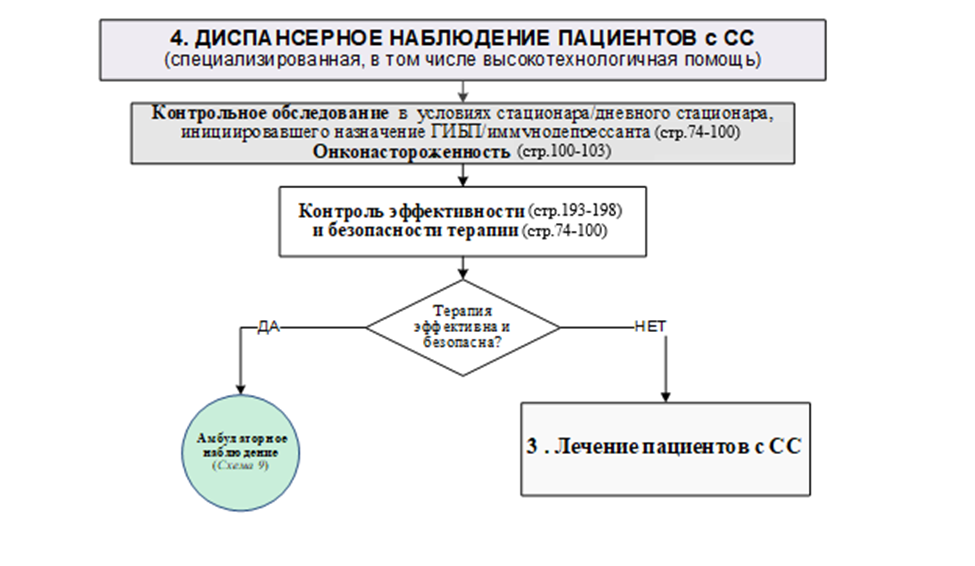
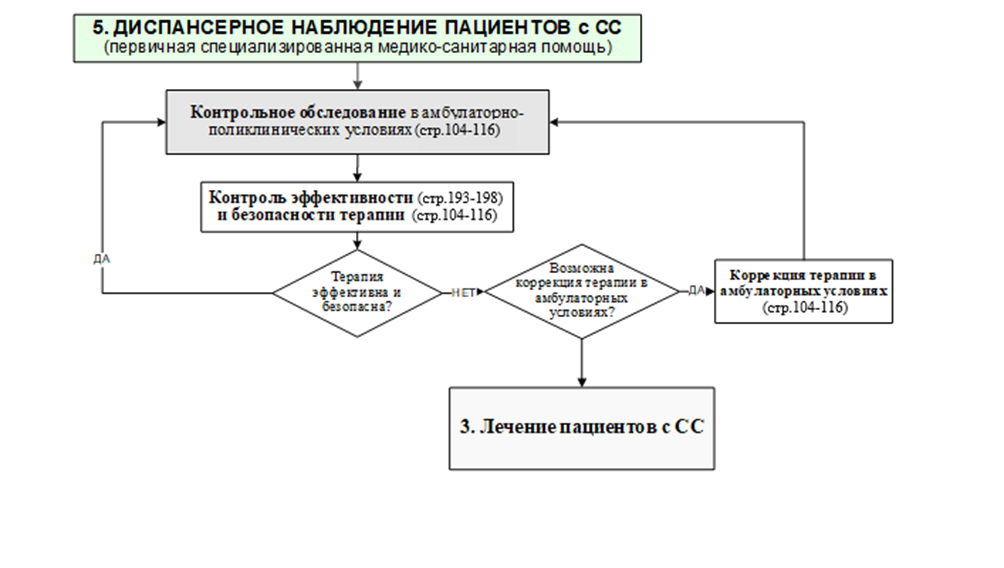
Схема 2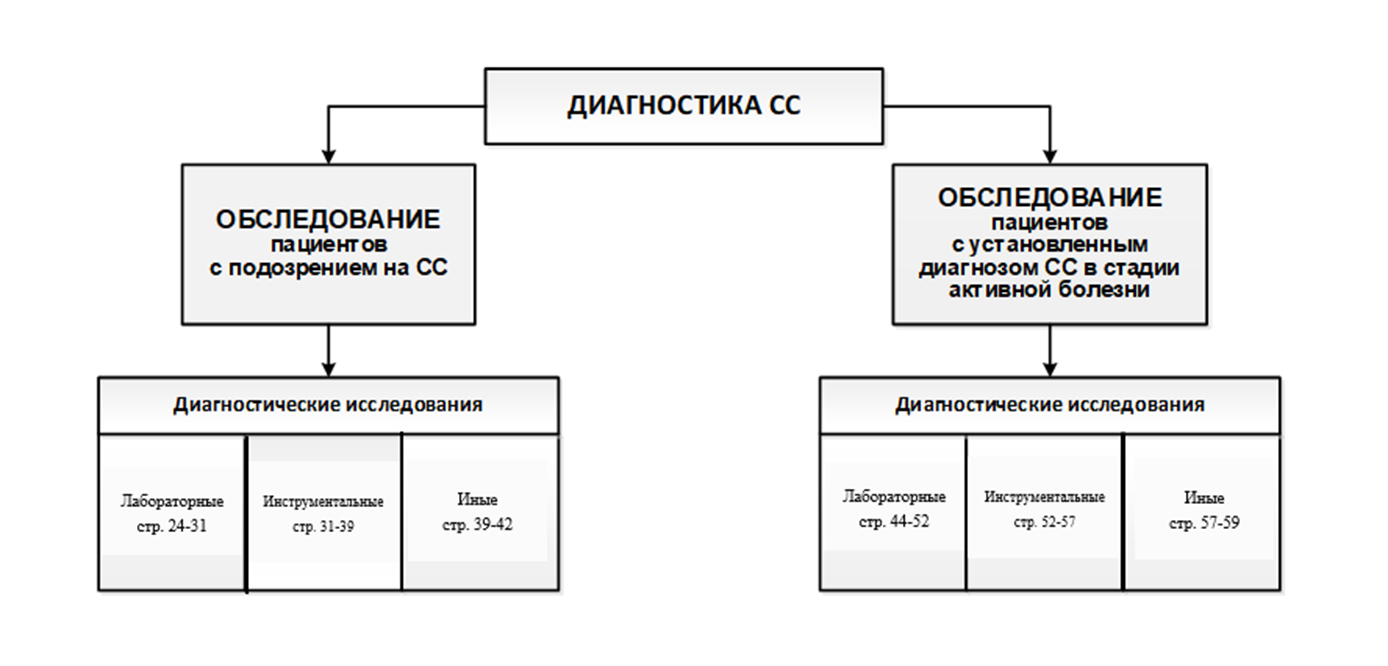 Схема 3
Схема 3