National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 2002;39(2 Suppl 1):S1-266.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int Suppl 2013;3:1-150.
Клинические рекомендации "Хроническая болезнь почек (ХБП)" (одобрены Минздравом России) 2024.
Kramer A., Boenink R., Stel V.S. et al. The ERA-EDTA Registry Annual Report 2018: a summary // Clinical Kidney Journal. https://doi.org/10.1093/ckj/sfaa271
Tsai WC, Wu HY, Peng YS et al. Risk Factors for Development and Progression of Chronic Kidney Disease: A Systematic Review and Exploratory Meta-Analysis. Medicine (Baltimore) 2016;95(11):e3013. doi: 10.1097/MD.0000000000003013
Shen Y, Cai R, Sun J et al. Diabetes mellitus as a risk factor for incident chronic kidney disease and end-stage renal disease in women compared with men: a systematic review and meta-analysis. Endocrine 2017;55(1):66-76. doi: 10.1007/s12020-016-1014-6
Chang AR, Grams ME, Ballew SH et al. Adiposity and risk of decline in glomerular filtration rate: meta-analysis of individual participant data in a global consortium. BMJ 2019;364: k5301. doi: 10.1136/bmj.k5301
Nitsch D, Grams M, Sang Y et al. Associations of estimated glomerular filtration rate and albuminuria with mortality and renal failure by sex: a meta-analysis. BMJ 2013;346: f324. doi: 10.1136/bmj. f324
See EJ, Jayasinghe K, Glassford N et al. Long-term risk of adverse outcomes after acute kidney injury: a systematic review and meta-analysis of cohort studies using consensus definitions of exposure. Kidney Int 2019;95(1):160-172. doi: 10.1016/j.kint.2018.08.036
Rashidbeygi E, Safabakhsh M, Delshad Aghdam S et al. Metabolic syndrome and its components are related to a higher risk for albuminuria and proteinuria: Evidence from a meta-analysis on 10,603,067 subjects from 57 studies. Diabetes Metab Syndr 2019;13(1):830-843. doi: 10.1016/j.dsx.2018.12.006
Xia J, Wang L, Ma Z et al. Cigarette smoking and chronic kidney disease in the general population: a systematic review and meta-analysis of prospective cohort studies. Nephrol Dial Transplant 2017;32(3):475-487. doi: 10.1093/ndt/gfw452
Garofalo C, Borrelli S, Pacilio M et al. Hypertension and Prehypertension and Prediction of Development of Decreased Estimated GFR in the General Population: A Meta-analysis of Cohort Studies. Am J Kidney Dis 2016;67(1):89-97. doi: 10.1053/j.ajkd.2015.08.027
Shang W, Li L, Ren Y et al. History of kidney stones and risk of chronic kidney disease: a meta-analysis. PeerJ 2017;5:e2907. doi: 10.7717/peerj.2907
Musso G, Gambino R, Tabibian JH et al. Association of non-alcoholic fatty liver disease with chronic kidney disease: a systematic review and meta-analysis. PLoS Med 2014;11(7):e1001680. doi: 10.1371/journal.pmed.1001680
Mantovani A, Zaza G, Byrne CD et al. Nonalcoholic fatty liver disease increases risk of incident chronic kidney disease: A systematic review and meta-analysis. Metabolism 2018; 79: 64-76. doi: 10.1016/j.metabol.2017.11.003
Yu X, Yuan Z, Lu H et al. Relationship between birth weight and chronic kidney disease: evidence from systematics review and two-sample Mendelian randomization analysis. Hum Mol Genet 2020;29(13):2261-2274. doi: 10.1093/hmg/ddaa074
Nankivell BJ, Alexander SI. Rejection of the kidney allograft. N Engl J Med. 2010 Oct 07;363(15):1451-62]:
Joosten SA, Sijpkens YW, van Kooten C, Paul LC. Chronic renal allograft rejection: pathophysiologic considerations. Kidney Int. 2005 Jul;68(1):1-13.]
Fresenius medical care annual report 2018. https://www.freseniusmedicalcare.com/fileadmin/data/com/pdf/Media_Center/Publications/Annual_Reports/FME_Annual-Report_2018.pdf
http://www.transplant-observatory.org/summary/
Заместительная почечная терапия хронической болезни почек 5 стадии в Российской Федерации 2016-2020 гг. Краткий отчет по данным Общероссийского Регистра заместительной почечной терапии Российского диализного общества / А. М. Андрусев, Н. Г. Перегудова, М. Б. Шинкарев, Н. А. Томилина // Нефрология и диализ. – 2022. – Т. 24, № 4. – С. 555-565. – DOI 10.28996/2618-9801-2022-4-555-565. – EDN RBZZBH.
Готье С.В., Хомяков С.М. Донорство и трансплантация органов в Российской Федерации в 2023 году. XVI сообщение регистра Российского трансплантологического общества. Вестник трансплантологии и искусственных органов. 2024;26(3):8-31. https://doi.org/10.15825/1995-1191-2024-3-8-31
National Center for Health Statistics. WHO Collaborating Centre for the WHO Family of International Classifications. https://www.who.int/classifications/icd/ICD-10%20Updates%202007.pdf
https://banfffoundation.org/central-repository-for-banff-2019-resources-3
Schinstock CA, Mannon RB, Budde K, Chong AS, Haas M, Knechtle S, Lefaucheur C, Montgomery RA, Nickerson P, Tullius SG, Ahn C, Askar M, Crespo M, Chadban SJ, Feng S, Jordan SC, Man K, Mengel M, Morris RE, O'Doherty I, Ozdemir BH, Seron D, Tambur AR, Tanabe K, Taupin JL, O'Connell PJ. Recommended Treatment for Antibody-mediated Rejection After Kidney Transplantation: The 2019 Expert Consensus From the Transplantion Society Working Group. Transplantation. 2020 May;104(5):911-922. doi: 10.1097/TP.0000000000003095
Tan EK, Bentall A, Dean PG, et al. Use of eculizumab for active antibody-mediated rejection that occurs early post-kidney transplantation: a consecutive series of 15 cases. Transplantation. 2019;103:2397–2404.
Orandi BJ, Zachary AA, Dagher NN, et al. Eculizumab and splenectomy as salvage therapy for severe antibody-mediated rejection after HLA-incompatible kidney transplantation. Transplantation. 2014;98:857–863.
Loupy A, Vernerey D, Tinel C, et al. Subclinical rejection phenotypes at 1 year post-transplant and outcome of kidney allografts. J Am Soc Nephrol. 2015;26:1721–1731.
Stegall MD, Diwan T, Raghavaiah S, et al. Terminal complement inhibition decreases antibody-mediated rejection in sensitized renal transplant recipients. Am J Transplant. 2011;11:2405–2413.
Wavamunno MD, O’Connell PJ, Vitalone M, et al. Transplant glomerulopathy:ultrastructural abnormalities occur early in longitudinal analysis of protocol biopsies. Am J Transplant. 2007;7:2757–2768.
Bentall A, Cornell LD, Gloor JM, et al. Five-year outcomes in living donor kidney transplants with a positive crossmatch. Am J Transplant. 2013;13:76–85.].
Aubert O, Loupy A, Hidalgo L, et al. Antibody-mediated rejection due to preexisting versus de novo donor-specific antibodies in kidney allograft recipients. J Am Soc Nephrol. 2017;28:1912–1923.]
KDIGO Clinical Practice Guideline on the Evaluation and Management of Candidates for Kidney Transplantation. Transplantation, 2020. 104, 4S: 1-103.
Tonelli M, Wiebe N, Knoll G, et al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant. 2011; 11: 2093–2109
Dudley C, Harden P. Renal Association Clinical Practice Guideline on the assessment of the potential kidney transplant recipient. Nephron Clin Pract. 2011; 118 Suppl 1: c209–224.
Thomsen T, Villebro N, Moller AM. Interventions for preoperative smoking cessation. Cochrane Database Syst Rev. 2014: CD002294.
Duerinckx N, Burkhalter H, Engberg SJ, et al. Correlates and Outcomes of Posttransplant Smoking in Solid Organ Transplant Recipients: A Systematic Literature Review and Meta-Analysis. Transplantation. 2016; 100: 2252–2263.
Nourbala MH, Nemati E, Rostami Z, et al. Impact of cigarette smoking on kidney transplant recipients: a systematic review. Iran J Kidney Dis. 2011; 5: 141–148.
Corbett C, Armstrong MJ, Neuberger J. Tobacco smoking and solid organ transplantation. Transplantation. 2012; 94: 979–987.
Schold JD, Srinivas TR, Guerra G, et al. A “weight-listing” paradox for candidates of renal transplantation? Am J Transplant. 2007; 7: 550–559.
Molnar MZ, Streja E, Kovesdy CP, et al. Associations of body mass index and weight loss with mortality in transplant-waitlisted maintenance hemodialysis patients. Am J Transplant. 2011; 11: 725–736.
Gill JS, Lan J, Dong J, et al. The survival benefit of kidney transplantation in obese patients. Am J Transplant. 2013; 13: 2083–2090.
Kostakis ID, Kassimatis T, Bianchi V, Paraskeva P, Flach C, Callaghan C, Phillips BL, Karydis N, Kessaris N, Calder F, Loukopoulos I. UK renal transplant outcomes in low and high BMI recipients: the need for a national policy. J Nephrol. 2020 Apr;33(2):371-381. doi: 10.1007/s40620-019-00654-7. Epub 2019 Oct 3. PMID: 31583535.
Gillespie H, O'Neill S, Curtis RMK, Callaghan C, Courtney AE. When There is No Guidance From the Guidelines: Renal Transplantation in Recipients With Class III Obesity. Transpl Int. 2023 Sep 15;36:11428. doi: 10.3389/ti.2023.11428. PMID: 37779511; PMCID: PMC10540226.
Scheuermann U, Babel J, Pietsch UC, Weimann A, Lyros O, Semmling K, Hau HM, Seehofer D, Rademacher S, Sucher R. Recipient obesity as a risk factor in kidney transplantation. BMC Nephrol. 2022 Jan 18;23(1):37. doi: 10.1186/s12882-022-02668-z. PMID: 35042452; PMCID: PMC8767742.
Oberholzer J, Giulianotti P, Danielson KK, et al. Minimally invasive robotickidney transplantation for obese patients previously denied access to transplantation. Am J.Transplant. 2013; 13: 721–728
Zimmerman D, Sood MM, Rigatto C, et al. Systematic review and meta-analysis of incidence, prevalence and outcomes of atrial fibrillation in patients on dialysis. Nephrol Dial Transplant. 2012; 27: 3816–3822.
Garg L, Chen C, Haines DE. Atrial fibrillation and chronic kidney disease requiring hemodialysis - Does warfarin therapy improve the risks of this lethal combination? Int J Cardiol. 2016; 222: 47–50.
Douketis, J.D., et al. Perioperative Management of Antithrombotic Therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest, 2012. 141. https://pubmed.ncbi.nlm.nih.gov/22315266
Pawlicki, J., et al. Risk factors for early hemorrhagic and thrombotic complications after kidney transplantation. Transplant Proc, 2011. 43: 3013. https://pubmed.ncbi.nlm.nih.gov/
Rouviere, O., et al. Acute thrombosis of renal transplant artery: graft salvage by means of intraarterial fibrinolysis. Transplantation, 2002. 73: 403.
Campbell S, Pilmore H, Gracey D, et al. KHA-CARI guideline: recipient assessment for transplantation. Nephrology (Carlton). 2013; 18: 455–462.
Kasiske BL, Cangro CB, Hariharan S, et al. The evaluation of renal transplantation candidates: clinical practice guidelines. Am J Transplant. 2001; 1 Suppl 2: 3–95
European Renal Best Practice Transplantation Guideline Development G. ERBP Guideline on the Management and Evaluation of the Kidney Donor and Recipient. Nephrol Dial Transplant. 2013; 28 Suppl 2: ii1–71.
Olbrisch ME, Benedict SM, Ashe K, et al. Psychological assessment and care of organ transplant patients. J Consult Clin Psychol. 2002; 70: 771–783.
Dew MA, Switzer GE, DiMartini AF, et al. Psychosocial assessments and outcomes in organ transplantation. Prog Transplant. 2000; 10: 239–259.
Broggi E, Bruyere F, Gaudez F, et al. Risk factors of severe incisional hernia after renal transplantation: a retrospective multicentric casecontrol study on 225 patients. World J Urol. 2017; 35: 1111–1117.
Ooms LS, Verhelst J, Jeekel J, et al. Incidence, risk factors, and treatment of incisional hernia after kidney transplantation: An analysis of 1,564 consecutive patients. Surgery. 2016; 159: 1407–1411
Smith CT, Katz MG, Foley D, et al. Incidence and risk factors of incisional hernia formation following abdominal organ transplantation. Surg Endosc. 2015; 29: 398–404.
NIH National Institute of Diabetes and Digestive and Kidney Diseases.Overweight & Obesity Statistics. (2017). https://www.niddk.nih.gov/health-information/health-statistics/Pages/overweight-obesity-statistics.aspx (Accessed February 28, 2020).
Nylund KM, Meurman JH, Heikkinen AM, et al. Oral health in patients with renal disease: a longitudinal study from predialysis to kidney transplantation. Clin Oral Investig. 2018; 22: 339–347.
Nylund K, Meurman JH, Heikkinen AM, et al. Oral health in predialysis patients with emphasis on periodontal disease. Quintessence Int. 2015; 46: 899–907.
Veisa G, Tasmoc A, Nistor I, et al. The impact of periodontal disease on physical and psychological domains in long-term hemodialysis patients: a cross-sectional study. Int Urol Nephrol. 2017; 49: 1261–1266.
Grossman DC, Curry SJ, Owens DK, et al. Screening for Prostate Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2018; 319: 1901–1913.
Wong G, Howard K, Webster AC, et al. Screening for renal cancer in recipients of kidney transplants. Nephrol Dial Transplant. 2011; 26: 1729–1739.
Данович ГМ. Трансплантация почки. М: ГЭОТАР-Медиа; 2013: 848.
Smith RA, Andrews KS, Brooks D, et al. Cancer screening in the United States, 2019: A review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin. 2019; 69: 184–210.
Siu AL. Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2016; 164:279–296.
Sanders RD, Bottle A, Jameson SS, et al. Independent preoperative predictors of outcomes in orthopedic and vascular surgery: the influence of time interval between an acute coronary syndrome or stroke and the operation. Ann Surg. 2012; 255: 901–907.
Jorgensen ME, Torp-Pedersen C, Gislason GH, et al. Time elapsed after ischemic stroke and risk of adverse cardiovascular events and mortality following elective noncardiac surgery. JAMA. 2014; 312: 269–277.
LeFevre ML, Force USPST. Screening for asymptomatic carotid artery stenosis: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014; 161: 356–362.
Rossitter CW, Vigo RB, Gaber AO, et al. Evaluation of Carotid Ultrasonography Screening Among Kidney Transplant Candidates: A Single-Center, Retrospective Study. Transplant Direct. 2017; 3: e135.
Chadban SJ, Staplin ND. Is it time to increase access to transplantation for those with diabetic end-stage kidney disease? Kidney Int. 2014; 86: 464–466.
Keddis MT, El Ters M, Rodrigo E, et al. Enhanced posttransplant management of patients with diabetes improves patient outcomes. Kidney Int. 2014; 86: 610–618.
Boucek P, Saudek F, Pokorna E, et al. Kidney transplantation in type 2 diabetic patients: a comparison with matched non-diabetic subjects. Nephrol Dial Transplant. 2002; 17: 1678–1683.
Yates CJ, Fourlanos S, Hjelmesaeth J, et al. New-onset diabetes after kidney transplantation-changes and challenges. Am J Transplant. 2012; 12: 820–828.
Argente-Pla M, Pérez-Lázaro A, Martinez-Millana A, et al. Simultaneous Pancreas Kidney Transplantation Improves Cardiovascular Autonomic Neuropathy with Improved Valsalva Ratio as the Most Precocious Test. J Diabetes Res. 2020; 7574628. doi: 10.1155/2020/7574628.
St Michel D, Donnelly T, Jackson T, et al. Assessing Pancreas Transplant Candidate Cardiac Disease: Preoperative Protocol Development at a Rapidly Growing Transplant Program. Methods Protoc. 2019; 2(4): 82. doi: 10.3390/mps2040082.
Chadban SJ, Staplin ND. Is it time to increase access to transplantation for those with diabetic end-stage kidney disease? Kidney Int. 2014; 86: 464–466.
Мартынов СА, Северина АС, Ларина ИИ, и др. Подготовка пациента с сахарным диабетом 1 типа на заместительной почечной терапии диализом к трансплантации почки. Проблемы Эндокринологии. 2020; 66(6): 18-30. https://doi.org/10.14341/probl12686.
Tydén G, Kumlien G, Berg UB. ABO-incompatible kidney transplantation in children. Pediatr Transplant. 2011; 15(5): 502-4.
Hourmant M, Figueres L, Gicquel A, et al. New rules of ABO-compatibility in kidney transplantation. Transfus Clin Biol. 2019; 26(3): 180-183.
Gloor JM, Lager DJ, Moore SB, et al. ABO-incompatible kidney transplantation using both A2 and non-A2 living donors. Transplantation. 2003;75:971–977.
Bohmig, G.A., et al. Strategies to overcome the ABO barrier in kidney transplantation. Nat Rev Nephrol, 2015. 11: 732.
De Clippel D, Baeten M, Torfs A, et al. Screening for HLA antibodies in plateletpheresis donors with a history of transfusion or pregnancy. Transfusion. 2014; 54: 3036–3042.
Shi X, Lv J, Han W, Zhong X, Xie X, Su B, Ding J. What is the impact of human leukocyte antigen mismatching on graft survival and mortality in renal transplantation? A meta-analysis of 23 cohort studies involving 486,608 recipients. BMC Nephrol. 2018 May 18;19(1):116. doi: 10.1186/s12882-018-0908-3. PMID: 29776389; PMCID: PMC5960106.
Filippone EJ, Farber JL. Humoral immune response and allograft function in kidney transplantation. Am J Kidney Dis. 2015;66:337–347.
Tait BD, Süsal C, Gebel HM, et al. Consensus guidelines on the testing and clinical management issues associated with HLA and non-HLA antibodies in transplantation. Transplantation. 2013;95:19–47.
Shi X, Liu R, Xie X, Lv J, Han W, Zhong X, Ding J. Effect of human leukocyte antigen mismatching on the outcomes of pediatric kidney transplantation: a systematic review and meta-analysis. Nephrol Dial Transplant. 2017 Nov 1;32(11):1939-1948. doi: 10.1093/ndt/gfx259.
Shiferaw WS, Akalu TY, Aynalem YA. Risk Factors for Anemia in Patients with Chronic Renal Failure: A Systematic Review and Meta-Analysis. Ethiop J Health Sci. 2020 Sep;30(5):829-842. doi: 10.4314/ejhs.v30i5.23. PMID: 33911845; PMCID: PMC8047269.
Fowler AJ, Ahmad T, Phull MK, Allard S, Gillies MA, Pearse RM. Meta-analysis of the association between preoperative anaemia and mortality after surgery. Br J Surg. 2015 Oct;102(11):1314-24. doi: 10.1002/bjs.9861. PMID: 26349842.
Allen UD, Preiksaitis JK, AST Infectious Diseases Community of Practice. Epstein-Barr virus and posttransplant lymphoproliferative disorder in solid organ transplantation. Am J Transplant. 2013; 13 Suppl 4: 107–120.
Malinis M, Boucher HW. Screening of donor and candidate prior to solid organ transplantation-Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019. 33(9):e13548. doi: 10.1111/ctr.13548.
Levitsky J, Doucette K, AST Infectious Diseases Community of Practice. Viral hepatitis in solid organ transplantation. Am J Transplant. 2013; 13 Suppl 4: 147–168.
Burdick RA, Bragg-Gresham JL, Woods JD, et al. Patterns of hepatitis B prevalence and seroconversion in hemodialysis units from three continents: the DOPPS. Kidney Int. 2003; 63: 2222–2229.
Kidney Disease: Improving Global Outcomes (KDIGO) Hepatitis C Work Group. KDIGO 2018 Clinical Practice Guideline on the Prevention, Diagnosis, Evaluation, and Treatment of Hepatitis C in Chronic Kidney Disease. Kidney Int Suppl. 2018;8:91–165.
Kotton CN, Kumar D, Caliendo AM, et al. Updated international consensus guidelines on the management of cytomegalovirus in solid organ transplantation. Transplantation. 2013; 96: 333–360.
Hardinger KL, Brennan DC. Cytomegalovirus Treatment in Solid Organ Transplantation: An Update on Current Approaches. Ann Pharmacother. 2024 Nov;58(11):1122-1133. doi: 10.1177/10600280241237534. Epub 2024 Mar 19. PMID: 38501850.
Прокопенко Е.И. Цитомегаловирусная инфекция после трансплантации почки: реальные достижения и перспективы изучения патогенеза, профилактики и лечения. Вестник трансплантологии и искусственных органов. 2019;21(3):151-165. https://doi.org/10.15825/1995-1191-2019-3-151-165
Российские клинические рекомендации по диагностике, лечению и профилактике венозных тромбоэмболических осложнений (ВТЭО). Флебология, Т.9, выпуск 2, № 4, 2015.
Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012; 141 (2 Suppl): e326-50.
Chang CY, Chien YJ, Kao MC, Lin HY, Chen YL, Wu MY. Pre-operative proteinuria, postoperative acute kidney injury and mortality: A systematic review and meta-analysis. Eur J Anaesthesiol. 2021 Jul 1;38(7):702-714. doi: 10.1097/EJA.0000000000001542
Levey AS, Becker C, Inker LA. Glomerular filtration rate and albuminuria for detection and staging of acute and chronic kidney disease in adults: a systematic review. JAMA. 2015 Feb 24;313(8):837-46. doi: 10.1001/jama.2015.0602. PMID: 25710660; PMCID: PMC4410363.
Chen J, Mohler ER, 3rd, Garimella PS, et al. Ankle Brachial Index and Subsequent Cardiovascular Disease Risk in Patients With Chronic Kidney Disease. J Am Heart Assoc. 2016; 5: pii: e003339.
Wu SW, Lin CK, Hung TW, et al. Subclinical peripheral arterial disease in renal transplantation. Am J Med Sci. 2014; 347: 267–270.
Gill JS, Ma I, Landsberg D, et al. Cardiovascular events and investigation in patients who are awaiting cadaveric kidney transplantation. J Am Soc Nephrol. 2005; 16: 808–816.
Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014; 64: e77–137.
Lentine KL, Costa SP, Weir MR, et al. Cardiac disease evaluation and management among kidney and liver transplantation candidates: a scientific statement from the American Heart Association and the American College of Cardiology Foundation: endorsed by the American Society of Transplant Surgeons, American Society of Transplantation, and National Kidney Foundation. Circulation. 2012; 126: 617–663.
Segall L, Nistor I, Covic A. Heart failure in patients with chronic kidney disease: a systematic integrative review. Biomed Res Int. 2014;2014:937398. doi: 10.1155/2014/937398. Epub 2014 May 15. PMID: 24959595; PMCID: PMC4052068.
Sarkio S, Halme L, Kyllonen L, et al. Severe gastrointestinal complications after 1,515 adult kidney transplantations. Transpl Int. 2004; 17: 505–510.
Telkes G, Peter A, Tulassay Z, et al. High frequency of ulcers, not associated with Helicobacter pylori, in the stomach in the first year after kidney transplantation. Nephrol Dial Transplant. 2011; 26: 727–732.
Hajj P, Ferlicot S, Massoud W, et al. Prevalence of renal cell carcinoma in patients with autosomal dominant polycystic kidney disease and chronic renal failure. Urology, 2009, 74, 631-634.
Boissier R, Hevia V, Bruins H, et al. The risk of tumour recurrence of patients undergoing renal transplantation for end-stage renal disease after previous treatment for a urological cancer: a systematic review. Eur Urol, 2018, 73, 94-108.
Boissier R, Hevia V, Bruins H, et al. The risk of tumour recurrence of patients undergoing renal transplantation for end-stage renal disease after previous treatment for a urological cancer: a systematic review. Eur Urol, 2018, 73, 94-108.
https://uroweb.org/guidelines/renal-transplantation
Ильинский И.М., Розенталь Р.Л. Патология почечных аллотрансплантатов.- «Зинатне».- Рига.- 1990.- 175 с.
Трансплантология. Руководство для врачей / Под редакцией академика В.И. Шумакова. - Москва.- Медицинское информационное агентство.- 2006.- 540 с.
Тырин В.В. Пункционная биопсия трансплантированной почки в интерпретации ее дисфункции и выборе тактики лечения / Автореферат диссертации … доктора медицинских наук. - Москва.- 2006.- 50 с.
Suhorukov Vadim. The role of core biopsy in kidney graft pathology diagnostics / Summary of Doctoral Thesis for obtaining a Doctor of Medicine degree Speciality - Transplantation. - Riga.- 2011.- 38 p.
Столяревич Е.С. Хроническая дисфункция трансплантированной почки: морфологическая картина, особенности течения, подходы к профилактике и лечению / Автореферат диссертации … доктора медицинских наук. - Москва. - 2010.- 48 с.
Столяревич Е.С. Хроническая трансплантационная нефропатия: клинико-морфологические сопоставления и факторы прогрессирования / Автореферат диссертации … кандидата медицинских наук. - Москва.- 2002.- 25 с.
Малов И.П. Гистологическое и иммуноморфологическое исследование аллотрансплантированных почек в позднем послеоперационном периоде / Автореферат диссертации … кандидата медицинских наук. - Москва. -2002.- 27 с.
Шумаков В.И., Ильинский И.М., Белецкая Л.В., Малов И.П., Тырин В.В., Зайденов В.А., Томилина Н.А. Гистологическое и иммуноморфологическое исследование хронического отторжения аллотрансплантированных почек // Вестник трансплантологии и искусственных органов. - 2000.-N 3.- С. 30-34.
Шумаков В.И., Малов И.П., Ильинский И.М., Тырин В.В., Белецкая Л.В., Зайденов В.В., Томилина Н.А., Гордюшина В.С. Виды патологии аллотрансплантированных трупных почек в позднем послеоперационном периоде по данным исследования пункционных биоптатов // Вестник трансплантологии и искусственных органов. - 2000.- N 1.- C. 11-14.
Ротова И.Д. Гистологическая и иммуногистохимическая диагностика цитомегаловирусной инфекции в пункционных биоптатах аллотрансплантированных почек / Автореферат диссертации … кандидата медицинских наук. - Москва.- 2007.- 23 с.
Pham PT, Pham PM, Pham SV, Pham PA, Pham PC. New onset diabetes after transplantation (NODAT): an overview. Diabetes Metab Syndr Obes. 2011;4:175-86. doi: 10.2147/DMSO.S19027.
Vincenti F, Friman S, Scheuermann E, Rostaing L, Jenssen T, Campistol JM, Uchida K, Pescovitz MD, Marchetti P, Tuncer M, Citterio F, Wiecek A, Chadban S, El-Shahawy M, Budde K, Goto N; DIRECT (Diabetes Incidence after Renal Transplantation: Neoral C Monitoring Versus Tacrolimus) Investigators. Results of an international, randomized trial comparing glucose metabolism disorders and outcome with cyclosporine versus tacrolimus. Am J Transplant. 2007 Jun;7(6):1506-14. doi: 10.1111/j.1600-6143.2007.01749.x.
Kasiske BL, Snyder JJ, Gilbertson D, Matas AJ. Diabetes mellitus after kidney transplantation in the United States. Am J Transplant. 2003 Feb;3(2):178-85. doi: 10.1034/j.1600-6143.2003.00010.x. PMID: 12603213.
Ojo AO. Cardiovascular complications after renal transplantation and their prevention. Transplantation. 2006 Sep 15;82(5):603-11. doi: 10.1097/01.tp.0000235527.81917.fe. PMID: 16969281.
Hjelmesaeth J, Hartmann A, Leivestad T, Holdaas H, Sagedal S, Olstad M, Jenssen T. The impact of early-diagnosed new-onset post-transplantation diabetes mellitus on survival and major cardiac events. Kidney Int. 2006 Feb;69(3):588-95. doi: 10.1038/sj.ki.5000116. PMID: 16395250.].
Spoto B, Pisano A, Zoccali C. Insulin resistance in chronic kidney disease: a systematic review. Am J Physiol Renal Physiol. 2016 Dec 1;311(6):F1087-F1108. doi: 10.1152/ajprenal.00340.2016. Epub 2016 Oct 5. PMID: 27707707.
Thomas G, Sehgal AR, Kashyap SR, Srinivas TR, Kirwan JP, Navaneethan SD. Metabolic syndrome and kidney disease: a systematic review and meta-analysis. Clin J Am Soc Nephrol. 2011 Oct;6(10):2364-73. doi: 10.2215/CJN.02180311. Epub 2011 Aug 18. PMID: 21852664; PMCID: PMC3186450.
Van Loo, A.A., et al. Pretransplantation hemodialysis strategy influences early renal graft function. J Am Soc Nephrol, 1998. 9: 473. https://www.ncbi.nlm.nih.gov/pubmed/9513911
Abramowicz, D., et al. European Renal Best Practice Guideline on kidney donor and recipient evaluation and perioperative care. Nephrol Dial Transplant, 2015. 30: 1790. https://www.ncbi.nlm.nih.gov/pubmed/25007790
Task Force for Preoperative Cardiac Risk. Guidelines for pre-operative cardiac risk assessment and perioperative cardiac management in non-cardiac surgery. Eur Heart J, 2009. 30: 2769. https://academic.oup.com/eurheartj/article/30/22/2769/478458
Benahmed, A., et al. Ticlopidine and clopidogrel, sometimes combined with aspirin, only minimally increase the surgical risk in renal transplantation: A case-control study. Nephrol Dial Transplant, 2014. 29: 463. https://www.ncbi.nlm.nih.gov/pubmed/24275542
Osman, Y., et al. Necessity of Routine Postoperative Heparinization in Non-Risky Live-Donor Renal Transplantation: Results of a Prospective Randomized Trial. Urology, 2007. 69: 647. https://www.ncbi.nlm.nih.gov/pubmed/17445644
Guerra R, Kawano PR, Amaro MP, Yamamoto HA, Gomes Filho FF, Amaro JL, El Dib RP, Garcia-Perdomo HA, Reis LO. Acute graft thrombosis in patients who underwent renal transplant and received anticoagulant or antiplatelet agents. A systematic review and meta-analysis. Am J Clin Exp Urol. 2022 Jun 15;10(3):129-141. PMID: 35874286; PMCID: PMC9301061.
Surianarayanan V, Hoather TJ, Tingle SJ, Thompson ER, Hanley J, Wilson CH. Interventions for preventing thrombosis in solid organ transplant recipients. Cochrane Database Syst Rev. 2021 Mar 15;3(3):CD011557. doi: 10.1002/14651858.CD011557.pub2. PMID: 33720396; PMCID: PMC8094924.
Orlando, G., et al. One-shot versus multidose perioperative antibiotic prophylaxis after kidney transplantation: a randomized, controlled clinical trial. Surgery, 2015. 157: 104. https://www.ncbi.nlm.nih.gov/pubmed/25304836
Choi, S.U., et al. Clinical significance of prophylactic antibiotics in renal transplantation. Transplant Proc, 2013. 45: 1392. https://www.ncbi.nlm.nih.gov/pubmed/23726580
Chan S, Ng S, Chan HP, Pascoe EM, Playford EG, Wong G, Chapman JR, Lim WH, Francis RS, Isbel NM, Campbell SB, Hawley CM, Johnson DW. Perioperative antibiotics for preventing post-surgical site infections in solid organ transplant recipients. Cochrane Database Syst Rev. 2020 Aug 4;8(8):CD013209. doi: 10.1002/14651858.CD013209.pub2. PMID: 32799356; PMCID: PMC7437398.
O’Malley, C.M., et al. A randomized, double-blind comparison of lactated Ringer’s solution and 0.9% NaCl during renal transplantation. Anesth Analg, 2005. 100: 1518. https://www.ncbi.nlm.nih.gov/pubmed/15845718
Othman, M.M., et al. The impact of timing of maximal crystalloid hydration on early graft function during kidney transplantation. Anesth Analg, 2010. 110: 1440. https://www.ncbi.nlm.nih.gov/pubmed/20418304
Dalton, R.S., et al. Physiologic impact of low-dose dopamine on renal function in the early post renal transplant period. Transplantation, 2005. 79: 1561. https://www.ncbi.nlm.nih.gov/pubmed/15940046
Ciapetti, M., et al. Low-dose dopamine in kidney transplantation. Transplant Proc, 2009. 41: 4165. https://www.ncbi.nlm.nih.gov/pubmed/20005360
Chedid, M.F., et al. Living donor kidney transplantation using laparoscopically procured multiple renal artery kidneys and right kidneys. J Am Coll Surg, 2013. 217: 144.
Dalton, R.S., et al. Physiologic impact of low-dose dopamine on renal function in the early post renal transplant period. Transplantation, 2005. 79: 1561. https://pubmed.ncbi.nlm.nih.gov/15940046
Ciapetti, M., et al. Low-dose dopamine in kidney transplantation. Transplant Proc, 2009. 41: 4165. https://pubmed.ncbi.nlm.nih.gov/20005360
Hanif, F., et al. Outcome of renal transplantation with and without intra-operative diuretics. Int J Surg, 2011. 9: 460
Joseph S. et al. Guidelines on the use of therapeutic apheresis in clinical practice – evidence-based approach from the writing committee of the American Society for Apheresis: the 7th special issue. Journal of Clinical Apheresis 2016. 31:149-338.
Мойсюк Я.Г., Сушков А.И. Несовместимые по группе крови родственные трансплантации почки: отдаленные результаты. Альманах клинической медицины. 2017;45(7):535-546. https://doi.org/10.18786/2072-0505-2017-45-7-535-546.
Veroux M, Zerbo D, Basile G, et al. Simultaneous Native Nephrectomy and Kidney Transplantation in Patients With Autosomal Dominant Polycystic Kidney Disease. PLoS One. 2016; 11: e0155481.
Chebib FT, Prieto M, Jung Y, et al. Native Nephrectomy in Renal Transplant Recipients with Autosomal Dominant Polycystic Kidney Disease. Transplant Direct. 2015; 1: e43.
Ahmad SB, Inouye B, Phelan MS, et al. Live Donor Renal Transplant With Simultaneous Bilateral Nephrectomy for Autosomal Dominant Polycystic Kidney Disease Is Feasible and Satisfactory at Long-term Follow-up. Transplantation. 2016; 100: 407–415.
Биктимиров, Т. Р. Оперативное лечение аутосомно-доминантного поликистоза почек / Т. Р. Биктимиров, А. Г. Мартов, Р. Г. Биктимиров, А. В. Баранов, И. А. Милосердов, А. А. Капутовский, А. М. Хитрых // Урология. – 2021. – № 4. – С. 121–125. DOI: 10.18565/urology.2021.4.121-125
Hajj P, Ferlicot S, Massoud W, et al. Prevalence of renal cell carcinoma in patients with autosomal dominant polycystic kidney disease and chronic renal failure. Urology, 2009, 74, 631-634.
Phelan, P.J., et al. Left versus right deceased donor renal allograft outcome. Transpl Int, 2009. 22: 1159. https://www.ncbi.nlm.nih.gov/pubmed/19891044
Ciudin, A., et al. Transposition of iliac vessels in implantation of right living donor kidneys. Transplant Proc, 2012. 44: 2945. https://www.ncbi.nlm.nih.gov/pubmed/23195003
Feng, J.Y., et al. Renal vein lengthening using gonadal vein reduces surgical difficulty in living-donor kidney transplantation. World J Surg, 2012. 36: 468. https://www.ncbi.nlm.nih.gov/pubmed/21882021
Nghiem, D.D. Use of spiral vein graft in living donor renal transplantation. Clin Transplant, 2008. 22: 719. https://www.ncbi.nlm.nih.gov/pubmed/18673376
Matheus, W.E., et al. Kidney transplant anastomosis: internal or external iliac artery? Urol J, 2009. 6: 260. https://www.ncbi.nlm.nih.gov/pubmed/20027554.
Галеев, Ш. Р. Пересадка почки при вариантных формах почечных сосудов : специальность 14.00.27 : диссертация на соискание ученой степени кандидата медицинских наук / Галеев Шамиль Ринатович. – Казань, 2005. – 104 с. – EDN NPZQCN.
El-Sherbiny, M., et al. The use of the inferior epigastric artery for accessory lower polar artery revascularization in live donor renal transplantation. Int Urol Nephrol, 2008. 40: 283. https://www.ncbi.nlm.nih.gov/pubmed/17721826
Firmin, L.C., et al. The use of explanted internal iliac artery grafts in renal transplants with multiple arteries. Transplantation, 2010. 89: 766. https://www.ncbi.nlm.nih.gov/pubmed/20308866
Oertl, A.J., et al. Saphenous vein interposition as a salvage technique for complex vascular situations during renal transplantation. Transplant Proc, 2007. 39: 140. https://www.ncbi.nlm.nih.gov/pubmed/17275492
Alberts, V.P., et al. Ureterovesical anastomotic techniques for kidney transplantation: a systematic review and meta-analysis. Transpl Int, 2014. 27: 593. https://www.ncbi.nlm.nih.gov/pubmed/24606191
Slagt, I.K., et al. A randomized controlled trial comparing intravesical to extravesical ureteroneocystostomy in living donor kidney transplantation recipients. Kidney Int, 2014. 85: 471. https://www.ncbi.nlm.nih.gov/pubmed/24284515
Dadkhah, F., et al. Modified ureteroneocystostomy in kidney transplantation to facilitate endoscopic management of subsequent urological complications. Int Urol Nephrol, 2010. 42: 285. https://www.ncbi.nlm.nih.gov/pubmed/19760513
Сайдулаев Д.А., Милосердов И.А., Готье С.В. Профилактика и хирургические методы лечения урологических осложнений у реципиентов почки. Вестник трансплантологии и искусственных органов. 2019;21(3):166-173. https://doi.org/10.15825/1995-1191-2019-3-166-173
Timsit, M.O., et al. Should routine pyeloureterostomy be advocated in adult kidney transplantation? A prospective study of 283 recipients. J Urol, 2010. 184: 2043. https://www.ncbi.nlm.nih.gov/pubmed/20850818
Kehinde, E.O., et al. Complications associated with using nonabsorbable sutures for ureteroneocystostomy in renal transplant operations. Transplant Proc, 2000. 32: 1917. https://www.ncbi.nlm.nih.gov/pubmed/11119999
Сайдулаев Д.А., Садовников С.В., Биктимиров Р.Г., Гаджиева П.М., Милосердов И.А. Успешные клинические случаи реконструктивно пластических лапароскопических операций на мочеточнике трансплантированной почки. Вестник трансплантологии и искусственных органов. 2021;23(3):61-65. https://doi.org/10.15825/1995-1191-2021-3-61-65
Галеев Р.Х. Полное замещение мочеточника лоскутом мочевого пузыря (операция Боари) после пересадки донорской почки / Р.Х. Галеев, Р.Ш. Гильмутдинов, Д.А. Назаров, С.П. Мартыненко // Урология. - 2003. - №3. - С.58-60.
Лопаткин Н.А. Урологические осложнения при трансплантаци почки / Н.А. Лопаткин, М.Ф.Трапезникова, Д.В.Перлин [и др.]. - М.: Издательский дом ГЭОТАР-МЕД, 2004. - 224 c.
Wilson, C.H., et al. Routine intraoperative ureteric stenting for kidney transplant recipients. Cochrane Database Syst Rev, 2013: CD004925. https://www.ncbi.nlm.nih.gov/pubmed/23771708
Tavakoli, A., et al. Impact of stents on urological complications and health care expenditure in renal transplant recipients: results of a prospective, randomized clinical trial. J Urol, 2007. 177: 2260. https://www.ncbi.nlm.nih.gov/pubmed/17509336.
Heidari, M., et al. Transplantation of kidneys with duplicated ureters. Scand J Urol Nephrol, 2010. 44: 337. https://www.ncbi.nlm.nih.gov/pubmed/20653492
Alberts, V.P., et al. Duplicated ureters and renal transplantation: a case-control study and review of the literature. Transplant Proc, 2013. 45: 3239. https://www.ncbi.nlm.nih.gov/pubmed/24182792
Roach, J. P., Bock, M. E., & Goebel, J. (2017). Pediatric kidney transplantation. Seminars in Pediatric Surgery, 26(4), 233–240. doi:10.1053/j.sempedsurg.2017.07.006.
Ghane Sharbaf F, Bitzan M, Szymanski KM, et al. Native nephrectomy prior to pediatric kidney transplantation: biological and clinical aspects. Pediatr Nephrol. 2012; 27: 1179–1188.
Dimitroulis, D., et al. Vascular complications in renal transplantation: a single-center experience in 1367 renal transplantations and review of the literature. Transplant Proc, 2009. 41: 1609. https://www.ncbi.nlm.nih.gov/pubmed/19545690
Pawlicki, J., et al. Risk factors for early hemorrhagic and thrombotic complications after kidney transplantation. Transplant Proc, 2011. 43: 3013. https://www.ncbi.nlm.nih.gov/pubmed/21996213
Rouviere, O., et al. Acute thrombosis of renal transplant artery: graft salvage by means of intra-arterial fibrinolysis. Transplantation, 2002. 73: 403. https://www.ncbi.nlm.nih.gov/pubmed/11884937
Domagala, P., et al. Complications of transplantation of kidneys from expanded-criteria donors. Transplant Proc, 2009. 41: 2970. https://www.ncbi.nlm.nih.gov/pubmed/19857652
Giustacchini, P., et al. Renal vein thrombosis after renal transplantation: an important cause of graft loss. Transplant Proc, 2002. 34: 2126. https://www.ncbi.nlm.nih.gov/pubmed/12270338
Wuthrich, R.P. Factor V Leiden mutation: potential thrombogenic role in renal vein, dialysis graft and transplant vascular thrombosis. Curr Opin Nephrol Hypertens, 2001. 10: 409. https://www.ncbi.nlm.nih.gov/pubmed/11342806
Parajuli, S., et al. Hypercoagulability in Kidney Transplant Recipients. Transplantation, 2016. 100: 719. https://www.ncbi.nlm.nih.gov/pubmed/26413991
Granata, A., et al. Renal transplant vascular complications: the role of Doppler ultrasound. J Ultrasound, 2015. 18: 101. https://www.ncbi.nlm.nih.gov/pubmed/26191097
Hogan, J.L., et al. Late-onset renal vein thrombosis: A case report and review of the literature. Int J Surg Case Rep, 2015. 6C: 73. https://www.ncbi.nlm.nih.gov/pubmed/25528029
Hurst, F.P., et al. Incidence, predictors and outcomes of transplant renal artery stenosis after kidney transplantation: analysis of USRDS. Am J Nephrol, 2009. 30: 459. https://www.ncbi.nlm.nih.gov/pubmed/19776559
Willicombe, M., et al. Postanastomotic transplant renal artery stenosis: association with de novo class II donor-specific antibodies. Am J Transplant, 2014. 14: 133. https://www.ncbi.nlm.nih.gov/pubmed/24354873
Ghazanfar, A., et al. Management of transplant renal artery stenosis and its impact on long-term allograft survival: a single-centre experience. Nephrol Dial Transplant, 2011. 26: 336. https://www.ncbi.nlm.nih.gov/pubmed/20601365
Seratnahaei, A., et al. Management of transplant renal artery stenosis. Angiology, 2011. 62: 219. https://www.ncbi.nlm.nih.gov/pubmed/20682611
Atray, N.K., et al. Post transplant lymphocele: a single centre experience. Clin Transplant, 2004. 18 Suppl 12: 46. https://www.ncbi.nlm.nih.gov/pubmed/15217407
Ulrich, F., et al. Symptomatic lymphoceles after kidney transplantation - multivariate analysis of risk factors and outcome after laparoscopic fenestration. Clin Transplant, 2010. 24: 273. https://www.ncbi.nlm.nih.gov/pubmed/19719727
Lucewicz, A., et al. Management of primary symptomatic lymphocele after kidney transplantation: a systematic review. Transplantation, 2011. 92: 663. https://www.ncbi.nlm.nih.gov/pubmed/21849931
Capocasale, E., et al. Octreotide in the treatment of lymphorrhea after renal transplantation: a preliminary experience. Transplant Proc, 2006. 38: 1047. https://www.ncbi.nlm.nih.gov/pubmed/16757259
Kayler, L., et al. Kidney transplant ureteroneocystostomy techniques and complications: review of the literature. Transplant Proc, 2010. 42: 1413. https://www.ncbi.nlm.nih.gov/pubmed/20620446
Secin, F.P., et al. Comparing Taguchi and Lich-Gregoir ureterovesical reimplantation techniques for kidney transplants. J Urol, 2002. 168: 926. https://www.ncbi.nlm.nih.gov/pubmed/12187192
Dinckan, A., et al. Early and late urological complications corrected surgically following renal transplantation. Transpl Int, 2007. 20: 702. https://www.ncbi.nlm.nih.gov/pubmed/17511829
Kumar, A., et al. Evaluation of the urological complications of living related renal transplantation at a single center during the last 10 years: impact of the Double-J* stent. J Urol, 2000. 164: 657. https://www.ncbi.nlm.nih.gov/pubmed/10953120
Mazzucchi, E., et al. Primary reconstruction is a good option in the treatment of urinary fistula after kidney transplantation. Int Braz J Urol, 2006. 32: 398. https://www.ncbi.nlm.nih.gov/pubmed/16953905
Davari, H.R., et al. Urological complications in 980 consecutive patients with renal transplantation. Int J Urol, 2006. 13: 1271. https://www.ncbi.nlm.nih.gov/pubmed/17010003
Sabnis, R.B., et al. The development and current status of minimally invasive surgery to manage urological complications after renal transplantation. Indian J Urol, 2016. 32: 186. https://www.ncbi.nlm.nih.gov/pubmed/27555675
Suttle, T., et al. Comparison of Urologic Complications Between Ureteroneocystostomy and Ureteroureterostomy in Renal Transplant: A Meta-Analysis. Exp Clin Transplant, 2016. 14: 276. https://www.ncbi.nlm.nih.gov/pubmed/26925612
Breda, A., et al. Incidence of ureteral strictures after laparoscopic donor nephrectomy. J Urol, 2006. 176: 1065. https://www.ncbi.nlm.nih.gov/pubmed/16890691
Kaskarelis, I., et al. Ureteral complications in renal transplant recipients successfully treated with interventional radiology. Transplant Proc, 2008. 40: 3170. https://www.ncbi.nlm.nih.gov/pubmed/19010224
He, B. Classification of ureteral stenosis and associated strategy for treatment after kidney transplant / B. He, A. Bremner, Y. Han. – Текст : непосредственный // Experimental and Clinical Transplantation. – 2013. – Vol. 11. – Iss. 2. – P. 122–127. doi: 10.6002/ect.2012.0179.
Kristo, B., et al. Treatment of renal transplant ureterovesical anastomotic strictures using antegrade balloon dilation with or without holmium:YAG laser endoureterotomy. Urology, 2003. 62: 831. https://www.ncbi.nlm.nih.gov/pubmed/14624903
Nie, Z., et al. Comparison of urological complications with primary ureteroureterostomy versus conventional ureteroneocystostomy. Clin Transplant, 2010. 24: 615. https://www.ncbi.nlm.nih.gov/pubmed/19925475
Chaykovska, L., et al. Kidney transplantation into urinary conduits with ureteroureterostomy between transplant and native ureter: single-center experience. Urology, 2009. 73: 380. https://www.ncbi.nlm.nih.gov/pubmed/19022489
Helfand, B.T., et al. Reconstruction of late-onset transplant ureteral stricture disease. BJU Int, 2011. 107: 982. https://www.ncbi.nlm.nih.gov/pubmed/20825404
Liu, Y., et al. Basiliximab or antithymocyte globulin for induction therapy in kidney transplantation: a meta-analysis. Transplant Proc, 2010. 42: 1667. https://www.ncbi.nlm.nih.gov/pubmed/20620496
Sun, Z.J., et al. Efficacy and Safety of Basiliximab Versus Daclizumab in Kidney Transplantation: A Meta-Analysis. Transplant Proc, 2015. 47: 2439. https://www.ncbi.nlm.nih.gov/pubmed/26518947
216Webster, A.C., et al. Interleukin 2 receptor antagonists for kidney transplant recipients. Cochrane Database Syst Rev, 2010: CD003897. https://www.ncbi.nlm.nih.gov/pubmed/20091551
Bamoulid, J., et al. Immunosuppression and Results in Renal Transplantation. Eur UrolSuppl,2016. 15: 415. https://www.sciencedirect.com/science/article/pii/S1569905616300823
Kidney Disease Improving Global Outcomes Transplant Work Group. KDIGO clinical practice guideline for the care of kidney transplant recipients. Am J Transplant, 2009. 9 Suppl 3: S1. https://www.ncbi.nlm.nih.gov/pubmed/19845597
Jones-Hughes, T., et al. Immunosuppressive therapy for kidney transplantation in adults: a systematic review and economic model. Health Technol Assess, 2016. 20: 1. https://www.ncbi.nlm.nih.gov/pubmed/27578428
Bamoulid, J., et al. Anti-thymocyte globulins in kidney transplantation: focus on current indications and long-term immunological side effects. Nephrol Dial Transplant, 2016. https://www.ncbi.nlm.nih.gov/pubmed/27798202
Malvezzi, P., et al. Induction by anti-thymocyte globulins in kidney transplantation: a review of the literature and current usage. J Nephropathol, 2015. 4: 110. https://www.ncbi.nlm.nih.gov/pubmed/26457257
Nashan B. Review of the proliferation inhibitor everolimus. ExpertOpin Investig Drugs, 2002; 11: 1845–1857.
Knight S.R., Morris P.J. Does the evidence support the use of mycophenolate mofetil therapeutic drug monitoring in clinical practice? A systematic review. Transplantation, 2008; 85: р.1675–1685.
Kyllonen L.E., Salmela K.T.. Early cyclosporine C0 and C2 monitoring in de novo kidney transplant patients: A prospective randomized single-center pilot study. Transplantation, 2006; 81: 1010–1015.
Bamoulid, J., et al. The need for minimization strategies: current problems of immunosuppression. Transpl Int, 2015. 28: 891. https://www.ncbi.nlm.nih.gov/pubmed/25752992
Leas, B.F., et al., in Calcineurin Inhibitors for Renal Transplant. 2016: Rockville.
Webster, A.C., et al. Tacrolimus versus ciclosporin as primary immunosuppression for kidney transplant recipients: meta-analysis and meta-regression of randomised trial data. BMJ, 2005. 331: 810. https://www.ncbi.nlm.nih.gov/pubmed/16157605.
Sawinski, D., et al. Calcineurin Inhibitor Minimization, Conversion, Withdrawal, and Avoidance Strategies in Renal Transplantation: A Systematic Review and Meta-Analysis. Am J Transplant, 2016. 16: 2117. https://www.ncbi.nlm.nih.gov/pubmed/26990455.
Caillard, S., et al. Advagraf((R)), a once-daily prolonged release tacrolimus formulation, in kidney transplantation: literature review and guidelines from a panel of experts. Transpl Int, 2016. 29: 860. https://www.ncbi.nlm.nih.gov/pubmed/26373896.
McCormack, P.L. Extended-release tacrolimus: a review of its use in de novo kidney transplantation. Drugs, 2014. 74: 2053. https://www.ncbi.nlm.nih.gov/pubmed/25352392.
Molnar, A.O., et al. Generic immunosuppression in solid organ transplantation: systematic review and meta-analysis. BMJ, 2015. 350: h3163. https://www.ncbi.nlm.nih.gov/pubmed/26101226.
Staatz, C.E., et al. Clinical Pharmacokinetics of Once-Daily Tacrolimus in Solid-Organ Transplant Patients. Clin Pharmacokinet, 2015. 54: 993. https://www.ncbi.nlm.nih.gov/pubmed/26038096.
van Gelder, T., et al. European Society for Organ Transplantation Advisory Committee recommendations on generic substitution of immunosuppressive drugs. Transpl Int, 2011. 24: 1135. https://www.ncbi.nlm.nih.gov/pubmed/22032583.
Diekmann, F. Immunosuppressive minimization with mTOR inhibitors and belatacept. Transpl Int, 2015. 28: 921. https://www.ncbi.nlm.nih.gov/pubmed/25959589.
Burton SA, Amir N, Asbury A, Lange A, Hardinger KL. Treatment of antibody-mediated rejection in renal transplant patients: a clinical practice survey. Clin Transplant 2015;29;118-123.
Ruangkanchanasetr P et al. Intensive plasmapheresis and intravenous immunoglobulin for treatment of antibody-mediated rejection after kidney transplant. Exp Clin Transplant 2014;12;328-333.
Сушков А.И., Шаршаткин А.В. Трудные решения при лечении острого гуморального отторжения пересаженной почки. Вестник трансплантологии и искусственных органов. 2016;18(2):125-130. https://doi.org/10.15825/1995-1191-2016-2-125-130
Kamar, N., et al. Calcineurin inhibitor-sparing regimens based on mycophenolic acid after kidney transplantation. Transpl Int, 2015. 28: 928. https://www.ncbi.nlm.nih.gov/pubmed/25557802.
Snanoudj, R., et al. Immunological risks of minimization strategies. Transpl Int, 2015. 28: 901. https://www.ncbi.nlm.nih.gov/pubmed/25809144.
Budde, K., et al. Enteric-coated mycophenolate sodium. Expert Opin Drug Saf, 2010. 9: 981. https://www.ncbi.nlm.nih.gov/pubmed/20795786.
Cooper, M., et al. Enteric-coated mycophenolate sodium immunosuppression in renal transplant patients: efficacy and dosing. Transplant Rev (Orlando), 2012. 26: 233. https://www.ncbi.nlm.nih.gov/pubmed/22863029.
Staatz, C.E., et al. Pharmacology and toxicology of mycophenolate in organ transplant recipients: an update. Arch Toxicol, 2014. 88: 1351. https://www.ncbi.nlm.nih.gov/pubmed/24792322.
van Gelder, T., et al. Mycophenolate revisited. Transpl Int, 2015. 28: 508. https://www.ncbi.nlm.nih.gov/pubmed/25758949.
Wagner, M., et al. Mycophenolic acid versus azathioprine as primary immunosuppression for kidney transplant recipients. Cochrane Database Syst Rev, 2015: CD007746. https://www.ncbi.nlm.nih.gov/pubmed/26633102.
Hirsch, H.H., et al. European perspective on human polyomavirus infection, replication and disease in solid organ transplantation. Clin Microbiol Infect, 2014. 20 Suppl 7: 74. https://www.ncbi.nlm.nih.gov/pubmed/24476010.
Le Meur, Y., et al. Therapeutic drug monitoring of mycophenolates in kidney transplantation: report of The Transplantation Society consensus meeting. Transplant Rev (Orlando), 2011. 25: 58. https://www.ncbi.nlm.nih.gov/pubmed/21454067.
Mathis, A.S., et al. Calcineurin inhibitor sparing strategies in renal transplantation, part one: Late sparing strategies. World J Transplant, 2014. 4: 57. https://www.ncbi.nlm.nih.gov/pubmed/25032096.
Haller, M.C., et al. Steroid avoidance or withdrawal for kidney transplant recipients. Cochrane Database Syst Rev, 2016: CD005632. https://www.ncbi.nlm.nih.gov/pubmed/27546100.
Kunz, R., et al. Maintenance therapy with triple versus double immunosuppressive regimen in renal transplantation: a meta-analysis. Transplantation, 1997. 63: 386. https://www.ncbi.nlm.nih.gov/pubmed/9039928.
Halleck, F., et al. An evaluation of sirolimus in renal transplantation. Expert Opin Drug Metab Toxicol, 2012. 8: 1337. https://www.ncbi.nlm.nih.gov/pubmed/22928953.
Ventura-Aguiar, P., et al. Safety of mTOR inhibitors in adult solid organ transplantation. Expert Opin Drug Saf, 2016. 15: 303. https://www.ncbi.nlm.nih.gov/pubmed/26667069.
Witzke, O., et al. Everolimus immunosuppression in kidney transplantation: What is the optimal strategy? Transplant Rev (Orlando), 2016. 30: 3. https://www.ncbi.nlm.nih.gov/pubmed/26603484.
Xie, X., et al. mTOR inhibitor versus mycophenolic acid as the primary immunosuppression regime combined with calcineurin inhibitor for kidney transplant recipients: a meta-analysis. BMC Nephrol, 2015. 16: 91. https://www.ncbi.nlm.nih.gov/pubmed/26126806.
Shipkova, M., et al. Therapeutic Drug Monitoring of Everolimus: A Consensus Report. Ther Drug Monit, 2016. 38: 143. https://www.ncbi.nlm.nih.gov/pubmed/26982492.
Liefeldt, L., et al. Donor-specific HLA antibodies in a cohort comparing everolimus with cyclosporine after kidney transplantation. Am J Transplant, 2012. 12: 1192. https://www.ncbi.nlm.nih.gov/pubmed/22300538.
Halleck, F., et al. Transplantation: Sirolimus for secondary SCC prevention in renal transplantation. Nat Rev Nephrol, 2012. 8: 687. https://www.ncbi.nlm.nih.gov/pubmed/23026948.
Ponticelli, C., et al. Skin cancer in kidney transplant recipients. J Nephrol, 2014. 27: 385. https://www.ncbi.nlm.nih.gov/pubmed/24809813.
Ho J, Okoli GN, Rabbani R, Lam OLT, Reddy VK, Askin N, Rampersad C, Trachtenberg A, Wiebe C, Nickerson P, Abou-Setta AM. Effectiveness of T cell-mediated rejection therapy: A systematic review and meta-analysis. Am J Transplant. 2022 Mar;22(3):772-785. doi: 10.1111/ajt.16907. Epub 2021 Dec 10. PMID: 34860468; PMCID: PMC9300092.
Gray D, Shepherd H, Daar A, Oliver DO, Morris PJ. Oral versus intravenous high-dose steroid treatment of renal allograft rejection. The big shot or not? Lancet. 1978 Jan 21;1(8056):117-8. doi: 10.1016/s0140-6736(78)90417-8. PMID: 87551.
Stromstad SA, Kauffman HM, Sampson D, Stawicki AT. Randomized steroid therapy of human kidney transplant rejection. Surg Forum. 1978;29:376-7.
Kauffman HM Jr, Stromstad SA, Sampson D, Stawicki AT. Randomized steroid therapy of human kidney transplant rejection. Transplant Proc. 1979 Mar;11(1):36-8.
Lui SF, Sweny P, Scoble JE, Varghese Z, Moorhead JF, Fernando ON. Low-dose vs high-dose intravenous methylprednisolone therapy for acute renal allograft rejection in patients receiving cyclosporin therapy. Nephrol Dial Transplant. 1989;4(5):387-9. doi: 10.1093/oxfordjournals.ndt.a091895.].
Webster AC, Pankhurst T, Rinaldi F, Chapman JR, Craig JC. Monoclonal and polyclonal antibody therapy for treating acute rejection in kidney transplant recipients: a systematic review of randomized trial data. Transplantation. 2006;81:953–965. doi: 10.1097/01.tp.0000215178.72344.9d.]
Eikmans M, Roelen DL, Claas FH. Molecular monitoring for rejection and graft outcome in kidney transplantation. Expert Opin Med Diagn. 2008;2:1365–1379. doi: 10.1517/17530050802600683.
Shinn C, Malhotra D, Chan L, Cosby RL, Shapiro JI. Time course of response to pulse methylprednisolone therapy in renal transplant recipients with acute allograft rejection. Am J Kidney Dis. 1999;34:304–307. doi: 10.1016/s0272-6386(99)70359-8.
Böhmig GA, Wahrmann M, Regele H, et al. Immunoadsorption in severe C4d-positive acute kidney allograft rejection: a randomized controlled trial. Am J Transplant. 2007;7:117–121.
Bonomini V, Vangelista A, Frascà GM, et al. Effects of plasmapheresis in renal transplant rejection: a controlled study. Trans Am Soc Artif Intern Organs. 1985;31:698–703.
Blake P, Sutton D, Cardella CJ. Plasma exchange in acute renal transplant rejection. Prog Clin Biol Res. 1990;337:249–252
Wan SS, Ying TD, Wyburn K, Roberts DM, Wyld M, Chadban SJ. The Treatment of Antibody-Mediated Rejection in Kidney Transplantation: An Updated Systematic Review and Meta-Analysis. Transplantation. 2018 Apr;102(4):557-568. doi: 10.1097/TP.0000000000002049.
Böhmig GA, Wahrmann M, Regele H, et al. Immunoadsorption in severe c4d-positive acute kidney allograft rejection: a randomized controlled trial. Am J Transplant. 2007;7:117–121.
Lee CY, Lin WC, Wu MS, et al. Repeated cycles of high-dose intravenous immunoglobulin and plasmapheresis for treatment of late antibody-mediated rejection of renal transplants. J Formos Med Assoc. 2016; 115:845–852
Schinstock CA, Mannon RB, Budde K, Chong AS, Haas M, Knechtle S, Lefaucheur C, Montgomery RA, Nickerson P, Tullius SG, Ahn C, Askar M, Crespo M, Chadban SJ, Feng S, Jordan SC, Man K, Mengel M, Morris RE, O'Doherty I, Ozdemir BH, Seron D, Tambur AR, Tanabe K, Taupin JL, O'Connell PJ. Recommended Treatment for Antibody-mediated Rejection After Kidney Transplantation: The 2019 Expert Consensus From the Transplantion Society Working Group. Transplantation. 2020;104(5):911-922. doi: 10.1097/TP.0000000000003095.
Roberts DM, Jiang SH, Chadban SJ. The treatment of acute antibody-mediated rejection in kidney transplant recipients-a systematic review. Transplantation. 2012;94:775–783.
Wan SS, Ying TD, Wyburn K, et al. The treatment of antibody-mediated rejection in kidney transplantation: an updated systematic review and meta-analysis. Transplantation. 2018;102:557–568.
Lefaucheur C, Loupy A, Vernerey D, et al. Antibody-mediated vascular rejection of kidney allografts: a population-based study. Lancet. 2013;381:313–319.]
Vo AA, Lukovsky M, Toyoda M, et al. Rituximab and intravenous immune globulin for desensitization during renal transplantation. N Engl J Med. 2008;359:242–251.
Федеральный закон "Об основах охраны здоровья граждан в Российской Федерации" от 21.11.2011 N 323-ФЗ
Heiwe S, Jacobson SH. Exercise training in adults with CKD: a systematic review and meta-analysis. Am J Kidney Dis. 2014 Sep;64(3):383-93. doi: 10.1053/j.ajkd.2014.03.020. Epub 2014 Jun 7. PMID: 24913219.
Williams AD, Fassett RG, Coombes JS. Exercise in CKD: why is it important and how should it be delivered? Am J Kidney Dis. 2014 Sep;64(3):329-31. doi: 10.1053/j.ajkd.2014.06.004. PMID: 25150853.
Pei G, Tang Y, Tan L, Tan J, Ge L, Qin W. Aerobic exercise in adults with chronic kidney disease (CKD): a meta-analysis. Int Urol Nephrol. 2019 Oct;51(10):1787-1795. doi: 10.1007/s11255-019-02234-x. Epub 2019 Jul 22. PMID: 31332699.
Parker R, Armstrong MJ, Corbett C, Day EJ, Neuberger JM. Alcohol and substance abuse in solid-organ transplant recipients. Transplantation. 2013 Dec 27;96(12):1015-24. doi: 10.1097/TP.0b013e31829f7579. PMID: 24025323.
Zwaan M, Erim Y, Kröncke S, Vitinius F, Buchholz A, Nöhre M; guideline group “Psychosocial Diagnosis and Treatment of Patients before and after Organ Transplantation”*. Psychosocial Diagnosis and Treatment Before and After Organ Transplantation. Dtsch Arztebl Int. 2023 Jun 16;120(24):413-416. doi: 10.3238/arztebl.m2023.0087. PMID: 37101343; PMCID: PMC10437037.
Pezeshki M, Taherian AA, Gharavy M, Ledger WL. Menstrual characteristics and pregnancy in women after renal transplantation. Int J Gynaecol Obstet 2004;85(2):119–25. http://www.ncbi.nlm.nih.gov/pubmed/15099772.
Bar J, Ben-Rafael Z, Pados A, Orvieto R, Boner G, Hod M. Prediction of pregnancy outcome in subgroups of women with renal disease. Clin Nephrol 2000;53(6):437–44. http://www.ncbi.nlm.nih.gov/pubmed/10879663.
Stratta P, Canavese C, Giacchino F, Mesiano P, Quaglia M, Rossetti M. Pregnancy in kidney transplantation: satisfactory outcomes and harsh realities. J Nephrol 2003;16(6):792-–806. http://www.ncbi.nlm.nih.gov/pubmed/14736006.
Mustafa MS, Noorani A, Abdul Rasool A, Tashrifwala FAA, Jayaram S, Raja S, Jawed F, Siddiq MU, Shivappa SG, Hameed I, Dadana S. Pregnancy outcomes in renal transplant recipients: A systematic review and meta-analysis. Womens Health (Lond). 2024 Jan-Dec;20:17455057241277520. doi: 10.1177/17455057241277520. PMID: 39287599; PMCID: PMC11418342.
Davison JM, Milne JEC. Pregnancy and renal transplantation. Br J Urol 1997;80(Suppl 1):29–32. http://www.ncbi.nlm.nih.gov/pubmed/9240221.
Sgro MD, Barozzino T, Mirghani HM, Sermer M, Moscato L, Akoury H, Koren G, Chitayat DA. Pregnancy outcome post renal transplantation. Teratology 2002;65(1):5–9. http://www.ncbi.nlm.nih.gov/pubmed/11835226.
Ponticelli C, Zaina B, Moroni G. Planned Pregnancy in Kidney Transplantation. A Calculated Risk. J Pers Med. 2021 Sep 26;11(10):956. doi: 10.3390/jpm11100956. PMID: 34683097; PMCID: PMC8537874.
Kainz A, Harabacz I, Cowlrick IS, Gadgil SD, Hagiwara D. Review of the course and outcome of 100 pregnancies in 84 women treated with tacrolimus. Transplantation 2000;70(12):1718–21. http://www.ncbi.nlm.nih.gov/pubmed/11152103.
Jain A, Venkataramanan R, Fung JJ, Gartner JC, Lever J, Balan V, Warty V, Starzl TE. Pregnancy after liver transplantation under tacrolimus. Transplantation 1997;64(4):559–65. http://www.ncbi.nlm.nih.gov/pubmed/9293865.
Sifontis NM, Coscia LA, Costantinescu S, Lavelanet AF, Moritz MJ, Armenti VT. Pregnancy outcomes in solid organ transplant recipients with exposure to micophenolate mofetil or sirolimus. Transplantation 2006;82(12):1698–702. http://www.ncbi.nlm.nih.gov/pubmed/17198262.
Bramham K, Nelson-Piercy C, Gao H. et al. Pregnancy in renal transplant recipients: a UK national cohort study. Clin J Am Soc Nephrol 2013; 8: 290–298 - PMC - PubMed
EBPG Expert Group on Renal Transplantation. European best practice guidelines for renal transplantation. Section IV: Long-term management of the transplant recipient. IV.10. Pregnancy in renal transplant recipients. Nephrol Dial Transplant 2002; 17 (Suppl 4): 50–55 – PubMed
Nankivell, B.J., et al. Diagnosis and prevention of chronic kidney allograft loss. Lancet, 2011. 378: 1428.https://www.ncbi.nlm.nih.gov/pubmed/22000139.
Westall, G.P., et al. Antibody-mediated rejection. Curr Opin Organ Transplant, 2015. 20: 492. https://www.ncbi.nlm.nih.gov/pubmed/26262460.
Jardine, A.G., et al. Prevention of cardiovascular disease in adult recipients of kidney transplants. Lancet, 2011. 378: 1419.https://www.ncbi.nlm.nih.gov/pubmed/22000138.
Liefeldt, L., et al. Risk factors for cardiovascular disease in renal transplant recipients and strategies to minimize risk. Transpl Int, 2010. 23: 1191.https://www.ncbi.nlm.nih.gov/pubmed/21059108.
Boor, P., et al. Renal allograft fibrosis: biology and therapeutic targets. Am J Transplant, 2015. 15: 863. https://www.ncbi.nlm.nih.gov/pubmed/25691290.
Westall, G.P., et al. Antibody-mediated rejection. Curr Opin Organ Transplant, 2015. 20: 492. https://www.ncbi.nlm.nih.gov/pubmed/26262460.
Chapman, J.R. Chronic calcineurin inhibitor nephrotoxicity-lest we forget. Am J Transplant, 2011. 11: 693.https://www.ncbi.nlm.nih.gov/pubmed/21446974.
Higgins, R.M., et al. Antibody-incompatible kidney transplantation in 2015 and beyond. Nephrol Dial Transplant, 2015. 30: 1972.https://www.ncbi.nlm.nih.gov/pubmed/25500804.
Naesens, M. Zero-Time Renal Transplant Biopsies: A Comprehensive Review. Transplantation, 2016. 100: 1425.https://www.ncbi.nlm.nih.gov/pubmed/26599490.
Kasiske, B.L., et al. The role of procurement biopsies in acceptance decisions for kidneys retrieved for transplant. Clin J Am Soc Nephrol, 2014. 9: 562.https://www.ncbi.nlm.nih.gov/pubmed/24558053.
Ujjawal A, Schreiber B, Verma A. Sodium-glucose cotransporter-2 inhibitors (SGLT2i) in kidney transplant recipients: what is the evidence? Ther Adv Endocrinol Metab. 2022 Apr 13;13:20420188221090001. doi: 10.1177/20420188221090001. PMID: 35450095; PMCID: PMC9016587.
Трансплантология. Фармакотерапия без ошибок // руководство для врачей / под ред. С. В. Готье и Я. Г. Мойсюка. — М.: Е-ното, 2014. — 432 с.
Jones-Hughes, T., et al. Immunosuppressive therapy for kidney transplantation in adults: a systematic review and economic model. Health Technol Assess, 2016. 20: 1. https://pubmed.ncbi.nlm.nih.gov/27578428
Leas, B.F., et al., Calcineurin Inhibitors for Renal Transplant. 2016: Rockville (MD): AHRQ. https://www.ncbi.nlm.nih.gov/books/NBK356377
Sawinski, D., et al. Calcineurin Inhibitor Minimization, Conversion, Withdrawal, and Avoidance Strategies in Renal Transplantation: A Systematic Review and Meta-Analysis. Am J Transplant, 2016. 16: 2117.
Knechtle SJ, Marson LP, Morris PJ. Kidney transplantation: principles and practice, 8 Edition, 2020, Elsevier
«Трансплантология. Фармакотерапия без ошибок» руководство для врачей / под ред. С. В. Готье и Я. Г. Мойсюка. — М.: Е-ното, 2014. — 432 с.
Markmann JF, Rickels MR, Eggerman TL, Bridges ND, Lafontant DE, Qidwai J, Foster E, Clarke WR, Kamoun M, Alejandro R, Bellin MD, Chaloner K, Czarniecki CW, Goldstein JS, Hering BJ, Hunsicker LG, Kaufman DB, Korsgren O, Larsen CP, Luo X, Naji A, Oberholzer J, Posselt AM, Ricordi C, Senior PA, Shapiro AMJ, Stock PG, Turgeon NA. Phase 3 trial of human islet-after-kidney transplantation in type 1 diabetes. Am J Transplant. 2021 Apr;21(4):1477-1492. doi: 10.1111/ajt.16174
Catarinella, Davide et al. Long-term outcomes of pancreatic islet transplantation alone in type 1 diabetes: a 20-year single-centre study in Italy. The Lancet Diabetes & Endocrinology, Volume 13, Issue 4, 279 – 293
Maanaoui, Mehdi Armanet, Mathieu et al.Islet-after-kidney transplantation versus kidney alone in kidney transplant recipients with type 1 diabetes (KAIAK): a population-based target trial emulation in France. The Lancet Diabetes & Endocrinology, Volume 12, Issue 10, 716 - 724.
Lindahl JP, Reinholt FP, Eide IA, Hartmann A, Midtvedt K, Holdaas H, Dorg LT, Reine TM, Kolset SO, Horneland R, Øyen O, Brabrand K, Jenssen T. In patients with type 1 diabetes simultaneous pancreas and kidney transplantation preserves long-term kidney graft ultrastructure and function better than transplantation of kidney alone. Diabetologia. 2014 Nov;57(11):2357-65. doi: 10.1007/s00125-014-3353-2.
Lehmann R, et al. Glycemic Control in Simultaneous Islet-Kidney Versus Pancreas-Kidney Transplantation in Type 1 Diabetes: A Prospective 13-Year Follow-up. Diabetes care. 2015;38:752–759. doi: 10.2337/dc14-1686
Kempf MC, et al. Logistics and transplant coordination activity in the GRAGIL Swiss-French multicenter network of islet transplantation. Transplantation. 2005;79:1200–5. doi: 10.1097/01.tp.0000161224.67535.41
Hillberg AL, et al. Improving alginate-poly-L-ornithine-alginate capsule biocompatibility through genipin crosslinking. J Biomed Mater Res B Appl Biomater. 2013;101:258–68. doi: 10.1002/jbm.b.32835.
Hering B, et al. Phase 3 Trial of Transplantation of Human Islets in Type 1 Diabetes Mellitus Complicatedby Severe Hypoglycemia. Diabetes Care. 2016 doi: 10.2337/dc15-1988. in Press. The results of this single arm Phase 3 Trial will be instrumental in obtaining licensure for a human islet product from the FDA which is required to fund future clinical allogeneic islet transplant procedures.
Bartlett ST, et al. Report from IPITA-TTS Opinion Leaders Meeting on the Future of beta-Cell Replacement. Transplantation. 2016;100(Suppl 2):S1–S44. doi: 10.1097/TP.0000000000001055.
O'Connell PJ, et al. Multicenter Australian trial of islet transplantation: improving accessibility and outcomes. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2013;13:1850–1858. doi: 10.1111/ajt.12250.
https://cr.minzdrav.gov.ru/preview-cr/469_3 Хроническая болезнь почек, взрослые
Altemose KE, Nailescu C. Management of pediatric obesity as a pathway towards kidney transplantation. Front Pediatr. 2024 Feb 15;12:1367520. doi: 10.3389/fped.2024.1367520.
Mahalati K, Belitsky P, Sketris I, West K, Panek R. Neoral monitoring by simplified sparse sampling area under the concentration‐time curve: its relationship to acute rejection and cyclosporine nephrotoxicity early after kidney transplantation. Transplantation. 1999;68(1):55‐62. doi: 10.1097/00007890-199907150-00011
Gaynor JJ, Ciancio G, Guerra G, Sageshima J, Roth D, Goldstein MJ, Chen L, Kupin W, Mattiazzi A, Tueros L, Flores S, Hanson L, Ruiz P, Vianna R, Burke GW 3rd. Lower tacrolimus trough levels are associated with subsequently higher acute rejection risk during the first 12 months after kidney transplantation. Transpl Int. 2016 Feb;29(2):216-26. doi: 10.1111/tri.12699. Epub 2015 Nov 3. PMID: 26442829.
Wallemacq P, Goffinet JS, O’Morchoe S et al. Multi-site analytical evaluation of the Abbott ARCHITECT tacrolimus assay. Ther Drug Monit 2009; 31: 198–204.
Jorgensen K, Povlsen J, Madsen S et al. C2 (2-h) levels are not superior to trough levels as estimates of the area under the curve in tacrolimus-treated renal-transplant patients. Nephrol Dial Transplant 2002; 17: 1487–1490.
Kasiske BL, Andany MA, Danielson B. A thirty percent chronic decline in inverse serum creatinine is an excellent predictor of late renal allograft failure. Am J Kidney Dis 2002; 39: 762–768
Kasiske BL, Andany MA, Hernandez D et al. Comparing methods for monitoring serum creatinine to predict late renal allograft failure. Am J Kidney Dis 2001; 38: 1065–1073.
Loupy A, Bouquegneau A, Stegall MD, Montgomery RA. Clinical outcomes after ABO-incompatible renal transplantation. Lancet (2019) 394(10213):1988-9. doi:10.1016/S0140-6736(19)32490-0
Kanter Berga J, Sancho Calabuig A, Gavela Martinez E, Puig Alcaraz N, Avila Bernabeu A, Crespo Albiach J, Molina Vila P, Beltrán Catalan S, Pallardó Mateu L. Desensitization Protocol in Recipients of Deceased Kidney Donor With Donor-Specific Antibody-Low Titers. Transplant Proc. 2016 Nov;48(9):2880-2883. doi: 10.1016/j.transproceed.2016.07.050.
Green H, Nesher E, Aizner S, Israeli M, Klein T, Zakai H, Rahamimov R, Rozen-Zvi B, Mor E. Long-term results of desensitization protocol with and without rituximab in sensitized kidney transplant recipients. Clin Transplant. 2019 Jun;33(6):e13562. doi: 10.1111/ctr.13562.
Mutze, S., Türk, I., Schönberger, B. et al. Colour-coded duplex sonography in the diagnostic assessment of vascular complications after kidney transplantation in children. Pediatric Radiology 27, 898–902 (1997). https://doi.org/10.1007/s00247005026
Nixon JN, Biyyam DR, Stanescu L, Phillips GS, Finn LS, Parisi MT. Imaging of pediatric renal transplants and their complications: a pictorial review. Radiographics. 2013 Sep-Oct;33(5):1227-51. doi: 10.1148/rg.335125150.
Castagnetti M, Angelini L, Ghirardo G, Zucchetta P, Gamba P, Zanon G, Murer L, Rigamonti W. Ureteral complications after renal transplant in children: timing of presentation, and their open and endoscopic management. Pediatr Transplant. 2014 Mar;18(2):150-4. doi: 10.1111/petr.12207
Balani SS, Jensen CJ, Kouri AM, Kizilbash SJ. Induction and maintenance immunosuppression in pediatric kidney transplantation-Advances and controversies. Pediatr Transplant. 2021 Nov;25(7):e14077. doi: 10.1111/petr.14077. ]
Prytula A, van Gelder T. Clinical aspects of tacrolimus use in paediatric renal transplant recipients. Pediatric nephrology (Berlin, Germany). 2019; 34: 31-43.
Weber LT, Shipkova M, Lamersdorf T, et al. Pharmacokinetics of mycophenolic acid (MPA) and determinants of MPA free fraction in pediatric and adult renal transplant recipients. German Study Group on Mycophenolate Mofetil Therapy in Pediatric Renal Transplant Recipients. J Am Soc Nephrol 1998; 9: 1511
Ettenger, Robert1,3; Sarwal, Minnie M.2. Mycophenolate Mofetil in Pediatric Renal Transplantation. Transplantation 80(2S):p S201-S210, October 15, 2005. | DOI: 10.1097/01.tp.0000186957.32801.c0
Gonwa T, Mendez R, Yang HC, Weinstein S, Jensik S, Steinberg S; Prograf Study Group. Randomized trial of tacrolimus in combination with sirolimus or mycophenolate mofetil in kidney transplantation: results at 6 months. Transplantation. 2003 Apr 27;75(8):1213-20. doi: 10.1097/01.TP.0000062837.99400.60.
Campbell SB, Walker R, Tai SS, Jiang Q, Russ GR. Randomized controlled trial of sirolimus for renal transplant recipients at high risk for nonmelanoma skin cancer. Am J Transplant. 2012 May;12(5):1146-56. doi: 10.1111/j.1600-6143.2012.04004.x.
Nashan B, Curtis J, Ponticelli C, Mourad G, Jaffe J, Haas T; 156 Study Group. Everolimus and reduced-exposure cyclosporine in de novo renal-transplant recipients: a three-year phase II, randomized, multicenter, open-label study. Transplantation. 2004 Nov 15;78(9):1332-40. doi: 10.1097/01.tp.0000140486.97461.49
Pascual J. Concentration-controlled everolimus (Certican): combination with reduced dose calcineurin inhibitors. Transplantation. 2005 May 15;79(9 Suppl):S76-9. doi: 10.1097/01.tp.0000162434.62591.f3. PMID: 15880020.
Hoyer PF, Ettenger R, Kovarik JM, et al. Everolimus** in pediatric de nova renal transplant patients. Transplantation. 2003;75:2082-2085.
Lablanche S, Vantyghem MC, Kessler L, Wojtusciszyn A, Borot S, Thivolet C, Girerd S, Bosco D, Bosson JL, Colin C, Tetaz R, Logerot S, Kerr-Conte J, Renard E, Penfornis A, Morelon E, Buron F, Skaare K, Grguric G, Camillo-Brault C, Egelhofer H, Benomar K, Badet L, Berney T, Pattou F, Benhamou PY; TRIMECO trial investigators. Islet transplantation versus insulin therapy in patients with type 1 diabetes with severe hypoglycaemia or poorly controlled glycaemia after kidney transplantation (TRIMECO): a multicentre, randomised controlled trial. Lancet Diabetes Endocrinol. 2018 Jul;6(7):527-537. doi: 10.1016/S2213-8587(18)30078-0.
Vantyghem MC, Chetboun M, Gmyr V, Jannin A, Espiard S, Le Mapihan K, Raverdy V, Delalleau N, Machuron F, Hubert T, Frimat M, Van Belle E, Hazzan M, Pigny P, Noel C, Caiazzo R, Kerr-Conte J, Pattou F; Members of the Spanish Back Pain Research Network Task Force for the Improvement of Inter-Disciplinary Management of Spinal Metastasis. Ten-Year Outcome of Islet Alone or Islet After Kidney Transplantation in Type 1 Diabetes: A Prospective Parallel-Arm Cohort Study. Diabetes Care. 2019 Nov;42(11):2042-2049. doi: 10.2337/dc19-0401. Erratum in: Diabetes Care. 2020 May;43(5):1164. doi: 10.2337/dc20-er05.
Lefaucheur C, Nochy D, Andrade J, et al. Comparison of combination plasmapheresis/IVIG/anti-CD20 versus high-dose IVIG in the treatment of antibody-mediated rejection. Am J Transplant 200991099–1107.
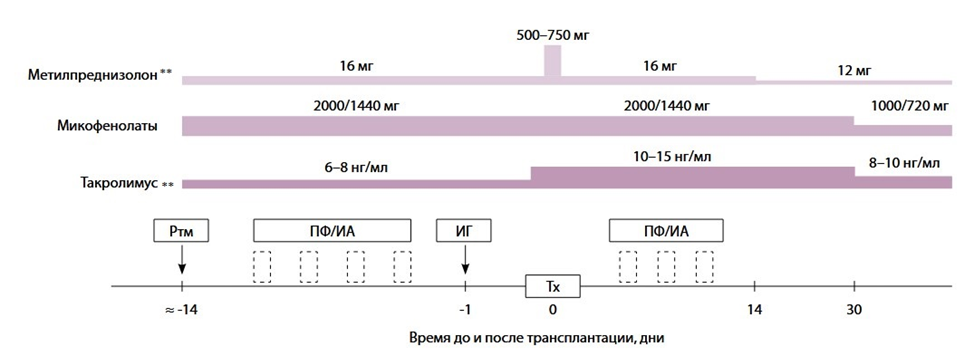 Схема 1. Персонализированный протокол ведения пациентов, которым планируется выполнение трансплантации почки от живого донора, несовместимого по групппе крови [152]
Схема 1. Персонализированный протокол ведения пациентов, которым планируется выполнение трансплантации почки от живого донора, несовместимого по групппе крови [152]
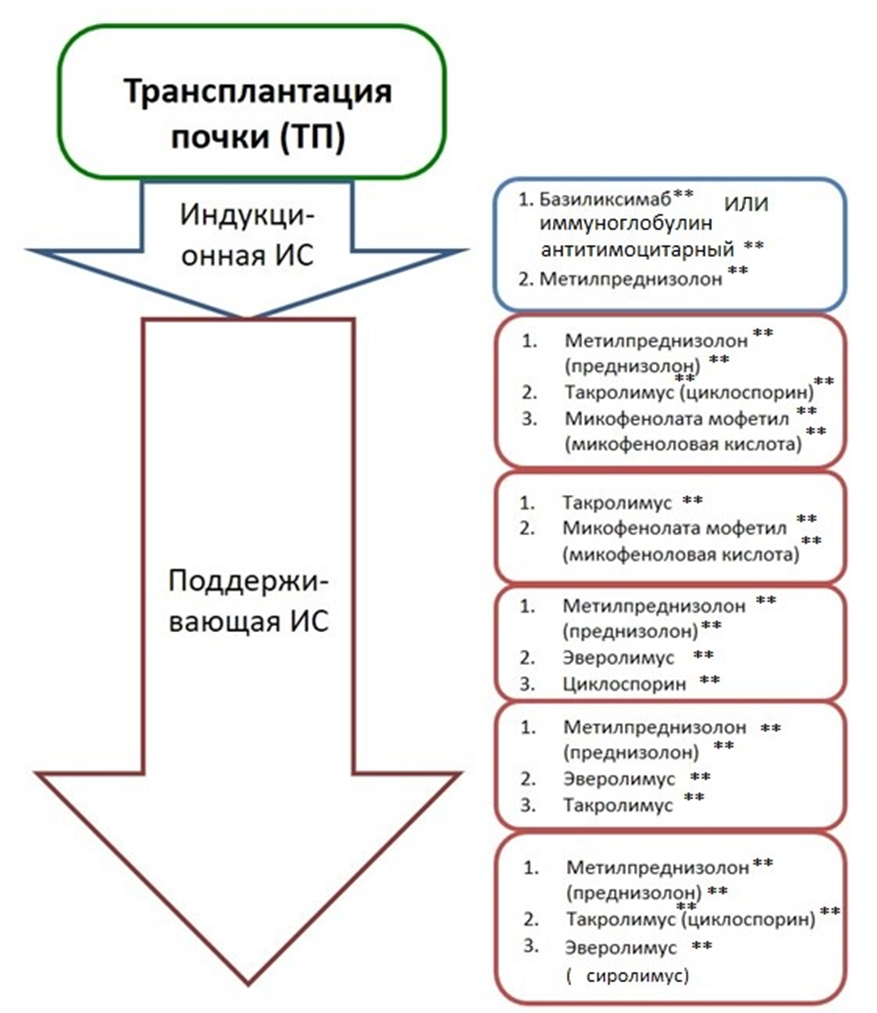 Схема 3. Различные виды иммуносупрессивной терапии. Адаптирована из «Трансплантология. Фармакотерапия без ошибок» руководство для врачей / под ред. С. В. Готье и Я. Г. Мойсюка. – М.: «Е-ното», 2014. – 432 с. [311]
Схема 3. Различные виды иммуносупрессивной терапии. Адаптирована из «Трансплантология. Фармакотерапия без ошибок» руководство для врачей / под ред. С. В. Готье и Я. Г. Мойсюка. – М.: «Е-ното», 2014. – 432 с. [311]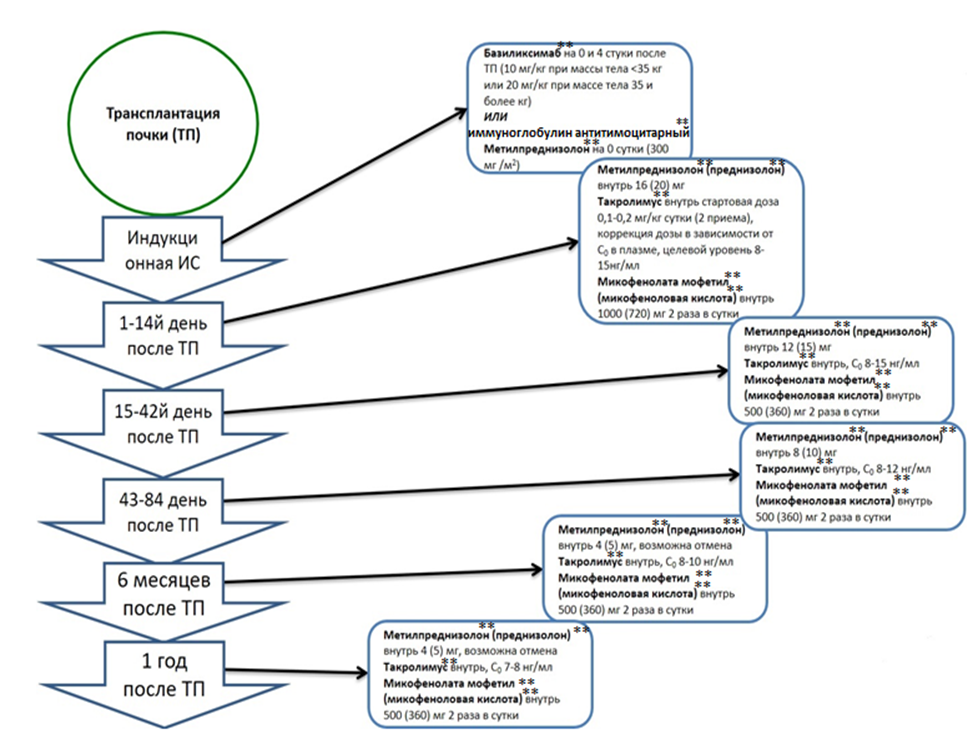 Схема 4. Схема иммуносупрессивной терапии после трансплантации почки. Адаптирована из «Трансплантология. Фармакотерапия без ошибок» руководство для врачей / под ред. С. В. Готье и Я. Г. Мойсюка.– М.: «Е-ното» , 2014. – 432 с. [311]
Схема 4. Схема иммуносупрессивной терапии после трансплантации почки. Адаптирована из «Трансплантология. Фармакотерапия без ошибок» руководство для врачей / под ред. С. В. Готье и Я. Г. Мойсюка.– М.: «Е-ното» , 2014. – 432 с. [311]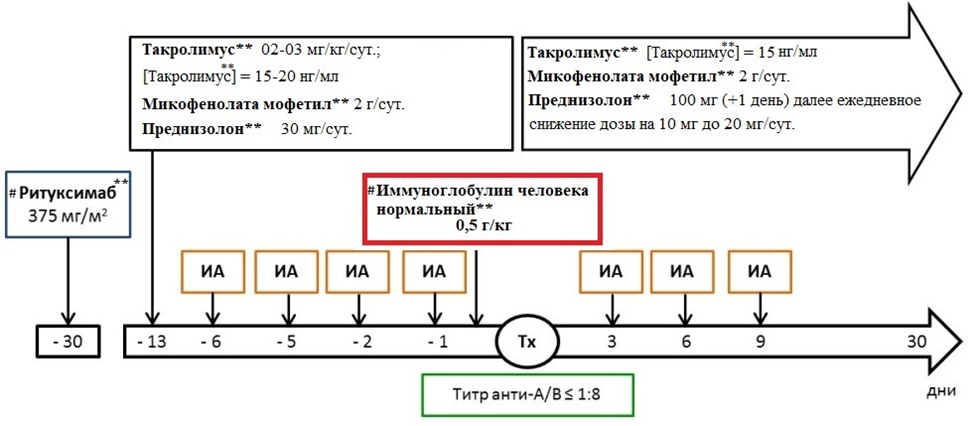 Схема 5. «Стокгольмский» протокол проведения AB0-несовместимой трансплантации почки от живого родственного донора. ИА – специфическая иммуноадсорбция; Tx – трансплантация почки [152].
Схема 5. «Стокгольмский» протокол проведения AB0-несовместимой трансплантации почки от живого родственного донора. ИА – специфическая иммуноадсорбция; Tx – трансплантация почки [152].