Sackett DL., Rosenberg WM., Gray JA., Haynes RB., Richardson WS. Evidence based medicine: what it is and what it isn't. BMJ 1996; 312(7023): 71-2. Doi: 10.1136/bmj.312.7023.71.
Федеральный закон от 21.11.2011 № 323-ФЗ (ред. от 03.04.2017) «Об основах охраны здоровья граждан в Российской Федерации».
Эпидемиологический словарь, 4-е издание. Под ред. Джона М. Ласта для Международной эпидемиологической ассоциации. М., 2009. 316 с..
Федеральное агентство по техническому регулированию и метрологии. Национальный стандарт Российской Федерации. ГОСТР 52379-2005. Надлежащая клиническая практика. Москва, 2005.
Al-Khatib SM., Stevenson WG., Ackerman MJ., Bryant WJ., Callans DJ., Curtis AB., Deal BJ., Dickfeld T., Field ME., Fonarow GC., et al. 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation 2018; 138(13): e272-e391. Doi: 10.1161/CIR.0000000000000549.
Elliot P., Zamorano JL., Anastasakis A., Borger MA., Borggrefe M., Cecchi F., Charron P., Hagege AA., Lafont A., Limongelli G., et al. 2014 ESC guidelines on diagnosis and management of hypertrophic cardiomyopathy: The task force for the diagnosis and management of hypertrophic cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J 2014; 35(39): 2733–79. Doi: 10.1093/eurheartj/ehu284.
Андреева Н.С., Реброва О.Ю., Зорин Н.А., Авксентьева М.В., Омельяновский В.В. Системы оценки достоверности научных доказательств и убедительности рекомендаций: сравнительная характеристика и перспективы унификации. Медицинские технологии. Оценка и выбор 2012; 4: 10-24.
Zeppenfeld K., Tfelt-Hansen J., de Riva M., Winkel BG., Behr ER., Blom NA., Charron P., Corrado D., Dagres N., de Chillou C., et al. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J 2022; 43(40): 3997-4126. Doi: 10.1093/eurheartj/ehac262.
Рыжкова О.П., Кардымон О.Л., Прохорчук Е.Б., Коновалов Ф.А., Масленников А.Б., Степанов В.А., Афанасьев А.А., Заклязьминская Е.В., Ребриков Д.В., Савостьянов К.В. и др. Руководство по интерпретации данных последовательности ДНК человека, полученных методами массового параллельного секвенирования (MPS) (редакция 2018, версия 2). Медицинская генетика 2019; 18(2): 3-23.
Ревишвили А.Ш., Шляхто Е.В., Попов С.В. и др. Российские клинические рекомендации по проведению электрофизиологических исследований, катетерной абляции и применению имплантируемых антиаритмических устройств. — Москва: ВНОА, 2017. — 701 с.
Myerburg RJ., Junttila MJ. Sudden cardiac death caused by coronary heart disease. Circulation 2012; 125(8): 1043-52. Doi: 10.1161/CIRCULATIONAHA.111.023846.
Stecker EC., Reinier K., Marijon E., Narayanan K., Teodorescu C., Uy-Evanado A., Gunson K, Jui J., Chugh SS. Public health burden of sudden cardiac death in the United States. Circ Arrhythm Electrophysiol 2014; 7(2): 212-17.
Chen LY., Sotoodehnia N., Bůžková P., Lopez FL., Yee LM., Heckbert SR., Prineas R., Soliman EZ., Adabag S., Konety S., et al. Atrial fibrillation and the risk of sudden cardiac death: the atherosclerosis risk in communities study and cardiovascular health study. JAMA Intern Med 2013; 173(1): 29-35. Doi: 10.1001/2013.jamainternmed.744.
Marijon E., Uy-Evanado A., Dumas F., Karam N., Reinier K., Teodorescu C., Narayanan K., Gunson K., Jui J., Jouven X., Chugh SS. Warning Symptoms Are Associated With Survival From Sudden Cardiac Arrest. Ann Intern Med 2016; 164(1): 23-9. Doi: 10.7326/M14-2342.
Glinge C., Jabbari R., Risgaard B., Lynge TH., Engstrøm T., Albert CM., Haunsø S., Winkel BG., Tfelt-Hansen J. Symptoms Before Sudden Arrhythmic Death Syndrome: A Nationwide Study Among the Young in Denmark. J Cardiovasc Electrophysiol 2015; 26(7): 761-67. Doi: 10.1111/jce.12674. .
Ågesen FN., Lynge TH., Blanche P., Banner J., Prescott E., Jabbari R., Tfelt-Hansen J. Temporal trends and sex differences in sudden cardiac death in the Copenhagen City Heart Study. Heart 2021; 107(16): 1303-1309. Doi: 10.1136/heartjnl-2020-318881.
Eckart RE., Shry EA., Burke AP., McNear JA., Appel DA., Castillo-Rojas LM., Avedissian L., Pearse LA., Potter RN., Tremaine L., et al. Sudden death in young adults: an autopsy-based series of a population undergoing active surveillance. J Am Coll Cardiol 2011; 58(12): 1254-61. Doi: 10.1016/j.jacc.2011.01.049.
Van der Werf C., Hendrix A., Birnie E., Bots ML., Vink A., Bardai A., Blom MT., Bosch J., Bruins W., Das CK., et al. Improving usual care after sudden death in the young with focus on inherited cardiac diseases (the CAREFUL study): a community-based intervention study. Europace 2016; 18(4): 592-601. Doi: 10.1093/europace/euv059.
United Nations Economic Commission for Europe. UNECE statistical database.
Л. М. Макаров, В. Н. Комолатова, И. И. Киселева. Распространенность внезапной сердечной смерти у лиц молодого возраста в крупном мегаполисе. Медицинский алфавит 2014. 3: 35–40.
Бокерия Л. А., Неминущий Н. М., Постол А. С. Сердечная ресинхронизирующая терапия. Формирование показаний и современных подходов к методу повышения эффективности. Комплексные проблемы сердечно-сосудистых заболеваний 2018; 7 (3): 102-116. Doi: 10.17802/2306-1278-2018-7-3-102-116
Fishman GI., Chugh SS., Dimarco JP., Albert CM., Anderson ME., Bonow RO., Buxton AE., Chen PS., Estes M., Jouven X., et al. Sudden cardiac death prediction and prevention: report from a National Heart, Lung, and Blood Institute and Heart Rhythm Society Workshop. Circulation 2010; 122(22): 2335-48. Doi: 10.1161/CIRCULATIONAHA.110.976092.
Wong CX., Brown A., Lau DH., Chugh SS., Albert CM., Kalman JM., Sanders P. Epidemiology of Sudden Cardiac Death: Global and Regional Perspectives. Heart Lung Circ 2019; 28(1): 6-14. Doi: 10.1016/j.hlc.2018.08.026.
Bougouin W., Lamhaut L., Marijon E., Jost D., Dumas F., Deye N., Beganton F., Empana JP., Chazelle E., Cariou A., et al. SDEC Co-Investigators. Characteristics and prognosis of sudden cardiac death in Greater Paris: population-based approach from the Paris Sudden Death Expertise Center (Paris-SDEC). Intensive Care Med 2014. 40(6): 846-54. Doi: 10.1007/s00134-014-3252-5.
Deo R., Albert CM. Epidemiology and genetics of sudden cardiac death. Circulation 2012; 125(4): 620-37. Doi: 10.1161/CIRCULATIONAHA.111.023838.
Gerber Y., Jacobsen SJ., Frye RL., Weston SA., Killian JM., Roger VL. Secular trends in deaths from cardiovascular diseases: a 25-year community study. Circulation 2006; 113(19): 2285-92. Doi: 10.1161/CIRCULATIONAHA.105.590463.
Krahn AD., Connolly SJ., Roberts RS., Gent M. ATMA Investigators. Diminishing proportional risk of sudden death with advancing age: implications for prevention of sudden death. Am Heart J 2004; 147(5): 837-40. Doi: 10.1016/j.ahj.2003.12.017.
Becker LB., Han BH., Meyer PM., Wright FA., Rhodes KV., Smith DW., Barrett J. Racial differences in the incidence of cardiac arrest and subsequent survival. The CPR Chicago Project. N Engl J Med 1993; 329(9): 600-6. Doi: 10.1056/NEJM199308263290902.
Zhao D., Post WS., Blasco-Colmenares E., Cheng A., Zhang Y., Deo R., Pastor-Barriuso R., Michos ED., Sotoodehnia N., Guallar E. Racial Differences in Sudden Cardiac Death. Circulation 2019; 139(14): 1688-1697. Doi: 10.1161/CIRCULATIONAHA.118.036553. Erratum in: Circulation 2019; 139(14): e837. Doi: 10.1161/CIR.0000000000000672.
Fox CS., Evans JC., Larson MG., Kannel WB., Levy D. Temporal trends in coronary heart disease mortality and sudden cardiac death from 1950 to 1999: the Framingham Heart Study. Circulation 2004; 110(5): 522-7. Doi: 10.1161/01.CIR.0000136993.34344.41.
Zheng ZJ., Croft JB., Giles WH., Mensah GA. Sudden cardiac death in the United States, 1989 to 1998. Circulation 2001; 104(18): 2158-63. Doi: 10.1161/hc4301.098254.
Dudas K., Lappas G., Stewart S., Rosengren A. Trends in out-of-hospital deaths due to coronary heart disease in Sweden (1991 to 2006). Circulation 2011; 123(1): 46-52. Doi: 10.1161/CIRCULATIONAHA.110.964999.
Heidbuchel H., Willems R., Jordaens L., Olshansky B., Carre F., Lozano IF., Wilhelm M., Müssigbrodt A., Huybrechts W., Morgan J., et al. Intensive recreational athletes in the prospective multinational ICD Sports Safety Registry: Results from the European cohort. Eur J Prev Cardiol 2019; 26(7): 764-775. Doi: 10.1177/2047487319834852.
Risgaard B., Winkel BG., Jabbari R., Glinge C., Ingemann-Hansen O., Thomsen JL., Ottesen GL., Haunsø S., Holst AG., Tfelt-Hansen J. Sports-related sudden cardiac death in a competitive and a noncompetitive athlete population aged 12 to 49 years: data from an unselected nationwide study in Denmark. Heart Rhythm 2014; 11(10): 1673-81. Doi: 10.1016/j.hrthm.2014.05.026.
Byrne R., Constant O., Smyth Y., et al. Multiple source surveillance incidence and aetiology of out-of-hospital sudden cardiac death in a rural population in the West of Ireland. European Heart Journal 2008; 29(11): 1418-1423. Doi: 10.1093/eurheartj/ehn155. Epub 2008 Apr 17.
Waldmann V., Karam N., Bougouin W., et al. Burden of coronary artery disease as a cause of sudden cardiac arrest in the young. Journal of the American College of Cardiology 2019; 73(16): 2118-2120. Doi: 10.1016/j.jacc.2019.01.064.
Waldmann V., Karam N., Rischard J., et al. Low rates of immediate coronary angiography among young adults resuscitated from sudden cardiac arrest. Resuscitation 2020; 147: 34-42. Doi: 10.1016/j.resuscitation.2019.12.005.
Бойцов С.А., Погосова Н.В., Бубнова М.Г. и др. Кардиоваскулярная профилактика 2017. Российские национальные рекомендации. Российский кардиологический журнал 2018; 7–122. https://doi.org/10.15829/1560-4071-2018-6-7-122.
Jouven X., Desnos M., Guerot C., Ducimetière P. Predicting sudden death in the population: the Paris Prospective Study I. Circulation 1999; 99(15): 1978-1983. Doi: 10.1161/01.cir.99.15.1978.
Dekker LRC., Bezzina CR., Henriques JPS., et al. Familial sudden death is an important risk factor for primary ventricular fibrillation: a case-control study in acute myocardial infarction patients. Circulation 2006; 114(11): 1140-1145. Doi: 10.1161/CIRCULATIONAHA.105.606145.
Deo R., Norby FL., Katz R., et al. Development and validation of a sudden cardiac death prediction model for the general population. Circulation 2016; 134(11): 806-816. Doi: 10.1161/CIRCULATIONAHA.116.023042.
Yoshinaga M., Ushinohama H., Sato S., et al. Etectrocardiographic screening of 1-month-old infants for identifying prolonged QT intervals. Circulation: Arrhythmia and Electrophysiology 2013; 6(5): 932-938. Doi: 10.1161/CIRCEP.113.000619.
Boas R., Sappler N., von Stülpnagel L., et al Periodic repolarization dynamics identifies ICD-responders in non-ischemic cardiomyopathy: a DANISH substudy. Circulation 2022; 145(10): 754-764. Doi: 10.1161/CIRCULATIONAHA.121.056464.
Spirito P., Bellone P., Harris K.M., et al. Magnitude of left ventricular hypertrophy and risk of sudden death in hypertrophic cardiomyopathy. The New England Journal of Medicine 2000; 342(24): 1778-1785. Doi: 10.1056/NEJM200006153422403.
Barsheshet A., Goldenberg I., O-Uchi J., et al. Mutations in cytoplasmic loops of the KCNQ1 channel and the risk of life-threatening events: implications for mutation-specific response to β-blocker therapy in type 1 long-QT syndrome. Circulation 2012;125(16): 1988-1996. Doi: 10.1161/CIRCULATIONAHA.111.048041.
Wahbi K., Ben Yaou R., Gandjbakhch E., et al. Development and validation of a new risk prediction score for life-threatening ventricular tachyarrhythmias in laminopathies / // Circulation. 2019; 140(4): 293-302. Doi: 10.1161/CIRCULATIONAHA.118.039410.
Cadrin-Tourigny J., Bosman L.P., Nozza A., et al. A new prediction model for ventricular arrhythmias in arrhythmogenic right ventricular cardiomyopathy. European Heart Journal 2019; 40(23): 1850-1858. Doi: 10.1093/eurheartj/ehz103.
Steyerberg E.W., Vergouwe Y. Steyerberg E.W. Towards better clinical prediction models: seven steps for development and an ABCD for validation. European Heart Journal 2014; 35(29): 1925-1931. Doi: 10.1093/eurheartj/ehu207.
Collins G.S., Reitsma J.B., Altman D.G., et al. TRIPOD Group. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. Circulation 2015; 350: g7594. Doi: 10.1136/bmj.g7594.
Zipes D.P., Camm A.J., Borggrefe M., et al. ACC/AHA/ЕОК 2006 Guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Circulation 2006; 114(10): e385-484. Doi: 10.1161/CIRCULATIONAHA.106.178233.
Priori SG., Blomström-Lundqvist C., Mazzanti A., Blom N., Borggrefe M., Camm J., Elliott PM., Fitzsimons D., Hatala R., Hindricks G., et al. 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J 2015; 36(41): 2793-2867. Doi: 10.1093/eurheartj/ehv316.
Keren A, Tzivoni D., Gavish D., Levi J., Gottlieb S., Benhorin J., Stern S. Etiology, warning signs and therapy of torsade de pointes. A study of 10 patients. Circulation 1981; 64(6): 1167-74. Doi: 10.1161/01.cir.64.6.1167.
Bhandari AK., Shapiro WA., Morady F., Shen EN., Mason J., Scheinman MM. Electrophysiologic testing in patients with the long QT syndrome. Circulation 1985; 71(1): 63-71. Doi: 10.1161/01.cir.71.1.63.
Piepoli MF., Hoes AW., Agewall S., Albus C., Brotons C., Catapano AL., Cooney MT., Corrà U., Cosyns B., Deaton C., et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 2016; 37(29): 2315-81. Doi: 10.1093/eurheartj/ehw106.
Casella M., Carbucicchio C., Russo E., Pizzamiglio F., Golia P., Conti S., Costa F., Dello Russo A., Tondo C. Electrical storm in systemic sclerosis: Inside the electroanatomic substrate. World J Cardiol 2014; 6(10): 1127-30. Doi: 10.4330/wjc.v6.i10.1127.
Apshtein A.E., Ideker R.E. Ventricular Fibrillation in “Cardiac Electrophysiology. From Cell to Bedside”. Saunders Company 2000: 677-684.
Epstein AE., Dimarco JP., Ellenbogen KA., Estes NA 3rd., Freedman RA., Gettes LS., Gillinov AM., Gregoratos G., Hammill SC., Hayes DL., Hlatky MA., et al. ACC/AHA/HRS 2008 Guidelines for device-based therapy of cardiac rhythm abnormalities. Heart Rhythm 2008; 5(6): 1-62. Doi: 10.1016/j.hrthm.2008.04.014.
Avanzas P., Arroyo-Espliguero R., Cosín-Sales J., Quiles J., Zouridakis E., Kaski JC. Multiple complex stenoses, high neutrophil count and C-reactive protein levels in patients with chronic stable angina. Atherosclerosis; 175(1): 151-57. Doi: 10.1016/j.atherosclerosis.2004.03.013.
Núñez J., Miñana G., Bodí V., Núñez E., Sanchis J., Husser O., Llàcer A. Low lymphocyte count and cardiovascular diseases. Curr Med Chem 2011; 18(21): 3226-33. Doi: 10.2174/092986711796391633.
Suh S., Cho YR., Park MK., Kim DK., Cho NH., Lee MK. Relationship between serum bilirubin levels and cardiovascular disease. PLoS One 2018; 13(2). Doi: 10.1371/journal.pone.0193041. eCollection 2018.
Alexander CM., Landsman PB., Teutsch SM. Diabetes mellitus, impaired fasting glucose, atherosclerotic risk factors, and prevalence of coronary heart disease. Am J Cardiol 2000; 86(9): 897-902. Doi: 10.1016/s0002-9149(00)01118-8.
Pilarczyk K., Carstens H., Heckmann J., Canbay A., Koch A., Pizanis N., Jakob H., Kamler M. The aspartate transaminase/alanine transaminase (DeRitis) ratio predicts mid-term mortality and renal and respiratory dysfunction after left ventricular assist device implantation. Eur J Cardiothorac Surg 2017; 52(4): 781-88. Doi: 10.1093/ejcts/ezx247.
Narita K., Ureshino H., Hashimoto S. Sustained ventricular tachycardia caused by subacute thyroiditis. Intern Med J 2018; 48(9): 1160-62. Doi: 10.1111/imj.14018.
Tsai IH., Su YJ. Thyrotoxic periodic paralysis with ventricular tachycardia. Electrocardiol 2019; 54: 93-5. Doi: 10.1016/j.jelectrocard.2019.04.001
Лебедев Д.С., Васичкина Е.С., Татарский Р.Б. Желудочковые тахиаритмии у детей . Р.Б. – СПб.: 2018. – 120 с.
Cheitlin MD., Armstrong WF., Aurigemma GP., Beller GA., Bierman FZ., Davis JL., Douglas PS., Faxon DP., Gillam LD., Kimball TR., et al. ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography – summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). Circulation 2003; 108(9): 1146-62. Doi: 10.1161/01.CIR.0000073597.57414.A9.
Podrid PJ., Graboys TB.. Exercise stress testing in the management of cardiac rhythm disorders. Med Clin North Am 1984; 68(5): 1139-52. Doi: 10.1016/s0025-7125(16)31089-6.
Prastaro M., D'Amore C., Paolillo S., Losi M., Marciano C., Perrino C., Ruggiero D., Gargiulo P., Savarese G., Trimarco B., et al. Prognostic role of transthoracic echocardiography in patients affected by heart failure and reduced ejection fraction. Heart Fail Rev 2015; 20(3): 305-16. Doi: 10.1007/s10741-014-9461-8.
Zellweger MJ., Hachamovitch R., Kang X., Hayes SW., Friedman JD., Germano G., Berman DS. Threshold, incidence, and predictors of prognostically high-risk silent ischemia in asymptomatic patients without prior diagnosis of coronary artery disease. J Nucl Cardiol 2009; 16(2): 193-200. Doi: 10.1007/s12350-008-9016-2.
Volosin K., Stadler RW., Wyszynski R., Kirchhof P. Tachycardia detection performance of implantable loop recorders: results from a large 'real-life' patient cohort and patients with induced ventricular arrhythmias. Europace 2013; 15(8): 1215-22. Doi: 10.1093/europace/eut036.
de Asmundis C., Conte G., Sieira J., Chierchia GB., Rodriguez-Manero M., Di Giovanni G., Ciconte G., Levinstein M., Baltogiannis G., Saitoh Y., et al. Comparison of the patient-activated event recording system vs. traditional 24 h Holter electrocardiography in individuals with paroxysmal palpitations or dizziness. Europace 2014; 16(8): 1231-5. Doi: 10.1093/europace/eut411.
Kang X., Berman DS., Lewin H., Miranda R., Erel J., Friedman JD., Amanullah AM. Comparative ability of myocardial perfusion single-photon emission computed tomography to detect coronary artery disease in patients with and without diabetes mellitus. Am Heart J 1999; 137(5): 949-57. Doi: 10.1016/s0002-8703(99)70421-7.
Zeliaś A., Stępińska J., Andres J., Trąbka-Zawicki A., Sadowski J., Żmudka K. Ten-year experience of an invasive cardiology centre with out-of-hospital cardiac arrest patients admitted for urgent coronary angiography. Kardiol Pol 2014; 72(8): 687-99. Doi: 10.5603/KP. a2014.0088.
Zaman S., Narayan A., Thiagalingam A., Sivagangabalan G., Thomas S., Ross DL., Kovoor P. Significance of repeat programmed ventricular stimulation at electrophysiology study for arrhythmia prediction after acute myocardial infarction. Pacing Clin Electrophysiol 2014; 37(7): 795-802. Doi: 10.1111/pace.12391.
Denes P., Uretz E., Ezri MD., Borbola J. Clinical predictors of electrophysiologic findings in patients with syncope of unknown origin. Arch Intern Med 1988; 148(9): 1922-8.
Speranzon A., Chicco D., Bonazza P., D'Alfonso R., Bobbo M., D'Agata Mottolese B., Barbi E., Caiffa T. Brugada Syndrome: Focus for the General Pediatrician. Children (Basel) 2024; 11(3): 281. Doi: 10.3390/children11030281.
Brignole M., Menozzi C., Moya A., Garcia-Civera R., Mont L., Alvarez M., Errazquin F., Beiras J., Bottoni N., Donateo P. International Study on Syncope of Uncertain Etiology (ISSUE) Investigators. Mechanism of syncope in patients with bundle branch block and negative electrophysiological test. Circulation 2001; 104(17): 2045-50. Doi: 10.1161/hc4201.097837.
Yuhas J., Mattocks K., Gravelin L., Remetz M., Foley J., Fazio R., Lampert R. Patients' attitudes and perceptions of implantable cardioverter-defibrillators: potential barriers to appropriate primary prophylaxis. Pacing Clin Electrophysiol 2012; 35(10): 1179-87. Doi: 10.1111/j.1540-8159.2012.03497.x.
St John Sutton M., Pfeffer MA., Plappert T., Rouleau JL., Moyé LA., Dagenais GR., Lamas GA., Klein M., Sussex B., Goldman S., et al. Quantitative two-dimensional echocardiographic measurements are major predictors of adverse cardiovascular events after acute myocardial infarction. The protective effects of captopril. Circulation 1994; 89(1): 68-75. Doi: 10.1161/01.cir.89.1.68.
Adler A., van der Werf C., Postema PG., Rosso R., Bhuiyan ZA., Kalman JM., Vohra JK., Guevara-Valdivia ME., Marquez MF., Halkin A., et al. The phenomenon of "QT stunning": the abnormal QT prolongation provoked by standing persists even as the heart rate returns to normal in patients with long QT syndrome. Heart Rhythm 2012; 9(6): 901-8. Doi: 10.1016/j.hrthm.2012.01.026.
Ackerman MJ., Priori SG., Willems S., Berul C., Brugada R., Calkins H., Camm AJ., Ellinor PT., Gollob M., Hamilton R., et al. HRS/EHRA expert consensus statement on the state of genetic testing for the channelopathies and cardiomyopathies this document was developed as a partnership between the Heart Rhythm Society (HRS) and the European Heart Rhythm Association (EHRA). Heart Rhythm 2011; 8(8): 1308-39. Doi: 10.1016/j.hrthm.2011.05.020.
Wilde AAM., Semsarian C., Márquez MF., Shamloo AS., Ackerman MJ., Ashley EA., Sternick EB., Barajas-Martinez H., Behr ER., Bezzina CR., et al. Developed in partnership with and endorsed by the European Heart Rhythm Association (EHRA), a branch of the European Society of Cardiology (ESC), the Heart Rhythm Society (HRS), the Asia Pacific Heart Rhythm Society (APHRS), and the Latin American Heart Rhythm Society (LAHRS). European Heart Rhythm Association (EHRA)/Heart Rhythm Society (HRS)/Asia Pacific Heart Rhythm Society (APHRS)/Latin American Heart Rhythm Society (LAHRS) Expert Consensus Statement on the state of genetic testing for cardiac diseases. Europace 2022; 24(8): 1307-1367. Doi: 10.1093/europace/euac030.
Adler A., Novelli V., Amin AS., Abiusi E., Care M., Nannenberg EA., Feilotter H., Amenta S., Mazza D., Bikker H., et al. An International, Multicentered, Evidence-Based Reappraisal of Genes Reported to Cause Congenital Long QT Syndrome. Circulation 2020; 141(6): 418-428. Doi: 10.1161/CIRCULATIONAHA.119.043132.
Casey JP., Støve SI., McGorrian C., Galvin J., Blenski M., Dunne A., Ennis S., Brett F., King MD., Arnesen T., et al. NAA10 mutation causing a novel intellectual disability syndrome with Long QT due to N-terminal acetyltransferase impairment. Sci Rep 2015; 5: 16022. Doi: 10.1038/srep16022.
Hosseini SM., Kim R., Costain G., et al. Reappraisal of reported genes for sudden arrhythmic death: evidence-based evaluation of gene validity for Brugada syndrome. Circulation 2018; 138(12): 1195-1205. Doi: 10.1161/CIRCULATIONAHA.118.035070.
Yamagata K., Horie M., Aiba T., et al. Genotype-Phenotype Correlation of SCN5A Mutation for the Clinical and Electrocardiographic Characteristics of Probands With Brugada Syndrome A Japanese Multicenter Registry. Circulation 2017; 135(23): 2255-2270. Doi: 10.1161/CIRCULATIONAHA.117.027983
Giudicessi JR., Ackerman MJ. Exercise testing oversights underlie missed and delayed diagnosis of catecholaminergic polymorphic ventricular tachycardia in young sudden cardiac arrest survivors. Heart Rhythm 2019; 16(8): 1232-1239. Doi: 10.1016/j.hrthm.2019.02.012.
Corrado D., Perazzolo Marra M., Zorzi A., et al. Diagnosis of arrhythmogenic cardiomyopathy: the Padua criteria. International Journal Cardiology 2020; 319(15): 106-114. Doi: 10.1016/j.ijcard.2020.06.005.
Walsh R., Thomson KL., Ware JS., et al. Reassessment of Mendelian gene pathogenicity using 7,855 cardiomyopathy cases and 60,706 reference samples. Genetics in Medicine 2017; 19(2): 192-203. Doi: 10.1038/gim.2016.90.
Corrado D., van Tintelen PJ., McKenna WJ., Hauer RNW., et al. Arrhythmogenic right ventricular cardiomyopathy: evaluation of the current diagnostic criteria and differential diagnosis. European Heart Journal 2020; 41(14): 1414-1429. Doi: 10.1093/eurheartj/ehz669.
Tester DJ., Medeiros-Domingo A., Will ML., Haglund CM., et al. Cardiac channel molecular autopsy: insights from 173 consecutive cases of autopsynegative sudden unexplained death referred for postmortem genetic testing. Mayo Clinic Proceedings 2012 Jun; 87(6): 524-39. Doi: 10.1016/j.mayocp.2012.02.017.
Nucifora G., Muser D., Masci PG., et al. Prevalence and prognostic value of concealed structural abnormalities in patients with apparently idiopathic ventricular arrhythmias of left versus right ventricular origin: a magnetic resonance imaging study. Circulation: Arrhythmia and Electrophysiology 2014; 7(3): 456-62. Doi: 10.1161/CIRCEP.113.001172.
Curcio A., Mazzanti A., Bloise R., et al. Clinical presentation and outcome of Brugada syndrome diagnosed with the new 2013 criteria. Journal of Cardiovascular Electrophysiology 2016; 27(8): 937-943. Doi: 10.1111/jce.12997.
Bjune T., Risgaard B., Kruckow L., Glinge C., et al. Post-mortem toxicology in young sudden cardiac death victims: a nationwide co- hort study. Europace 2018; 20(4): 614-621. Doi: 10.1093/europace/euw435.
Papadakis M., Raju H., Behr ER., et al. Sudden cardiac death with autopsy findings of uncertain significance: potential for erroneous interpretation. Circulation: Arrhythmia and Electrophysiology 2013; 6(3): 588-96. Doi: 10.1161/CIRCEP.113.000111.
Van der Werf C., Hofman N., Tan HL., et al. Diagnostic yield in sudden unexplained death and aborted cardiac arrest in the young: the experience of a tertiary referral center in The Netherlands. Heart Rhythm 2010; 7(10): 1383-1389. Doi: 10.1016/j.hrthm.2010.05.036.
Wong LCH., Roses-Noguer F., Till JA., et al. Cardiac evaluation of pediatric relatives in sudden arrhythmic death syndrome: a 2-center experience. Circulation: Arrhythmia and Electrophysiology 2014; 7(5): 800-806. Doi: 10.1161/CIRCEP.114.001818.
Behr ER., Dalageorgou C., Christiansen M., Syrris P., et al. Sudden arrhythmic death syndrome: familial evaluation identifies inheritable heart disease in the majority of families. European Heart Journal 2008; 29(13): 1670-1680. Doi: 10.1093/eurheartj/ehn219.
Madhavan M., Friedman PA., Lennon RJ., et al. Implantable cardioverter-defibrillator therapy in patients with ventricular fibrillation out of hospital cardiac arrest secondary to acute coronary syndrome. Journal of the American Heart Association 2015; 4(2): e001255. Doi: 10.1161/JAHA.114.001255.
Gibbs C., Thalamus J., Heldal K., Holla ØL., Haugaa KH., Hysing J. Predictors of mortality in high-risk patients with QT prolongation in a community hospital. Europace 2018; 20(FI1): 99-107. Doi: 10.1093/europace/eux286.)
Simpson TF., Salazar JW., Vittinghoff E., Probert J., Iwahashi A., Olgin JE., Ursell P., Hart A., Moffatt E., Tseng ZH. Association of QT-Prolonging Medications With Risk of Autopsy-Defined Causes of Sudden Death. JAMA Intern Med 2020; 180(5): 698-706. Doi: 10.1001/jamainternmed.2020.0148.
Brugada J., Blom N., Sarquella-Brugada G., Blomstrom-Lundqvist C., Deanfield J., Janousek J., Abrams D., Bauersfeld U., Brugada R., Drago F., et al. Pharmacological and non-pharmacological therapy for arrhythmias in the pediatric population: EHRA and AEPC-Arrhythmia Working Group joint consensus statement. Europace 2013; 15(9): 1337-82. Doi: 10.1093/europace/eut082.
Schupp T., Behnes M., Zworowsky MV., Kim SH., Weidner K., Rusnak J., Kuche P., Müller J., Barth C., Reiser L., et al. Hypokalemia but not Hyperkalemia is Associated with Recurrences of Ventricular Tachyarrhythmias in ICD Recipients. Clin Lab 2020; 66(3). Doi: 10.7754/Clin.Lab.2019.190645.
Goyal A., Spertus JA., Gosch K., Venkitachalam L., Jones PG., Van den Berghe G., Kosiborod M. Serum potassium levels and mortality in acute myocardial infarction. JAMA 2012; 307(2): 157-64. Doi: 10.1001/jama.2011.1967.
Tzivoni D., Banai S., Schuger C., Benhorin J., Keren A., Gottlieb S., Stern S. Treatment of torsade de pointes with magnesium sulfate. Circulation 1988; 77(2): 392-7. Doi: 10.1161/01.cir.77.2.392.
Van de Voorde P., Turner NM., Djakow J., de Lucas N., Martinez-Mejias A., Biarent D., Bingham R., Brissaud O., Hoffmann F., Johannesdottir GB., et al. European Resuscitation Council Guidelines 2021: Paediatric Life Support. Resuscitation 2021; 161: 327-387. Doi: 10.1016/j.resuscitation.2021.02.015.
Soar J., Perkins GD., Maconochie I., Böttiger BW., Deakin CD., Sandroni C., Olasveengen TM., Wyllie J., Greif R., Lockey A., et al. European Resuscitation Council Guidelines for Resuscitation: 2018 Update - Antiarrhythmic drugs for cardiac arrest. Resuscitation 2019; 134: 99-103. Doi: 10.1016/j.resuscitation.2018.11.018.
Балыкова Л.А., Назарова И.С., Тишина А.Н. Лечение аритмий сердца у детей. Практическая медицина 2011; 53: 30-37.
Wyse DG., Friedman PL., Brodsky MA., Beckman KJ., Carlson MD., Curtis AB., Hallstrom AP., Raitt MH., Wilkoff BL., Greene HL.; AVID Investigators. Life-threatening ventricular arrhythmias due to transient or correctable causes: high risk for death in follow-up. J Am Coll Cardiol 2001; 38(6): 1718-24. Doi: 10.1016/s0735-1097(01)01597-2.
Ladejobi A., Pasupula DK., Adhikari S., Javed A., Durrani AF., Patil S., Qin D., Ahmad S., Munir MB., Rijal S., et al. Implantable Defibrillator Therapy in Cardiac Arrest Survivors With a Reversible Cause. Circ Arrhythm Electrophysiol 2018; 11(3): e005940. doi: 10.1161/CIRCEP.117.005940.
Silvetti, M.S.; Colonna, D.; Gabbarini, F.; Porcedda, G.; Rimini, A.; D’Onofrio, A.; Leoni, L. New Guidelines of Pediatric Cardiac Implantable Electronic Devices: What Is Changing in Clinical Practice? J. Cardiovasc. Dev. Dis 2024, 11(4): 99. Doi: 10.3390/jcdd11040099.
Link MS., Berkow LC., Kudenchuk PJ., Halperin HR., Hess EP., Moitra VK., Neumar RW., O'Neil BJ., Paxton JH., Silvers SM., et al. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015; 132(18 Suppl 2): S444-64. Doi: 10.1161/CIR.0000000000000261.
Stiell IG., Wells GA., Field B., Spaite DW., Nesbitt LP., De Maio VJ., Nichol G., Cousineau D., Blackburn J., Munkley D., et al. Advanced cardiac life support in out-of-hospital cardiac arrest. N Engl J Med 2004; 351(7): 647-56. Doi: 10.1056/NEJMoa040325.
Sasson C., Rogers MA., Dahl J., Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 2010; 3(1): 63-81. Doi: 10.1161/CIRCOUTCOMES.109.889576.
Cobb LA., Fahrenbruch CE., Walsh TR., Copass MK., Olsufka M., Breskin M., Hallstrom AP. Influence of cardiopulmonary resuscitation prior to defibrillation in patients with out-of-hospital ventricular fibrillation. JAMA 1999; 281(13): 1182-8. Doi: 10.1001/jama.281.13.1182.
Cronin EM., Bogun FM., Maury P., Peichl P., et al. 2019 HRS/EHRA/APHRS/LAHRS expert consensus statement on catheter ablation of ventricular arrhythmias. Europace 2019; 21(8): 1143-1144. Doi: 10.1093/europace/euz132.
Van de Voorde P, Turner NM, Djakow J, de Lucas N, Martinez-Mejias A, Biarent D, Bingham R, Brissaud O, Hoffmann F, Johannesdottir GB, Lauritsen T, Maconochie I. European Resuscitation Council Guidelines 2021: Paediatric Life Support. Resuscitation. 2021 Apr;161:327-387.
Carolina Ornelas-Dorian, Kevin R., William B., Amal M., Jeffrey T. Assessment and Management of a Child With Wide Complex Tachycardia. Annals of Emergency Medicine 2024. 83: 42-45. Doi: 10.1016/j.annemergmed.2023.08.007.
Dorian P., Cass D., Schwartz B., Cooper R., Gelaznikas R., Barr A. Amiodarone as compared with lidocaine for shock-resistant ventricular fibrillation. N Engl J Med 2002; 346(12): 884-90. Doi: 10.1056/NEJMoa013029.
Kudenchuk PJ., Brown SP., Daya M., Rea T., Nichol G., Morrison LJ., Leroux B., Vaillancourt C., Wittwer L., Callaway CW., et al. Resuscitation Outcomes Consortium Investigators. Amiodarone, Lidocaine, or Placebo in Out-of-Hospital Cardiac Arrest. N Engl J Med 2016; 374(18): 1711-22. Doi: 10.1056/NEJMoa1514204.
Herlitz J., Ekström L., Wennerblom B., Axelsson A., Bång A., Lindkvist J., Persson NG., Holmberg S. Lidocaine in out-of-hospital ventricular fibrillation. Does it improve survival? Resuscitation 1997; 33(3): 199-205. Doi: 10.1016/s0300-9572(96)01018-0.
Gueugniaud PY., Mols P., Goldstein P., Pham E., Dubien PY., Deweerdt C., Vergnion M., Petit P., Carli P. A comparison of repeated high doses and repeated standard doses of epinephrine for cardiac arrest outside the hospital. European Epinephrine Study Group. N Engl J Med 1998; 339(22): 1595-601. Doi: 10.1056/NEJM199811263392204.
Hagihara A., Hasegawa M., Abe T., Nagata T., Wakata Y., Miyazaki S. Prehospital epinephrine use and survival among patients with out-of-hospital cardiac arrest. JAMA 2012; 307(11): 1161-8. Doi: 10.1001/jama.2012.294.
Maconochie IK., Aickin R., Hazinski MF., Atkins DL., Bingham R., Couto TB., Guerguerian AM., Nadkarni VM., Ng KC., Nuthall GA., et al. Pediatric Life Support Collaborators. Pediatric Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Resuscitation 2020; 156: A120-A155. Doi: 10.1016/j.resuscitation.2020.09.013.
Topjian AA., Raymond TT., Atkins D., Chan M., Duff JP., Joyner BL Jr., Lasa JJ., Lavonas EJ., Levy A., Mahgoub M., et al. Pediatric Basic and Advanced Life Support Collaborators. Part 4: Pediatric Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020; 142(16_suppl_2): S469-S523. Doi: 10.1161/CIR.0000000000000901.
Long B., Koyfman A. Best Clinical Practice: Emergency Medicine Management of Stable Monomorphic Ventricular Tachycardia. J Emerg Med 2017; 52(4): 484-492. Doi: 10.1016/j.jemermed.2016.09.010.
Tang PT., Do DH., Li A., Boyle NG. Team Management of the Ventricular Tachycardia Patient. Arrhythm Electrophysiol Rev 2018; 7(4): 238-246. Doi: 10.15420/aer.2018.37.2.
Ohlow MA., Beierlein A., Müller S., von Korn H., Geller JC., Yu J., Lauer B. Stable tachycardia with wide QRS complex in pre-hospital emergency medicine. Dtsch Med Wochenschr 2005; 130(47): 2694-8. Doi: 10.1055/s-2005-922056.
Patel KK., Spertus JA., Khariton Y., Tang Y., Curtis LH., Chan PS. American Heart Association’s Get With the Guidelines–Resuscitation Investigators. Association Between Prompt Defibrillation and Epinephrine Treatment With Long-Term Survival After In-Hospital Cardiac Arrest. Circulation 2018; 137(19): 2041-2051. Doi: 10.1161/CIRCULATIONAHA.117.030488.
Eckardt L., Breithardt G., Kirchhof P. Approach to wide complex tachycardias in patients without structural heart disease. Heart 2006; 92(5): 704-11. Doi: 10.1136/hrt.2005.063792.
Hudson KB., Brady WJ., Chan TC., Pollack M., Harrigan RA. Electrocardiographic manifestations: ventricular tachycardia. J Emerg Med 2003; 25(3): 303-14. Doi: 10.1016/s0736-4679(03)00207-5.
Miller JM., Das MK., Yadav AV., Bhakta D., Nair G, Alberte C. Value of the 12-lead ECG in wide QRS tachycardia. Cardiol Clin 2006; 24(3): 439-51. Doi: 10.1016/j.ccl.2006.03.003.
Goldberger ZD., Rho RW., Page RL. Approach to the diagnosis and initial management of the stable adult patient with a wide complex tachycardia. Am J Cardiol 2008; 101(10): 1456-66. Doi: 10.1016/j.amjcard.2008.01.024.
Abedin Z. Differential diagnosis of wide QRS tachycardia: A review. J Arrhythm 2021; 37(5): 1162-1172. Doi: 10.1002/joa3.12599.
Marill KA., Wolfram S., Desouza IS., Nishijima DK., Kay D., Setnik GS., Stair TO., Ellinor PT. Adenosine for wide-complex tachycardia: efficacy and safety. Crit Care Med 2009; 37(9): 2512-8. Doi: 10.1097/CCM.0b013e3181a93661.
Sharma AD, Klein GJ, Yee R. Intravenous adenosine triphosphate during wide QRS complex tachycardia: safety, therapeutic efficacy, and diagnostic utility. Am J Med. 1990 Apr;88(4):337-43.
Brugada J., Katritsis D.G., Arbelo E., et al. 2019 ESC Guidelines for the management of patients with supraventricular tachycardia. The task force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC). European Heart Journal 2020; 41(5): 655-720. Doi: 10.1093/eurheartj/ehz467.
Ortiz M., Martín A., Arribas F., Coll-Vinent B., Del Arco C., Peinado R., Almendral J. PROCAMIO Study Investigators. Randomized comparison of intravenous vs. intravenous for the acute treatment of tolerated wide QRS tachycardia: the PROCAMIO study. Eur Heart J 2017; 38(17): 1329-1335. Doi: 10.1093/eurheartj/ehw230.
Buxton AE., Marchlinski FE., Doherty JU., et al. Repetitive, monomorphic ventricular tachycardia: clinical and electrophysiologic characteristics in patients with and patients without organic heart disease. American Journal of Cardiology 1984; 54(8): 997-1002. Doi: 10.1016/s0002-9149(84)80133-2.
Griffith MJ., Garratt CJ., Rowland E., et al. Effects of intravenous adenosine on verapamil-sensitive ‘idiopathic’ ventricular tachycardia. American Journal of Cardiology 1994; 73(11): 759-64. Doi: 10.1016/0002-9149(94)90877-x.
Buxton AE., Marchlinski FE., Doherty JU., et. al. Hazards of intravenous verapamil for sustained ventricular tachycardia. American Journal of Cardiology 1987; 59(12): 1107-1110. Doi: 10.1016/0002-9149(87)90857-5.
Rankin AC., Rae A.P., Cobbe SM. Misuse of intravenous verapamil in patients with ventricular tachycardia. Lancet 1987; 2(8557): 472-474. Doi: 10.1016/s0140-6736(87)91790-9.
Kehr J, Binfield A, Maxwell F, Hornung T, Skinner JR. Fascicular tachycardiain infancy and the use of verapamil: a case series and literature review. Arch Dis Child 2019; 104(8): 789-792. Doi: 10.1136/archdischild-2018-315617.
Pedersen CT., Kay GN., Kalman J., Borggrefe M., et al. EHRA/HRS/APHRS expert consensus on ventricular arrhythmias. Europace 2014; 16(9): 1257-1283. Doi: 10.1093/europace/euu194.
Kowlgi GN., Cha Y-M. Management of ventricular electrical storm: a contemporary appraisal. Europace 2020; 22(12): 1768-1780. Doi: 10.1093/europace/euaa232.
Guerra F., Shkoza M., Scappini L., Flori M., et al. Role of electrical storm as a mortality and morbidity risk factor and its clinical predictors: a meta-analysis. Europacen 2014; 16(3): 347-353. Doi: 10.1093/europace/eut304.
Noda T., Kurita T., Nitta T., Chiba Y., et al. Significant impact of electrical storm on mortality in patients with structural heart disease and an implantable cardiac defibrillator. International Journal of Cardiology 2018; 255(15): 85-91. Doi: 10.1016/j.ijcard.2017.11.077.
Soar J., Maconochie I., Wyckoff MH., Olasveengen TM., et al. 2019 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: summary from the basic life support; advanced life support; pediatric life support; neonatal life support; education, implementation, and teams; and first aid task force. Circulation 2019; 140(24): e826-e880. Doi: 10.1161/CIR.0000000000000734.
Eifling M., Razavi M., Massumi A. The evaluation and management of electrical storm. Texas Heart Institute Journal 2011; 38(2): 111-21.
Chatzidou S., Kontogiannis C., Tsilimigras DI., et al. Propranolol versus metoprolol for treatment of electrical storm in patients with implantable cardioverter-defibrillator. Journal of the American College of Cardiology 2018; 71(17): 1897-1906. Doi: 10.1016/j.jacc.2018.02.056.
Connolly SJ., Dorian P., Roberts RS., Gent M., et al. Comparison of beta-blockers, amiodarone plus beta-blockers, or sotalol for prevention of shocks from implantable cardioverter defibrillators: the OPTIC Study: a randomized trial. JAMA 2006; 295(2): 165-71. Doi: 10.1001/jama.295.2.165.
Gorgels AP., van den Dool A., Hofs A., Mulleneers R., Smeets JL., Vos MA., Wellens HJ. Comparison of procainamide and lidocaine in terminating sustained monomorphic ventricular tachycardia. Am J Cardiol 1996; 78(1): 43-6. Doi: 10.1016/s0002-9149(96)00224-x.
Martí-Carvajal AJ., Simancas-Racines D., Anand V., Bangdiwala S. Prophylactic lidocaine for myocardial infarction. Cochrane Database Syst Rev 2015; 2015(8): CD008553. Doi: 10.1002/14651858.CD008553.pub2.
Martins RP, Urien JM, Barbarot N, Rieul G, Sellal JM, Borella L, Clementy N, Bisson A, Guenancia C, Sagnard A, Schumacher S, Gandjbakhch E, Duchateau J, Tixier R, Goepp A, Hamon D, Lellouche N, Champ-Rigot L, Milliez P, Marijon E, Varlet E, Garcia R, Degand B, Bouju P, Mabo P, Leclercq C, Behar N, Pavin D, de Chillou C, Sacher F, Galand V. Effectiveness of Deep Sedation for Patients With Intractable Electrical Storm Refractory to Antiarrhythmic Drugs. Circulation 2020; 142(16): 1599-1601. Doi: 10.1161/CIRCULATIONAHA.120.047468.
Carbucicchio C., Santamaria M., Trevisi N., Maccabelli G., Giraldi F., Fassini G., Riva S., Moltrasio M., Cireddu M., Veglia F., et al. Catheter ablation for the treatment of electrical storm in patients with implantable cardioverter-defibrillators: short- and long-term outcomes in a prospective single-center study. Circulation 2008; 117(4): 462-9. Doi: 10.1161/CIRCULATIONAHA.106.686534
Vergara P., Tung R., Vaseghi M., Brombin C., Frankel DS., Di Biase L., Nagashima K., Tedrow U., Tzou WS., Sauer WH., et al. Successful ventricular tachycardia ablation in patients with electrical storm reduces recurrences and improves survival. Heart Rhythm 2018; 15(1): 48-55. Doi: 10.1016/j.hrthm.2017.08.022. Epub 2017 Aug 24. Erratum in: Heart Rhythm. 2018 Mar; 15(3):472. doi: 10.1016/j.hrthm.2018.02.002.
Haïssaguerre M., Shah DC., Jaïs P., Shoda M., Kautzner J., Arentz T., Kalushe D., Kadish A., Griffith M., Gaïta F., et al. Role of Purkinje conducting system in triggering of idiopathic ventricular fibrillation. Lancet 2002; 359(9307): 677-8. Doi: 10.1016/S0140-6736(02)07807-8.
Komatsu Y., Hocini M., Nogami A., Maury P., Peichl P., Iwasaki YK., Masuda K., Denis A., Voglimacci-Stephanopoli Q., Wichterle D., et al. Catheter Ablation of Refractory Ventricular Fibrillation Storm After Myocardial Infarction. Circulation 2019; 139(20): 2315-2325. Doi: 10.1161/CIRCULATIONAHA.118.037997.
Knecht S., Sacher F., Wright M., Hocini M., Nogami A., Arentz T., Petit B., Franck R., De Chillou C., Lamaison D., et al. Long-term follow-up of idiopathic ventricular fibrillation ablation: a multicenter study. J Am Coll Cardiol 2009; 54(6): 522-8. Doi: 10.1016/j.jacc.2009.03.065.
Peichl P., Cihák R., Kozeluhová M., Wichterle D., Vancura V., Kautzner J. Catheter ablation of arrhythmic storm triggered by monomorphic ectopic beats in patients with coronary artery disease. J Interv Card Electrophysiol 2010; 27(1): 51-9. Doi: 10.1007/s10840-009-9443-2.
Fudim M., Boortz-Marx R., Ganesh A., Waldron NH., Qadri YJ., Patel CB., Milano CA., Sun AY, Mathew JP., Piccini JP. Stellate ganglion blockade for the treatment of refractory ventricular arrhythmias: A systematic review and meta-analysis. J Cardiovasc Electrophysiol 2017; 28(12): 1460-1467. Doi: 10.1111/jce.13324.
Do DH., Bradfield J., Ajijola OA., Vaseghi M., Le J, Rahman S., Mahajan A., Nogami A., Boyle NG., Shivkumar K. Thoracic Epidural Anesthesia Can Be Effective for the Short-Term Management of Ventricular Tachycardia Storm. J Am Heart Assoc 2017; 6(11): e007080. Doi: 10.1161/JAHA.117.007080. PMID: 29079570; PMCID: PMC5721785.
Vaseghi M., Barwad P., Malavassi Corrales FJ., Tandri H., Mathuria N., Shah R., Sorg JM., Gima J., Mandal K., Sàenz Morales LC., et al. Cardiac Sympathetic Denervation for Refractory Ventricular Arrhythmias. J Am Coll Cardiol 2017; 69(25): 3070-3080. Doi: 10.1016/j.jacc.2017.04.035.
Vaseghi M., Gima J., Kanaan C., Ajijola OA., Marmureanu A., Mahajan A., Shivkumar K. Cardiac sympathetic denervation in patients with refractory ventricular arrhythmias or electrical storm: intermediate and long-term follow-up. Heart Rhythm 2014; 11(3): 360-6. Doi: 10.1016/j.hrthm.2013.11.028.
Le Pennec-Prigent S., Flecher E., Auffret V., Leurent G., Daubert JC., Leclercq C., Mabo P., Verhoye JP., Martins RP. Effectiveness of Extracorporeal Life Support for Patients With Cardiogenic Shock Due To Intractable Arrhythmic Storm. Crit Care Med 2017; 45(3): e281-e289. Doi: 10.1097/CCM.0000000000002089.
Mariani S., Napp LC., Lo Coco V., Delnoij TSR., Luermans JGLM., Ter Bekke RMA., Timmermans C., Li T., Dogan G., Schmitto JD., et al. Mechanical circulatory support for life-threatening arrhythmia: A systematic review. Int J Cardiol 2020; 308: 42-49. Doi: 10.1016/j.ijcard.2020.03.045.
Muser D., Liang JJ., Castro SA., Hayashi T., Enriquez A., Troutman GS., McNaughton NW., Supple G., Birati EY., Schaller R., et al. Outcomes with prophylactic use of percutaneous left ventricular assist devices in high-risk patients undergoing catheter ablation of scar-related ventricular tachycardia: A propensity-score matched analysis. Heart Rhythm 2018; 15(10): 1500-1506. Doi: 10.1016/j.hrthm.2018.04.028.
Mathuria N., Wu G., Rojas-Delgado F., Shuraih M., Razavi M., Civitello A., Simpson L., Silva G., Wang S., Elayda M., Kantharia B., et al. Outcomes of pre-emptive and rescue use of percutaneous left ventricular assist device in patients with structural heart disease undergoing catheter ablation of ventricular tachycardia. J Interv Card Electrophysiol 2017; 48(1): 27-34. Doi: 10.1007/s10840-016-0168-8.
Ponikowski P., Voors AA., Anker SD., Bueno H., Cleland JGF., Coats AJS., Falk V., González-Juanatey JR., Harjola VP., Jankowska EA., et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016; 37(27): 2129-2200. Doi: 10.1093/eurheartj/ehw128.
McDonagh TA., Metra M., Adamo M., Gardner RS., Baumbach A., Böhm M., Burri H., Butler J., Čelutkienė J., Chioncel O., et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 2021; 42(36): 3599-3726. Doi: 10.1093/eurheartj/ehab368.
AlJaroudi WA., Refaat MM., Habib RH., Al-Shaar L., Singh M., Gutmann R., Bloom HL., Dudley SC., Ellinor PT., Saba SF., et al. Genetic Risk Assessment of Defibrillator Events Investigators. Effect of angiotensin-converting enzyme inhibitors and receptor blockers on appropriate implantable cardiac defibrillator shock in patients with severe systolic heart failure (from the GRADE Multicenter Study). Am J Cardiol 2015; 115(7): 924-31. Doi: 10.1016/j.amjcard.2015.01.020.
Pitt B., Remme W., Zannad F., Neaton J., Martinez F., Roniker B., Bittman R., Hurley S., Kleiman J., Gatlin M; Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study Investigators. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 2003; 348(14): 1309-21. Doi: 10.1056/NEJMoa030207.
McMurray JJ., Packer M., Desai AS., Gong J., Lefkowitz MP., Rizkala AR., Rouleau JL., Shi VC., Solomon SD., Swedberg K., et al. PARADIGM-HF Investigators and Committees. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med 2014; 371(11): 993-1004. Doi: 10.1056/NEJMoa1409077.
Packer M., Anker SD., Butler J., Filippatos G., Pocock SJ., Carson P., Januzzi J., Verma S., Tsutsui H., Brueckmann M., et al. EMPEROR-Reduced Trial Investigators. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N Engl J Med 2020; 383(15): 1413-1424. Doi: 10.1056/NEJMoa2022190.
Desai AS., McMurray JJ., Packer M., Swedberg K., Rouleau JL., Chen F., Gong J., Rizkala AR., Brahimi A., Claggett B., et al. Effect of the angiotensin-receptor-neprilysin inhibitor LCZ696 compared with enalapril on mode of death in heart failure patients. Eur Heart J 2015; 36(30): 1990-7. Doi: 10.1093/eurheartj/ehv186.
Жарова О.П., Басаргина Е.Н., Фисенко А.П., Гандаева Л.А., Деревнина Ю.В., Эффективность медикаментозной терапии хронической сердечной недостаточности у детей раннего возраста с дилатационной кардиомиопатией. Российский педиатрический журнал 2019; 22(4): 219-225. DoI: 10.18821/1560-9561-2019-22-4-219-225.
Kirk R., Dipchand AI., Rosenthal DN., Addonizio L., Burch M., Chrisant M., Dubin A., Everitt M., Gajarski R., Mertens L., et al. The International Society for Heart and Lung Transplantation Guidelines for the management of pediatric heart failure: Executive summary. J Heart Lung Transplant 2014; 33(9): 888-909. Doi: 10.1016/j.healun.2014.06.002.
Das BB. A Review of Contemporary and Future Pharmacotherapy for Chronic Heart Failure in Children. Children (Basel) 202; 11(7): 859. Doi: 10.3390/children11070859.
Rupp S., Apitz C., Tholen L., Latus H., Ostermayer SH., Schmidt D., Bauer J., Schranz D. Upgraded heart failure therapy leads to an improved outcome of dilated cardiomyopathy in infants and toddlers. Cardiol Young 2015; 25(7): 1300-5. Doi: 10.1017/S1047951114002406.
Chavey WE., Hogikyan RV., Van Harrison R., Nicklas JM. Heart Failure Due to Reduced Ejection Fraction: Medical Management. Am Fam Physician 2017; 95(1): 13-20.
Castro Díez C., Khalil F., Schwender H., Dalinghaus M., Jovanovic I., Makowski N., Male C., Bajcetic M., van der Meulen M., de Wildt SN., et al. Pharmacotherapeutic management of paediatric heart failure and ACE-I use patterns: a European survey. BMJ Paediatr Open 2019; 3(1): e000365. Doi: 10.1136/bmjpo-2018-000365.
Bogle C., Colan SD., Miyamoto SD., Choudhry S., Baez-Hernandez N., Brickler MM., Feingold B., Lal AK., Lee TM., Canter CE., et al. American Heart Association Young Hearts Pediatric Heart Failure and Transplantation Committee of the Council on Lifelong Congenital Heart Disease and Heart Health in the Young (Young Hearts). Treatment Strategies for Cardiomyopathy in Children: A Scientific Statement From the American Heart Association. Circulation 2023; 148(2): 174-195. Doi: 10.1161/CIR.0000000000001151.
Nguyen KT., Vittinghoff E., Dewland TA., Dukes JW., Soliman EZ., Stein PK., Gottdiener JS., Alonso A., Chen LY., Psaty BM., et al. Ectopy on a Single 12-Lead ECG, Incident Cardiac Myopathy, and Death in the Community. J Am Heart Assoc 2017; 6(8): e006028. Doi: 10.1161/JAHA.117.006028.
Dukes JW., Dewland TA., Vittinghoff E., Mandyam MC., Heckbert SR., Siscovick DS., Stein PK., Psaty BM., Sotoodehnia N., Gottdiener JS., et al. Ventricular Ectopy as a Predictor of Heart Failure and Death. J Am Coll Cardiol 2015; 66(2): 101-9. Doi: 10.1016/j.jacc.2015.04.062.
Gill JS., Mehta D., Ward DE., Camm AJ. Efficacy of flecainide, sotalol, and verapamil in the treatment of right ventricular tachycardia in patients without overt cardiac abnormality. Br Heart J 1992; 68(4): 392-7. Doi: 10.1136/hrt.68.10.392.
Shimizu W. Arrhythmias originating from the right ventricular outflow tract: how to distinguish "malignant" from "benign"? Heart Rhythm 2009; 6(10): 1507-11. Doi: 10.1016/j.hrthm.2009.06.017.
Jamil HA., Mohammed SA., Gierula J., Paton MF., Lowry JE., Cubbon RM., Kearney MT., Witte KKA. Prognostic Significance of Incidental Nonsustained Ventricular Tachycardia Detected on Pacemaker Interrogation. Am J Cardiol 2019; 123(3): 409-413. Doi: 10.1016/j.amjcard.2018.10.040.
Dabbagh GS., Bogun F. Predictors and Therapy of Cardiomyopathy Caused by Frequent Ventricular Ectopy. Curr Cardiol Rep 2017; 19(9): 80. Doi: 10.1007/s11886-017-0887-1.
Hyman MC., Mustin D., Supple G., Schaller RD., Santangeli P., Arkles J., Lin D., Muser D., Dixit S., Nazarian S., et al. Class IC antiarrhythmic drugs for suspected premature ventricular contraction-induced cardiomyopathy. Heart Rhythm 2018; 15(2): 159-163. Doi: 10.1016/j.hrthm.2017.12.018.
Ling Z., Liu Z., Su L. et al. Radiofrequency ablation versus antiarrhythmic medication for treatment of ventricular premature beats from the right ventricular outflow tract: prospective randomized study. Circulation: Arrhythmia and Electrophysiology 2014; 7(2): 237-243. Doi: 10.1161/CIRCEP.113.000805.
Latchamsetty R., Yokokawa M., Morady F., et al. Multicenter outcomes for catheter ablation of idiopathic premature ventricular complexes. JACC Clinical Electrophysiology 2015; 1(3): 116-123. Doi: 10.1016/j.jacep.2015.04.005.
Primeau R., Agha A., Giorgi C., Shenasa M. Long term efficacy and toxicity of amiodarone in the treatment of refractory cardiac arrhythmias. Canadian Journal of Cardiology 1989; 5(2): 98-104.
R. A. Bertels, Janneke A. E. Kammeraad, A. M. Zeelenberg, et al. The Efcacy of Anti Arrhythmic Drugs in Children With Idiopathic Frequent Symptomatic or Asymptomatic Premature Ventricular Complexes With or Without Asymptomatic Ventricular Tachycardia: a Retrospective Multi Center Study. Pediatr Cardiol. 2021; 42(4): 883-890. Doi: 10.1007/s00246-021-02556-7.
Mont L., Seixas T., Brugada P., Brugada J., et al. Clinical and electrophysiologic characteristics of exercise-related idiopathic ventricular tachycardia. The American Journal of Cardiology 1991; 68(9): 897-900. Doi: 10.1016/0002-9149(91)90405-a.
Toivonen L., Nieminen M. Persistent ventricular tachycardia resulting in left ventricular dilatation treated with verapamil. International Journal of Cardiology 1986; 13(3): 361-365. Doi: 10.1016/0167-5273(86)90120-8.
Singh B., Kaul U., Talwar KK., Wasir H.S. Reversibility of tachycardia induced cardiomyopathy following the cure of idiopathic left ventricular tachycardia using radiofrequency energy. Pacing Clinical Electrophysiology 1996; 19(9): 1391-1392. Doi: 10.1111/j.1540-8159.1996.tb04222.x.
Stec S., et al. Benign symptomatic premature ventricular complexes: short− and long− term efficacy of antiarrhythmic drugs and radiofrequency ablation. Polish Heart Journal (Kardiologia Polska) 2012; 70(4): 351-358.
Krittayaphong R., Bhuripanyo K., Punlee K., Kangkagate C., Chaithiraphan S. Effect of atenolol on symptomatic ventricular arrhythmia without structural heart disease: a randomized placebo-controlled study. Am Heart J 2002; 144(6): e10. Doi: 10.1067/mhj.2002.125516.
Kuhlkamp V., Mewis C., Mermi J., et al. Suppression of sustained ventricular tachyarrhythmias: a comparison of d,l-sotalol with no antiarrhythmic drug treatment. J Am Coll Cardiol 1999; 33(1): 46-52. Doi: 10.1016/s0735-1097(98)00521-x.
Capucci A, Di Pasquale G, Boriani G. A double-blind crossover comparison of flecainide and slow-release mexiletine in the treatment of stable premature ventricular complexes. Int J Clin Pharmacol Res 1991; 11(1): 23-33.
Лоскутов Н.С. Этацизин в коррекции доброкачественных желудочковых нарушений ритма у больных ИБС и гипертонической болезнью / Н.С. Лоскутов, М.Б. Нагорный // Известия Российской военно-медицинской академии. – 2022. – Т. 41, № S2. – С. 272-276.
Соколов С.Ф., Бакалов С.А., Миронова Н.А., Рогова М.М., Малкина Т.А., Голицын С.П. Эффективность и безопасность аллапинина при краткосрочном и длительном лечении больных с доброкачественной желудочковой экстрасистолией. Кардиология 2014; 1: 20-26.
Влияние этацизина и атенолола на аритмии у больных с различными заболеваниями сердца / А. Макарова, А. Евдокименко, Т. М. Ибрагимова, Э.Оморова // Здравоохранение Кыргызстана. – 2009. – № 1. – С. 72-74.
Новые возможности применения неинвазивных электрофизиологических предикторов внезапной сердечной смерти: прогнозирование эффективности и безопасности антиаритмической терапии / Д.А. Царегородцев, А.В. Седов, Н.В. Мельник [и др.] // Кардиология и сердечно-сосудистая хирургия. – 2015. – Т. 8, № 6. – С. 114-121.
Oeffl N., Schober L., Faudon P., Schweintzger S., Manninger M., Köstenberger M., Sallmon H., Scherr D., Kurath-Koller S. Antiarrhythmic Drug Dosing in Children-Review of the Literature. Children (Basel) 2023; 10(5): 847. Doi: 10.3390/children10050847.
Ruberman W., Weinblatt E., Goldberg JD., et al. Ventricular premature beats and mortality after myocardial infarction. The New England Journal of Medicine 1977; 297(14): 750-757. Doi: 10.1056/NEJM197710062971404.
Engström G., Hedblad B., Janzon L., Juul-Möller S. Ventricular arrhythmias during 24-h ambulatory ECG recording: incidence, risk factors and prognosis in men with and without a history of cardiovascular disease. J Intern Med 1999; 246(4): 363-72. Doi: 10.1046/j.1365-2796.1999.00509.x.
Hoffmann A., Bühler FR., Burckhardt D. High-grade ventricular ectopic activity and 5-year survival in patients with chronic heart disease and in healthy subjects. Cardiology 1983; 70 Suppl 1: 82-7. Doi: 10.1159/000173635.
Bikkina M., Larson MG., Levy D. Asymptomatic ventricular arrhythmias and mortality risk in subjects with left ventricular hypertrophy. J Am Coll Cardiol 1993; 22(4): 1111-6. Doi: 10.1016/0735-1097(93)90424-y.
Adabag AS., Casey SA., Kuskowski MA., Zenovich AG., Maron BJ. Spectrum and prognostic significance of arrhythmias on ambulatory Holter electrocardiogram in hypertrophic cardiomyopathy. J Am Coll Cardiol 2005; 45(5): 697-704. Doi: 10.1016/j.jacc.2004.11.043.
Freemantle N., Cleland J., Young P., Mason J., Harrison J. beta Blockade after myocardial infarction: systematic review and meta regression analysis. BMJ 1999; 318(7200): 1730-7. Doi: 10.1136/bmj.318.7200.1730.
Magalie Ladouceur, Victor Waldmann, Stefano Bartoletti, Marie-A Chaix, Paul Khairy, Ventricular arrhythmia in congenital heart diseases with a systemic right ventricle, International Journal of Cardiology Congenital Heart Disease, Volume 13, 2023, 100463, ISSN 2666-6685, https://doi.org/10.1016/j.ijcchd.2023.100463
Ono K., Iwasaki YK., Akao M., Ikeda T., Ishii K., Inden Y., Kusano K., Kobayashi Y., Koretsune Y., Sasano T., et al. J Arrhythm 2022; 38(6): 833-973. Doi: 10.1002/joa3.12714.
Al-Gobari M., El Khatib C., Pillon F., Gueyffier F. β-Blockers for the prevention of sudden cardiac death in heart failure patients: a meta-analysis of randomized controlled trials. BMC Cardiovasc Disord 2013; 13: 52. Doi: 10.1186/1471-2261-13-52.
Cleophas TJ., Zwinderman AH. Beta-blockers and heart failure: meta-analysis of mortality trials. Int J Clin Pharmacol Ther 2001; 39(9): 383-8. Doi: 10.5414/cpp39383.
Hjalmarson A. Effects of beta blockade on sudden cardiac death during acute myocardial infarction and the postinfarction period. Am J Cardiol. 1997; 80(9B): 35J-39J. Doi: 10.1016/s0002-9149(97)00837-0.
Al-Gobari M., Al-Aqeel S., Gueyffier F., Burnand B. Effectiveness of drug interventions to prevent sudden cardiac death in patients with heart failure and reduced ejection fraction: an overview of systematic reviews. BMJ Open 2018; 8(7): e021108. Doi: 10.1136/bmjopen-2017-021108.
Baman TS., Lange DC., Ilg KJ., Gupta SK., Liu TY., Alguire C., Armstrong W., Good E., Chugh A., Jongnarangsin K., Pelosi F Jr., et al. Relationship between burden of premature ventricular complexes and left ventricular function. Heart Rhythm 2010; 7(7): 865-9. Doi: 10.1016/j.hrthm.2010.03.036.
Julian DG., Camm AJ., Frangin G., Janse MJ., Munoz A., Schwartz PJ., Simon P. Randomised trial of effect of amiodarone on mortality in patients with left-ventricular dysfunction after recent myocardial infarction: EMIAT. European Myocardial Infarct Amiodarone Trial Investigators. Lancet 1997; 349(9053): 667-74. Doi: 10.1016/s0140-6736(96)09145-3.
Cairns JA., Connolly SJ., Roberts R., Gent M. Randomised trial of outcome after myocardial infarction in patients with frequent or repetitive ventricular premature depolarisations: CAMIAT. Canadian Amiodarone Myocardial Infarction Arrhythmia Trial Investigators. Lancet 1997; 349(9053): 675-82. Doi: 10.1016/s0140-6736(96)08171-8.
Echt DS., Liebson PR., Mitchell LB., Peters RW., Obias-Manno D., Barker AH., Arensberg D., Baker A., Friedman L., Greene HL., et al. Mortality and morbidity in patients receiving encainide, flecainide, or placebo. The Cardiac Arrhythmia Suppression Trial. N Engl J Med 1991; 324(12): 781-8. Doi: 10.1056/NEJM199103213241201.
Cardiac Arrhythmia Suppression Trial II Investigators. Effect of the antiarrhythmic agent moricizine on survival after myocardial infarction. N Engl J Med 1992; 327(4): 227-33. Doi: 10.1056/NEJM199207233270403.
Ho AT., Pai SM., Timothy P., Pai RG. Effect of concomitant antiarrhythmic therapy on survival in patients with implantable cardioverter defibrillators. Pacing Clin Electrophysiol 2005; 28(7): 647-53. Doi: 10.1111/j.1540-8159.2005.00164.x.
Hayes DL., Boehmer JP., Day JD., Gilliam FR. 3rd, Heidenreich PA., Seth M., Jones PW., Saxon LA. Cardiac resynchronization therapy and the relationship of percent biventricular pacing to symptoms and survival. Heart Rhythm 2011; 8(9): 1469-75. Doi: 10.1016/j.hrthm.2011.04.015.
Bardy GH., Lee KL., Mark DB., Poole JE., Packer DL., Boineau R., Domanski M., Troutman C., Anderson J., Johnson G., et al. Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 2005; 352(3): 225-37. Doi: 10.1056/NEJMoa043399.
Vorperian VR., Havighurst TC., Miller S., January CT. Adverse effects of low dose amiodarone: a meta-analysis. J Am Coll Cardiol 1997; 30(3): 791-8. Doi: 10.1016/s0735-1097(97)00220-9.
Kuck KH., Cappato R., Siebels J., Rüppel R. Randomized comparison of antiarrhythmic drug therapy with implantable defibrillators in patients resuscitated from cardiac arrest: the Cardiac Arrest Study Hamburg (CASH). Circulation 2000; 102(7): 748-54. Doi: 10.1161/01.cir.102.7.748.
Furberg CD., Yusuf S. Effect of drug therapy on survival in chronic congestive heart failure. Am J Cardiol 1988; 62(2): 41A-45A. Doi: 10.1016/s0002-9149(88)80084-5.
Mahé I., Chassany O., Grenard AS., Caulin C., Bergmann JF. Defining the role of calcium channel antagonists in heart failure due to systolic dysfunction. Am J Cardiovasc Drugs 2003; 3(1): 33-41. Doi: 10.2165/00129784-200303010-00004.
Masarone D., Limongelli G., Rubino M., Valente F., Vastarella R., Ammendola E., Gravino R., Verrengia M., Salerno G., Pacileo G. Management of Arrhythmias in Heart Failure. J Cardiovasc Dev Dis 2017; 4(1): 3. Doi: 10.3390/jcdd4010003.
Podrid P., Lown B. Selection of an antiarrhythmic drug to protect against ventricular fibrillation. In Proceedings of the first US-USSR Symposium on Sudden Death. DHEW publ. no. (NIH) 1978. 259-278.
Mason JW. A comparison of seven antiarrhythmic drugs in patients with ventricular tachyarrhythmias. Electrophysiologic Study versus Electrocardiographic Monitoring Investigators. N Engl J Med 1993; 329(7): 452-8. Doi: 10.1056/NEJM199308123290702.
Aiba T., Kurita T., Taguchi A., Shimizu W., Suyama K., Aihara N., Kamakura S.. Long-term efficacy of empirical chronic amiodarone therapy in patients with sustained ventricular tachyarrhythmia and structural heart disease. Circ J 2002; 66(4): 367-71. Doi: 10.1253/circj.66.367.
Bokhari F., Newman D., Greene M., Korley V., Mangat I., Dorian P. Long-term comparison of the implantable cardioverter defibrillator versus amiodarone: eleven-year follow-up of a subset of patients in the Canadian Implantable Defibrillator Study (CIDS). Circulation 2004; 110(2): 112-6. Doi: 10.1161/01.CIR.0000134957.51747.6E.
Sobiech M., Lewandowski M., Zając D., Maciąg A., Syska P., Ateńska-Pawłowska J., Kowalik I., Sterliński M., Szwed H., Pytkowski M. Efficacy and tolerability of mexiletine treatment in patients with recurrent ventricular tachyarrhythmias and implantable cardioverter-defibrillator shocks. Kardiol Pol 2017; 75(10): 1027-1032. Doi: 10.5603/KP.2017.0189.
AbdelWahab A., Sapp J. Ventricular Tachycardia with ICD Shocks: When to Medicate and When to Ablate. Curr Cardiol Rep 2017; 19(11): 105. Doi: 10.1007/s11886-017-0924-0.
Sapp JL., Wells GA., Parkash R., Stevenson WG., Blier L., Sarrazin JF., Thibault B., Rivard L., Gula L., Leong-Sit P., et al. Ventricular Tachycardia Ablation versus Escalation of Antiarrhythmic Drugs. N Engl J Med 2016; 375(2): 111-21. Doi: 10.1056/NEJMoa1513614.
Deyell MW., Steinberg C., Doucette S., Parkash R., Nault I., Gray C., Essebag V., Gardner M., Sterns LD., Healey JS., et al. Mexiletine or catheter ablation after amiodarone failure in the VANISH trial. J Cardiovasc Electrophysiol 2018; 29(4): 603-608. Doi: 10.1111/jce.13431.
Gao D., Van Herendael H., Alshengeiti L., Dorian P., Mangat I., Korley V., Ahmad K., Golovchiner G., Aves T., Pinter A. Mexiletine as an adjunctive therapy to amiodarone reduces the frequency of ventricular tachyarrhythmia events in patients with an implantable defibrillator. J Cardiovasc Pharmacol 2013; 62(2): 199-204. Doi: 10.1097/FJC.0b013e31829651fe.
Kavey RE., Blackman MS., Sondheimer HM. Phenytoin therapy for ventricular arrhythmias occurring late after surgery for congenital heart disease. Am Heart J 1982;104(4 Pt 1): 794-8. Doi: 10.1016/0002-8703(82)90013-8.
Epstein A. E., Plumb VJ., Henthorn RW., Waldo AL. Phenytoin in the treatment of inducible ventricular tachycardia: results of electrophysiologic testing and long-term follow-up. Pacing Clin Electrophysiol 1987; 10(5): 1049-57. Doi: 10.1111/j.1540-8159.1987.tb06124.x.
Fogoros RN., Fiedler SB., Elson JJ. Efficacy of phenytoin in suppressing inducible ventricular tachyarrhythmias. Cardiovasc Drugs Ther 1988; 2(2): 171-176. Doi: 10.1007/BF00051232.
Ruwald MH., Solomon SD., Foster E., Kutyifa V., et al. Left ventricular ejection fraction normalization in cardiac resynchronization therapy and risk of ventricular arrhythmias and clinical outcomes: results from the Multicenter Automatic Defibrillator Implantation Trial with Cardiac Resynchronization Therapy (MADIT-CRT) trial. Circulation 2014; 130(25): 2278-86. Doi: 10.1161/CIRCULATIONAHA.114.011283
El-Sherif N., Turitto G. Electrolyte disorders and arrhythmogenesis. Journal of Cardiology 2011; 18(3): 233-45.
Conolly SJ., Gent M., Roberts RS., et al. Canadian Implantable Defibrillator Study (CIDS): a randomized trial of the implantable cardioverter defibrillator against amiodarone. Circulation 2000; 101(11): 1297-1302. Doi: 10.1161/01.cir.101.11.1297.
Tanner H., Hindricks G., Volkmer M., et al. Catheter ablation of recurrent scar-related ventricular tachycardia using electroanatomical mapping and irrigated ablation technology: results of the prospective multicenter Euro-VT-study. Journal of Cardiovascular Electrophysiology 2010; 21(1): 47-53. Doi: 10.1111/j.1540-8167.2009.01563.x.
Hohnloser SH., Kuck KH., Dorian P., et al. On behalf of the DINAMIT investigators. Prophylactic use of an implantable cardioverter-defibrillator after acute myocardial infarction. The New England Journal of Medicine 2004; 351(24): 2481-2488. Doi: 10.1056/NEJMoa041489.
Steinbeck G., Andresen D., Seidl K. Defibrillator Implantation Early after Myocardial Infarction. Immediate Risk-Stratification Improves Survival (IRIS). The New England Journal of Medicine 2009; 361: 1427-1436. Doi: 10.1056/NEJMoa0901889.
Moss AJ., Hall WJ., Cannom DS., et al. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. The New England Journal of Medicine 1996; 335(26): 1933-1940. Doi: 10.1056/NEJM199612263352601.
Buxton AE., Lee KL., Fisher JD., et al. A randomized study of the prevention of sudden death in patients with coronary artery disease. Multicenter Unsustained Tachycardia Trial Investigators. The New England Journal of Medicine 1999; 341(25): 1882-1890. Doi: 10.1056/NEJM199912163412503.
Moss AJ., Zareba W., Hall WJ., et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. The New England Journal of Medicine 2002; 346(12): 877-883. Doi: 10.1056/NEJMoa013474.
Bristow MR., Saxon LA., Boehmer J., et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. The New England Journal of Medicine 2004; 350(21): 2140-2150. Doi: 10.1056/NEJMoa032423.
Bigger JT. Prophylactic use of implanted cardiac defibrillators in patients at risk for ventricular arrhythmias after coronary artery bypass graft surgery (Coronary Artery Bypass Graft (CABG) Patch Trial Investigators). The New England Journal of Medicine 1997; 337(22): 1569-1575. Doi: 10.1056/NEJM199711273372201.
Køber L., Thune JJ., Nielsen JC., et al. Defibrillator Implantation in Patients with Nonischemic Systolic Heart Failure. Danish Study to Assess the Efficacy of ICDs in Patients with Non-ischemic Systolic Heart Failure on Mortality (DANISH). The New England Journal of Medicine 2016; 375(13): 1221-1230. Doi: 10.1056/NEJMoa1608029.
Bänsch D., Antz M., Boczor S., et al. Primary Prevention of Sudden Cardiac Death in Idiopathic Dilated Cardiomyopathy The Cardiomyopathy Trial (CAT). Circulation 2002; 105(12): 1453-1458. Doi: 10.1161/01.cir.0000012350.99718.ad.
Strickberger SA., Hummel JD., Bartlett TG., et al. Amiodarone Versus Implantable Cardioverter-Defibrillator: Randomized Trial in Patients With Nonischemic Dilated Cardiomyopathy and Asymptomatic Nonsustained Ventricular Tachycardia–AMIOVIRT. Journal of the American College of Cardiology 2003; 41(10): 1707-1712. Doi: 10.1016/s0735-1097(03)00297-3.
Kadish A., Dyer A., Daubert JP., Quigg R., Estes NA., Anderson KP., Calkins H., Hoch D., Goldberger J., Shalaby A., et al. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med 2004; 350(21): 2151-8. Doi: 10.1056/NEJMoa033088.
Desai AS., Fang JC., Maisel WH., Baughman KL. Implantable defibrillators for the prevention of mortality in patients with nonischemic cardiomyopathy: a meta-analysis of randomized controlled trials. JAMA 2004; 292(23): 2874-9. Doi: 10.1001/jama.292.23.2874.
Algalarrondo V., Perault R., Bories MC., Narayanan K., Garcia R., Combes N., Perier MC., Defaye P., Sadoul N., Gras D., et al. Prophylactic implantable cardioverter defibrillators for primary prevention: From implantation to heart transplantation. Arch Cardiovasc Dis 2018; 111(12): 758-765. Doi: 10.1016/j.acvd.2018.05.004.
Sandner SE., Wieselthaler G., Zuckermann A., Taghavi S., Schmidinger H., Pacher R., Ploner M., Laufer G., Wolner E., Grimm M. Survival benefit of the implantable cardioverter-defibrillator in patients on the waiting list for cardiac transplantation. Circulation 2001; 104(12 Suppl 1): I171-6. Doi: 10.1161/hc37t1.094916.
Cleland JG., Daubert JC., Erdmann E., Freemantle N., Gras D., Kappenberger L., Klein W., Tavazzi L.; CARE-HF study Steering Committee and Investigators. The CARE-HF study (CArdiac REsynchronisation in Heart Failure study): rationale, design and end-points. Eur J Heart Fail 2001; 3(4): 481-9. Doi: 10.1016/s1388-9842(01)00176-3.
Tang AS., Wells GA., Talajic M., Arnold MO., Sheldon R., Connolly S., Hohnloser SH., Nichol G., Birnie DH., Sapp JL., et al. Cardiac-resynchronization therapy for mild-to-moderate heart failure. N Engl J Med 2010 ;363(25): 2385-95. Doi: 10.1056/NEJMoa1009540.
Eickholt C., Siekiera M., Kirmanoglou K., Rodenbeck A., Heussen N., Schauerte P., Lichtenberg A., Balzer J., Rassaf T., Perings S., Kelm M., et al. Improvement of left ventricular function under cardiac resynchronization therapy goes along with a reduced incidence of ventricular arrhythmia. PLoS One 2012; 7(11): e48926. Doi: 10.1371/journal.pone.0048926.
Young JB., Abraham WT., Smith AL., Leon AR., Lieberman R., Wilkoff B., Canby RC., Schroeder JS., Liem LB., Hall S., et al. Combined cardiac resynchronization and implantable cardioversion defibrillation in advanced chronic heart failure: the MIRACLE ICD Trial. JAMA 2003; 289(20): 2685-94. Doi: 10.1001/jama.289.20.2685.
Bradley DJ., Bradley EA., Baughman KL., Berger RD., Calkins H., Goodman SN., Kass DA., Powe NR. Cardiac resynchronization and death from progressive heart failure: a meta-analysis of randomized controlled trials. JAMA 2003; 289(6): 730-40. Doi: 10.1001/jama.289.6.730.
McAlister FA., Ezekowitz JA., Wiebe N., Rowe B., Spooner C., Crumley E., Hartling L., Klassen T., Abraham W. Systematic review: cardiac resynchronization in patients with symptomatic heart failure. Ann Intern Med 2004; 141(5): 381-90. Doi: 10.7326/0003-4819-141-5-200409070-00101.
Cleland JG., Coletta AP., Lammiman M., Witte KK., Loh H., Nasir M., Clark AL. Clinical trials update from the European Society of Cardiology meeting 2005: CARE-HF extension study, ESSENTIAL, CIBIS-III, S-ICD, ISSUE-2, STRIDE-2, SOFA, IMAGINE, PREAMI, SIRIUS-II and ACTIVE. Eur J Heart Fail 2005; 7(6): 1070-5. Doi: 10.1016/j.ejheart.2005.09.006.
Cleland JG., Daubert JC., Erdmann E.., Freemantle N, Gras D., Kappenberger L., Tavazzi L. Longer-term effects of cardiac resynchronization therapy on mortality in heart failure [the CArdiac REsynchronization-Heart Failure (CARE-HF) trial extension phase]. Eur Heart J 2006; 27(16): 1928-32. Doi: 10.1093/eurheartj/ehl099.
Daubert C., Gold MR., Abraham WT., Ghio S., Hassager C., Goode G., Szili-Török T., Linde C.; REVERSE Study Group. Prevention of disease progression by cardiac resynchronization therapy in patients with asymptomatic or mildly symptomatic left ventricular dysfunction: insights from the European cohort of the REVERSE (Resynchronization Reverses Remodeling in Systolic Left Ventricular Dysfunction) trial. J Am Coll Cardiol 2009; 54(20): 1837-46. Doi: 10.1016/j.jacc.2009.08.011.
Linde C., Gold MR., Abraham WT., St John Sutton M., Ghio S., Cerkvenik J., Daubert C; REsynchronization reVErses Remodeling in Systolic left vEntricular dysfunction Study Group. Long-term impact of cardiac resynchronization therapy in mild heart failure: 5-year results from the REsynchronization reVErses Remodeling in Systolic left vEntricular dysfunction (REVERSE) study. Eur Heart J 2013; 34(33): 2592-9. Doi: 10.1093/eurheartj/eht160.
Cleland JG., Abraham WT., Linde C., Gold MR., Young JB., Claude Daubert J., Sherfesee L., Wells GA., Tang AS. An individual patient meta-analysis of five randomized trials assessing the effects of cardiac resynchronization therapy on morbidity and mortality in patients with symptomatic heart failure. Eur Heart J 2013; 34(46): 3547-56. Doi: 10.1093/eurheartj/eht290
Woods B., Hawkins N., Mealing S., Sutton A., Abraham WT., Beshai JF., Klein H., Sculpher M., Plummer CJ., Cowie MR. Individual patient data network meta-analysis of mortality effects of implantable cardiac devices. Heart 2015; 101(22): 1800-6. Doi: 10.1136/heartjnl-2015-307634.
Steffel J., Robertson M., Singh JP., Abraham WT., Bax JJ., Borer JS., Dickstein K., Ford I., Gorcsan J 3rd., Gras D., et al. The effect of QRS duration on cardiac resynchronization therapy in patients with a narrow QRS complex: a subgroup analysis of the EchoCRT trial. Eur Heart J 2015; 36(30): 1983-9. Doi: 10.1093/eurheartj/ehv242.
Jacobsson J., Reitan C., Carlson J., Borgquist R., Platonov PG. Atrial fibrillation incidence and impact of biventricular pacing on long-term outcome in patients with heart failure treated with cardiac resynchronization therapy. BMC Cardiovasc Disord 2019; 19(1): 195. Doi: 10.1186/s12872-019-1169-1.
Healey JS., Hohnloser SH., Exner DV., Birnie DH., Parkash R., Connolly SJ., Krahn AD., Simpson CS., Thibault B., Basta M., et al. RAFT Investigators. Cardiac resynchronization therapy in patients with permanent atrial fibrillation: results from the Resynchronization for Ambulatory Heart Failure Trial (RAFT). Circ Heart Fail 2012; 5(5): 566-70. Doi: 10.1161/CIRCHEARTFAILURE.
Lopes C., Pereira T., Barra S. Cardiac resynchronization therapy in patients with atrial fibrillation: a meta-analysis. Rev Port Cardiol 2014; 33(11): 717-25. Doi: 10.1016/j.repc.2014.05.008.
Gasparini M., Leclercq C., Lunati M., Landolina M., Auricchio A., Santini M., Boriani G., Lamp B., Proclemer A., Curnis A., et al. Cardiac resynchronization therapy in patients with atrial fibrillation: the CERTIFY study (Cardiac Resynchronization Therapy in Atrial Fibrillation Patients Multinational Registry). JACC Heart Fail 2013; 1(6): 500-7. Doi: 10.1016/j.jchf.2013.06.003.
Upadhyay GA., Choudhry NK., Auricchio A., Ruskin J., Singh JP. Cardiac resynchronization in patients with atrial fibrillation: a meta-analysis of prospective cohort studies. J Am Coll Cardiol 2008; 52(15): 1239-46. Doi: 10.1016/j.jacc.2008.06.043.
Gasparini M., Auricchio A., Regoli F., Fantoni C., Kawabata M., Galimberti P., Pini D., Ceriotti C., Gronda E., Klersy C., et al. Four-year efficacy of cardiac resynchronization therapy on exercise tolerance and disease progression: the importance of performing atrioventricular junction ablation in patients with atrial fibrillation. J Am Coll Cardiol 2006; 48(4): 734-43. Doi: 10.1016/j.jacc.2006.03.056.
Ferreira AM., Adragão P., Cavaco DM., Candeias R., Morgado FB., Santos KR., Santos E., Silva JA. Benefit of cardiac resynchronization therapy in atrial fibrillation patients vs. patients in sinus rhythm: the role of atrioventricular junction ablation. Europace 2008; 10(7): 809-15. Doi: 10.1093/europace/eun135.
Orlov MV., Gardin JM., Slawsky M., Bess RL., Cohen G., Bailey W., Plumb V., Flathmann H., de Metz K. Biventricular pacing improves cardiac function and prevents further left atrial remodeling in patients with symptomatic atrial fibrillation after atrioventricular node ablation. Am Heart J 2010; 159(2): 264-70. Doi: 10.1016/j.ahj.2009.11.012.
Doshi RN., Daoud EG., Fellows C., Turk K., Duran A., Hamdan MH., Pires LA. PAVE Study Group. Left ventricular-based cardiac stimulation post AV nodal ablation evaluation (the PAVE study). J Cardiovasc Electrophysiol 2005; 16(11): 1160-5. Doi: 10.1111/j.1540-8167.2005.50062.x.
Brignole M., Gammage M., Puggioni E., Alboni P., Raviele A., Sutton R., Vardas P., Bongiorni MG., Bergfeldt L., Menozzi C., Musso G. Optimal Pacing SITE (OPSITE) Study Investigators. Comparative assessment of right, left, and biventricular pacing in patients with permanent atrial fibrillation. Eur Heart J 2005; 26(7): 712-22. Doi: 10.1093/eurheartj/ehi069.
Brignole M., Botto GL., Mont L., Oddone D., Iacopino S., De Marchi G., Campoli M., Sebastiani V., Vincenti A., Garcia Medina D., et al. Predictors of clinical efficacy of 'Ablate and Pace' therapy in patients with permanent atrial fibrillation. Heart 2012; 98(4): 297-302. Doi: 10.1136/heartjnl-2011-301069.
Leclercq C., Cazeau S., Lellouche D., Fossati F., Anselme F., Davy JM., Sadoul N., Klug D., Mollo L., Daubert JC. Upgrading from single chamber right ventricular to biventricular pacing in permanently paced patients with worsening heart failure: The RD-CHF Study. Pacing Clin Electrophysiol 2007; 30 Suppl 1: S23-30. Doi: 10.1111/j.1540-8159.2007.00598.x.
Höijer CJ., Meurling C., Brandt J. Upgrade to biventricular pacing in patients with conventional pacemakers and heart failure: a double-blind, randomized crossover study. Europace 2006; 8(1): 51-5. Doi: 10.1093/europace/euj014.
van Geldorp IE., Vernooy K., Delhaas T., Prins MH., Crijns HJ., Prinzen FW., Dijkman B. Beneficial effects of biventricular pacing in chronically right ventricular paced patients with mild cardiomyopathy. Europace 2010; 12(2): 223-9. Doi: 10.1093/europace/eup378.
Laurenzi F., Achilli A., Avella A., Peraldo C., Orazi S., Perego GB., Cesario A., Valsecchi S., De Santo T., Puglisi A., et al. Biventricular upgrading in patients with conventional pacing system and congestive heart failure: results and response predictors. Pacing Clin Electrophysiol 2007; 30(9): 1096-104. Doi: 10.1111/j.1540-8159.2007.00819.x.
Vatankulu MA., Goktekin O., Kaya MG., Ayhan S., Kucukdurmaz Z., Sutton R., Henein M. Effect of long-term resynchronization therapy on left ventricular remodeling in pacemaker patients upgraded to biventricular devices. Am J Cardiol 2009; 103(9): 1280-4. Doi: 10.1016/j.amjcard.2009.01.023.
Foley PW., Muhyaldeen SA., Chalil S., Smith RE., Sanderson JE., Leyva F. Long-term effects of upgrading from right ventricular pacing to cardiac resynchronization therapy in patients with heart failure. Europace 2009; 11(4): 495-501. Doi: 10.1093/europace/eup037.
Paparella G., Sciarra L., Capulzini L., Francesconi A., et al. Long-term effects of upgrading to biventricular pacing: differences with cardiac resynchronization therapy as primary indicationю Pacing Clinical Electrophysiology 2010; 33(7): 841-849. Doi: 10.1111/j.1540-8159.2010.02701.x.
Gage RM., Burns KV., Bank AJ. Echocardiographic and clinical response to cardiac resynchronization therapy in heart failure patients with and without previous right ventricular pacing. European Journal of Heart Failure 2014; 16(11): 1199-1205. Doi: 10.1002/ejhf.143.
Bardy G.H., Smith WM., Hood MA. et al. An entirely subcutaneous implantable cardioverter-defibrillator. The New England Journal of Medicine 2010; 363(1): 36-44. Doi: 10.1056/NEJMoa0909545.
Weiss R., Knight BP., Gold MR., Leon AR., et al. Safety and efficacy of a totally subcutaneous implantable-cardioverter defibrillator. Circulation 2013; 128(9): 944-953. Doi: 10.1161/CIRCULATIONAHA.113.003042.
Jarman JW., Lascelles K., Wong T., et al. Clinical experience of entirely subcutaneous implantable cardioverter-defibrillators in children and adults: cause for caution. European Heart Journal 2012; 33(11): 1351-1359. Doi: 10.1093/eurheartj/ehs017.
Dabiri Abkenari L., Theuns DA., Valk SD., et al. Clinical experience with a novel subcutaneous implantable defibrillator system in a single center. Clinical Research in Cardiology 2011; 100(9): 737-44. Doi: 10.1007/s00392-011-0303-6.
Burke MC., Gold MR., Knight BP., et al. Safety and efficacy of the totally subcutaneous implantable defibrillator: 2-year results from a pooled analysis of the IDE Study and EFFORTLESS Registry. Journal of the American College of Cardiology 2015; 65(16): 1605-1615. Doi: 10.1016/j.jacc.2015.02.047.
Lambiase PD., Barr C., Theuns DA. et al. Worldwide experience with a totally subcutaneous implantable defibrillator: early results from the EFFORTLESS S-ICD Registry. European Heart Journal 2014; 35(25): 1657-1665. Doi: 10.1093/eurheartj/ehu112.
Irvine J., Dorian P., Baker B., et al. Quality of life in the Canadian Implantable Defibrillator Study (CIDS). American Heart Journal 2002 Aug;144(2):282-9. Doi: 10.1067/mhj.2002.124049.
Tomzik J., Koltermann KC., Zabel M., et. Al. Quality of Life in Patients with an Implantable Cardioverter Defibrillator: A Systematic Review. Frontiers in Cardiovascular Medicine 2015; 2: 34. Doi: 10.3389/fcvm.2015.00034.
Schron EB., Exner DV., Yao Q., et. Al. Quality of life in the antiarrhythmics versus implantable defibrillators trial impact of therapy and influence of adverse symptoms and defibrillator shocks. Circulation 2002; 105(5): 589-594. Doi: 10.1161/hc0502.103330.
Koopman HM., Vrijmoet-Wiersma CM., Langius JN., et al. Psychological functioning and disease-related quality of life in pediatric patients with an implantable cardioverter defibrillator. Pediatric Cardiology 2012; 33(4): 569-575. Doi: 10.1007/s00246-012-0175-1.
Padeletti L., Arnar DO., Boncinelli L. et al. EHRA Expert Consensus Statement on the management of cardiovascular implantable electronic devices in patients nearing end of life or requesting withdrawal of therapy. Europace 2010; 12(10): 1480-1489. Doi: 10.1093/europace/euq275.
Jaarsma T., Beattie JM., Ryder M., Rutten FH., et al. Palliative care in heart failure: a position statement from the palliative care workshop of the Heart Failure Association of the European Society of Cardiology. European Journal of Heart Failure 2009; 11(5): 433-443. Doi: 10.1093/eurjhf/hfp041.
Scott PA., Silberbauer J., McDonagh TA., Murgatroyd FD. Impact of prolonged implantable cardioverter-defibrillator arrhythmia detection times on outcomes: a meta-analysis. Heart Rhythm 2014; 11(5): 828-835. Doi: 10.1016/j.hrthm.2014.02.009.
Tan VH., Wilton SB., Kuriachan V., et al. Impact of programming strategies aimed at reducing nonessential implantable cardioverter defibrillator therapies on mortality: a systematic review and meta-analysis. Circulation: Arrhythmia and Electrophysiology 2014; 7(1): 164-170. Doi: 10.1161/CIRCEP.113.001217.
Saeed M., Hanna I., Robotis D., Styperek R., Polosajian L., Khan A., Alonso J., Nabutovsky Y., Neason C. Programming implantable cardioverter-defibrillators in patients with primary prevention indication to prolong time to first shock: results from the PROVIDE study. J Cardiovasc Electrophysiol 2014; 25(1): 52-9. Doi: 10.1111/jce.12273.
Wathen MS., DeGroot PJ., Sweeney MO., Stark AJ., Otterness MF., Adkisson WO., Canby RC., Khalighi K., Machado C., Rubenstein DS., et al. Prospective randomized multicenter trial of empirical antitachycardia pacing versus shocks for spontaneous rapid ventricular tachycardia in patients with implantable cardioverter-defibrillators: Pacing Fast Ventricular Tachycardia Reduces Shock Therapies (PainFREE Rx II) trial results. Circulation 2004; 110(17): 2591-6. Doi: 10.1161/01.CIR.0000145610.64014.E4.
Sweeney MO., Wathen MS., Volosin K., Abdalla I., DeGroot PJ., Otterness MF., Stark AJ. Appropriate and inappropriate ventricular therapies, quality of life, and mortality among primary and secondary prevention implantable cardioverter defibrillator patients: results from the Pacing Fast VT REduces Shock ThErapies (PainFREE Rx II) trial. Circulation 2005; 111(22): 2898-905. Doi: 10.1161/CIRCULATIONAHA.104.526673.
Borne RT., Varosy PD., Masoudi FA. Implantable cardioverter-defibrillator shocks: epidemiology, outcomes, and therapeutic approaches. JAMA Intern Med 2013; 173(10): 859-65. Doi: 10.1001/jamainternmed.2013.428.
Berg SK., Higgins M., Reilly CM., Langberg JJ., Dunbar SB. Sleep quality and sleepiness in persons with implantable cardioverter defibrillators: outcome from a clinical randomized longitudinal trial. Pacing Clin Electrophysiol 2012; 35(4): 431-43. Doi: 10.1111/j.1540-8159.2011.03328.x.
Barsheshet A., Moss AJ., McNitt S., Jons C., Glikson M., Klein HU., Huang DT., Steinberg JS., Brown MW., Zareba W., et al. Long-term implications of cumulative right ventricular pacing among patients with an implantable cardioverter-defibrillator. Heart Rhythm 2011; 8(2): 212-8. Doi: 10.1016/j.hrthm.2010.10.035.
Wilkoff BL., Cook JR., Epstein AE., Greene HL., Hallstrom AP., Hsia H., Kutalek SP., Sharma A.; Dual Chamber and VVI Implantable Defibrillator Trial Investigators. Dual-chamber pacing or ventricular backup pacing in patients with an implantable defibrillator: the Dual Chamber and VVI Implantable Defibrillator (DAVID) Trial. JAMA 2002; 288(24): 3115-23. Doi: 10.1001/jama.288.24.3115.
Olshansky B., Day JD., Moore S., Gering L., Rosenbaum M., McGuire M., Brown S., Lerew DR. Is dual-chamber programming inferior to single-chamber programming in an implantable cardioverter-defibrillator? Results of the INTRINSIC RV (Inhibition of Unnecessary RV Pacing With AVSH in ICDs) study. Circulation 2007; 115(1): 9-16. Doi: 10.1161/CIRCULATIONAHA.106.629428.
Gasparini M., Proclemer A., Klersy C., Kloppe A., Lunati M., Ferrer JB., Hersi A., Gulaj M., Wijfels MC., Santi E., et al. Effect of long-detection interval vs standard-detection interval for implantable cardioverter-defibrillators on antitachycardia pacing and shock delivery: the ADVANCE III randomized clinical trial. JAMA 2013; 309(18): 1903-11. Doi: 10.1001/jama.2013.4598.
Moss AJ., Schuger C., Beck CA., Brown MW., Cannom DS., Daubert JP., Estes NA 3rd., Greenberg H., Hall WJ., Huang DT., et al. Reduction in inappropriate therapy and mortality through ICD programming. N Engl J Med. 2012 Dec 13;367(24):2275-83. Doi: 10.1056/NEJMoa1211107.
Wilkoff BL., Williamson BD., Stern RS., Moore SL., Lu F., Lee SW., Birgersdotter-Green UM., Wathen MS., Van Gelder IC., Heubner BM., et al. Strategic programming of detection and therapy parameters in implantable cardioverter-defibrillators reduces shocks in primary prevention patients: results from the PREPARE (Primary Prevention Parameters Evaluation) study. J Am Coll Cardiol 2008; 52(7): 541-50. Doi: 10.1016/j.jacc.2008.05.011.
Ploux S., Swerdlow CD., Strik M., Welte N., Klotz N., Ritter P., Haïssaguerre M., Bordachar P. Towards eradication of inappropriate therapies for ICD lead failure by combining comprehensive remote monitoring and lead noise alerts. J Cardiovasc Electrophysiol 2018; 29(8): 1125-1134. Doi: 10.1111/jce.13653.
Ellenbogen KA., Gunderson BD., Stromberg KD., Swerdlow CD. Performance of Lead Integrity Alert to assist in the clinical diagnosis of implantable cardioverter defibrillator lead failures: analysis of different implantable cardioverter defibrillator leads. Circ Arrhythm Electrophysiol 2013; 6(6): 1169-77. Doi: 10.1161/CIRCEP.113.000744.
Swerdlow CD., Gunderson BD., Ousdigian KT., Abeyratne A., Sachanandani H., Ellenbogen KA. Downloadable software algorithm reduces inappropriate shocks caused by implantable cardioverter-defibrillator lead fractures: a prospective study. Circulation 2010; 122(15): 1449-55. Doi: 10.1161/CIRCULATIONAHA.110.962407.
Guédon-Moreau L., Kouakam C., Klug D., Marquié C., Brigadeau F., Boulé S., Blangy H., Lacroix D., Clémenty J., Sadoul N., et al. Decreased delivery of inappropriate shocks achieved by remote monitoring of ICD: a substudy of the ECOST trial. J Cardiovasc Electrophysiol 2014; 25(7): 763-70. Doi: 10.1111/jce.12405.
Gulizia MM., Piraino L., Scherillo M., Puntrello C., Vasco C, Scianaro MC., Mascia F., Pensabene O., Giglia S., Chiarandà G., et al. A randomized study to compare ramp versus burst antitachycardia pacing therapies to treat fast ventricular tachyarrhythmias in patients with implantable cardioverter defibrillators: the PITAGORA ICD trial. Circ Arrhythm Electrophysiol 2009; 2(2): 146-53. Doi: 10.1161/CIRCEP.108.804211.
Gold MR., Weiss R., Theuns DA., Smith W., Leon A., Knight BP., Carter N., Husby M., Burke MC. Use of a discrimination algorithm to reduce inappropriate shocks with a subcutaneous implantable cardioverter-defibrillator. Heart Rhythm 2014; 11(8): 1352-8. Doi: 10.1016/j.hrthm.2014.04.012.
Mesquita J., Cavaco D., Ferreira A., Lopes N., Santos PG., Carvalho MS., Haas A., Costa F., Carmo P., Morgado F., et al. Effectiveness of subcutaneous implantable cardioverter-defibrillators and determinants of inappropriate shock delivery. Int J Cardiol 2017; 232: 176-180. Doi: 10.1016/j.ijcard.2017.01.034.
Gold MR., Lambiase PD., El-Chami MF., Knops RE., Aasbo JD., Bongiorni MG., Russo AM., Deharo JC., Burke MC., Dinerman J., et al. Primary Results From the Understanding Outcomes With the S-ICD in Primary Prevention Patients With Low Ejection Fraction (UNTOUCHED) Trial. Circulation 2021; 143(1): 7-17. Doi: 10.1161/CIRCULATIONAHA.120.048728.
Gilliam FR., Hayes DL., Boehmer JP., Day J., Heidenreich PA., Seth M., Jones PW., Stein KM., Saxon LA. Real world evaluation of dual-zone ICD and CRT-D programming compared to single-zone programming: the ALTITUDE REDUCES study. J Cardiovasc Electrophysiol 2011; 22(9): 1023-9. Doi: 10.1111/j.1540-8167.2011.02086.x.
Silka MJ., Shah MJ., Silva JNA., Balaji S., Beach CM., Benjamin MN., Berul CI., Cannon B., Cecchin F., Cohen MI., et al. 2021 PACES Expert Consensus Statement on the Indications and Management of Cardiovascular Implantable Electronic Devices in Pediatric Patients: Executive Summary. Heart Rhythm; 18(11): 1925-1950. Doi: 10.1016/j.hrthm.2021.07.051.
Приложение к приказу об организации оказания паллиативной медицинской помощи, включая порядок взаимодействия медицинских организаций, организаций социального обслуживания и общественных объединений, иных некоммерческих организаций, осуществляющих свою деятельность в сфере охраны здоровья, утвержденному приказом Министерства здравоохранения Российской Федерации и Министерства труда и социальной защиты Российской Федерации от 31 мая 2019г.: № 345н/372н.
Hupcey JE., Kitko L., Alonso W. Patients' Perceptions of Illness Severity in Advanced Heart Failure. J Hosp Palliat Nurs 2016; 18(2): 110-114. Doi: 10.1097/NJH.0000000000000229.
Tsutsui H., Isobe M., Ito H., Ito H., Okumura K., Ono M., Kitakaze M., Kinugawa K., Kihara Y., Goto Y., et al. Japanese Circulation Society and the Japanese Heart Failure Society Joint Working Group. JCS 2017/JHFS 2017 Guideline on Diagnosis and Treatment of Acute and Chronic Heart Failure - Digest Version. Circ J 2019; 83(10) :2084-2184. Doi: 10.1253/circj.CJ-19-0342.
Lewis WR., Luebke DL., Johnson NJ., Harrington MD., Costantini O., Aulisio MP. Withdrawing implantable defibrillator shock therapy in terminally ill patients. Am J Med 2006; 119(10): 892-6. Doi: 10.1016/j.amjmed.2006.01.017.
Goldstein NE., Lampert R., Bradley E., Lynn J., Krumholz HM. Management of implantable cardioverter defibrillators in end-of-life care. Ann Intern Med 2004; 141(11): 835-8. Doi: 10.7326/0003-4819-141-11-200412070-00006.
Kinch Westerdahl A., Sjöblom J., Mattiasson AC., Rosenqvist M., Frykman V. Implantable cardioverter-defibrillator therapy before death: high risk for painful shocks at end of life. Circulation 2014; 129(4): 422-9. Doi: 10.1161/CIRCULATIONAHA.113.002648.
Brady DR. Planning for Deactivation of Implantable Cardioverter Defibrillators at the End of Life in Patients With Heart Failure. Crit Care Nurse 2016; 36(6): 24-31. Doi: 10.4037/ccn2016362.
Ferrell BR, Twaddle ML, Melnick A, Meier DE. National Consensus Project Clinical Practice Guidelines for Quality Palliative Care Guidelines, 4th Edition. J Palliat Med. 2018 Dec;21(12):1684-1689.
Greater Manchester and Eastern Cheshire Strategic Clinical Networks. Palliative care pain & symptom control guidelines for adults. 5th ed. [Manchester]: Greater Manchester and Eastern Cheshire Strategic Clinical Networks; 2019.
Stoevelaar R., Brinkman-Stoppelenburg A., van Driel AG., Theuns DA., Bhagwandien RE., van Bruchem-Visser RL., Lokker IE., van der Heide A., Rietjens JA. Trends in time in the management of the implantable cardioverter defibrillator in the last phase of life: a retrospective study of medical records. Eur J Cardiovasc Nurs 2019; 18(6): 449-457. Doi: 10.1177/1474515119844660.
Crespo-Leiro MG., Metra M., Lund LH., Milicic D., Costanzo MR., Filippatos G., Gustafsson F., Tsui S., Barge-Caballero E., De Jonge N., et al. Advanced heart failure: a position statement of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 2018; 20(11): 1505-1535. Doi: 10.1002/ejhf.1236.
Kida K., Doi S., Suzuki N. Palliative Care in Patients with Advanced Heart Failure. Heart Fail Clin 2020; 16(2): 243-254. Doi: 10.1016/j.hfc.2019.12.006.
Lowey SE. Palliative Care in the Management of Patients with Advanced Heart Failure. Adv Exp Med Biol 2018; 1067: 295-311. Doi: 10.1007/5584_2017_115.
Гасымова Н.З., Шабанов В.В., Сафонов Н.В., Рзаев Ф.Г., Филатов А.Г., Рогалев П.В., Кропоткин Е.Б., Михайлов Е.Н. Многоконтактное картирование в лечении различных нарушений ритма сердца. Вестник аритмологии 2024; 31(1): 110-122. Doi: 10.35336/VA-1297.
Philip Saul J., et al. PACES/HRS expert consensus statement on the use of catheter ablation in children and patients with congenital heart disease. Heart Rhythm 2016; 13(6): e251-89. Doi: 10.1016/j.hrthm.2016.02.009.
Crosson JE., Callans DJ., Bradley DJ., Dubin A., Epstein M., Etheridge S., Papez A., Phillips JR., Rhodes LA., Saul P., Stephenson E., Stevenson W., Zimmerman F. PACES/HRS expert consensus statement on the evaluation and management of ventricular arrhythmias in the child with a structurally normal heart. Heart Rhythm. 2014; 11(9): e55-78. Doi: 10.1016/j.hrthm.2014.05.010.
Latchamsetty R., Bogun F. Premature Ventricular Complexes and Premature Ventricular Complex Induced Cardiomyopathy. Current Problems in Cardiology 2015; 40(9): 379-422. Doi: 10.1016/j.cpcardiol.2015.03.002.
Daniels DV., Lu YY., Morton JB., Santucci PA., et al Idiopathic epicardial left ventricular tachycardia originating remote from the sinus of Valsalva: electrophysiological characteristics, catheter ablation, and identification from the 12-1ead electrocardiogram. Circulation. 2006; 113(13): 1659-1666. Doi: 10.1161/CIRCULATIONAHA.105.611640.
Doppalapudi H., Yamada T., McElderry HT., Plumb VJ., et al. Ventricular tachycardia originating from the posterior papillary muscle in the left ventricle: a distinct clinical syndrome. Circulation: Arrhythmia and Electrophysiology 2008; 1(1): 23-29. Doi: 10.1161/CIRCEP.107.742940.
Sapp JL., Tang ASL., Parkash R., Stevenson WG., Healey JS., Wells G. A randomized clinical trial of catheter ablation and antiarrhythmic drug therapy for suppression of ventricular tachycardia in ischemic cardiomyopathy: The VANISH2 trial. Am. Heart J. 2024; 274: 1-10. Doi: 10.1016/j.ahj.2024.04.009.
Visser CA., Kan G., David GK., Lie KI., et al. Two dimensional echocardiography in the diagnosis of left ventricular thrombus: a prospective study of 67 patients with anatomic validation. Chest 1983; 83(2): 228-232. Doi: 10.1378/chest.83.2.228.
Weinsaft JW., Kim RJ., Ross M., et al. Contrast-enhanced anatomic imaging as compared to contrast-enhanced tissue characterization for detection of left ventricular thrombus. JACC Cardiovascular Imaging 2009; 2(8): 969-979. Doi: 10.1016/j.jcmg.2009.03.017.
Soto-Iglesias D., Acosta J., Penela D., et al. Image-based criteria to identify the presence of epicardial arrhythmogenic substrate in patients with transmural myocardial infarction. Heart Rhythm 2018; 15(6): 814-821. Doi: 10.1016/j.hrthm.2018.02.007.
Reddy VY., Reynolds MR., Neuzil P., et al. Prophylactic catheter ablation for the prevention of defibrillator therapy. The New England Journal of Medicine 2007; 357(26): 2657-2665. Doi: 10.1056/NEJMoa065457.
Kumar S., Baldinger SH., Romero J., et al. Substrate-based ablation versus ablation guided by activation and entrainment mapping for ventricular tachycardia: a systematic review and meta-analysis. Journal of Cardiovascular Electrophysiology 2016; 27(12): 1437-1447. Doi: 10.1111/jce.13088.
Acosta J., Penela D., Andreu D., et al. Multielectrode vs. point-by-point mapping for ventricular tachycardia substrate ablation: a randomized study. Europace 2018; 20(3): 512-519. Doi: 10.1093/europace/euw406.
Berte B., Relan J., Sacher F., et al. Impact of electrode type on mapping of scar-related VT. Journal of Cardiovascular Electrophysiology 2015; 26(11): 1213-1223. Doi: 10.1111/jce.12761.
Yamashita S., Cochet H., Sacher F., et al. Impact of new technologies and approaches for post-myocardial infarction ventricular tachycardia ablation during long-term follow-up. Circulation: Arrhythmia and Electrophysiology 2016; 9(7): e003901. Doi: 10.1161/CIRCEP.116.003901.
Desjardins B., Yokokawa M., Good E., et al. Characteristics of intramural scar in patients with nonischemic cardiomyopathy and relation to intramural ventricular arrhythmias. Circulation: Arrhythmia and Electrophysiology 2013; 6(5): 891-897. Doi: 10.1161/CIRCEP.113.000073.
Deyell MW., Park KM., Han Y., Frankel DS., Dixit S., Cooper JM., Hutchinson MD., Lin D., Garcia F., Bala R., et al. Predictors of recovery of left ventricular dysfunction after ablation of frequent ventricular premature depolarizations. Heart Rhythm 2012; 9(9): 1465-72. Doi: 10.1016/j.hrthm.2012.05.019.
Farré J., Wellens HJ. Philippe Coumel: a founding father of modern arrhythmology. Europace 2004; 6(5): 464-5. Doi: 10.1016/j.eupc.2004.06.001.
Neira V., Enriquez A., Simpson C., Baranchuk A. Update on long QT syndrome. J Cardiovasc Electrophysiol 2019; 30(12): 3068-3078. Doi: 10.1111/jce.14227.
Winbo A., Paterson DJ. The Brain-Heart Connection in Sympathetically Triggered Inherited Arrhythmia Syndromes. Heart Lung Circ 2020; 29(4): 529-537. Doi: 10.1016/j.hlc.2019.11.002.
Schwartz PJ., Priori SG., Cerrone M., Spazzolini C., Odero A., Napolitano C., Bloise R., De Ferrari GM., Klersy C., Moss AJ., et al. Left cardiac sympathetic denervation in the management of high-risk patients affected by the long-QT syndrome. Circulation 2004; 109(15): 1826-33. Doi: 10.1161/01.CIR.0000125523.14403.1E.
Ataklte F., Erqou S., Laukkanen J., Kaptoge S. Meta-analysis of ventricular premature complexes and their relation to cardiac mortality in general populations. Am J Cardiol 2013; 112(8): 1263-70. Doi: 10.1016/j.amjcard.2013.05.065.
Arnar DO., Mairesse GH., Boriani G., Calkins H., Chin A., Coats A., Deharo JC., Svendsen JH., Heidbüchel H., Isa R., et al. Management of asymptomatic arrhythmias: a European Heart Rhythm Association (EHRA) consensus document, endorsed by the Heart Failure Association (HFA), Heart Rhythm Society (HRS), Asia Pacific Heart Rhythm Society (APHRS), Cardiac Arrhythmia Society of Southern Africa (CASSA), and Latin America Heart Rhythm Society (LAHRS). Europace 2019; 21(6): 844–845. Doi: 10.1093/europace/euz046.
Lee V., Perera D., Lambiase P. Prognostic significance of exercise-induced premature ventricular complexes: a systematic review and meta-analysis of observational studies. Heart Asia 2017; 9(1): 14-24. Doi: 10.1136/heartasia-2016-010854.
Lin CY., Chang SL., Chung FP., Chen YY., Lin YJ., Lo LW., Hu YF., Tuan TC., Chao TF., Liao JN., Chang YT., et al. Long-Term Outcome of Non-Sustained Ventricular Tachycardia in Structurally Normal Hearts. PLoS One 2016; 11(8): e0160181. Doi: 10.1371/journal.pone.0160181.
Muser D., Nucifora G., Muser D., Nucifora G., Pieroni M., Castro SA., Casado Arroyo R., Maeda S., Benhayon DA., Liuba I., et al. Prognostic Value of Nonischemic Ringlike Left Ventricular Scar in Patients With Apparently Idiopathic Nonsustained Ventricular Arrhythmias. Circulation 2021; 143(14): 1359-1373. Doi: 10.1161/CIRCULATIONAHA.120.047640.
Aquaro GD., Pingitore A., Strata E., Di Bella G., Molinaro S., Lombardi M. Cardiac magnetic resonance predicts outcome in patients with premature ventricular complexes of left bundle branch block morphology. J Am Coll Cardiol 2010; 56(15): 1235-43. Doi: 10.1016/j.jacc.2010.03.087.
Чуева К.А., Татарский Р.Б., Ковальчук Т.С., Первунина Т.М., Труфанов Г.Е., Рыжков А.В., Фокин В.А., Лебедев Д.С., Васичкина Е.С. Возможности магнитно-резонансной томографии в поиске субстрата «идиопатических» желудочковых аритмий у детей. Вестник аритмологии. 2021;28(4):9-14.
Prystowsky EN., Padanilam BJ., Joshi S., Fogel RI. Ventricular arrhythmias in the absence of structural heart disease. J Am Coll Cardiol 2012; 59(20): 1733-44. Doi: 10.1016/j.jacc.2012.01.036.
Niwano S., Wakisaka Y., Niwano H., Fukaya H., Kurokawa S., Kiryu M., Hatakeyama Y., Izumi T. Prognostic significance of frequent premature ventricular contractions originating from the ventricular outflow tract in patients with normal left ventricular function. Heart 2009; 95(15): 1230-7. Doi: 10.1136/hrt.2008.159558.
Sharma N., Cortez D., Imundo JR. High burden of premature ventricular contractions in structurally normal hearts: To worry or not in pediatric patients? Ann Noninvasive Electrocardiol 2019; 24(6): e12663. Doi: 10.1111/anec.12663.
Hamon D., Swid MA., Rajendran PS., Liu A., Boyle NG., Shivkumar K., Bradfield JS. Premature ventricular contraction diurnal profiles predict distinct clinical characteristics and beta-blocker responses. J Cardiovasc Electrophysiol 2019; 30(6): 836-843. Doi: 10.1111/jce.13944.
Pfammatter JP., Paul T. Idiopathic ventricular tachycardia in infancy and childhood: a multicenter study on clinical profile and outcome. Working Group on Dysrhythmias and Electrophysiology of the Association for European Pediatric Cardiology. J Am Coll Cardiol 1999; 33(7): 2067-72. Doi: 10.1016/s0735-1097(99)00105-9.
Kjekshus J., Bathen J., Orning OM., Storstein L. A double-blind, crossover comparison of flecainide acetate and disopyramide phosphate in the treatment of ventricular premature complexes. Am J Cardiol 1984; 53(5): 72B-78B. Doi: 10.1016/0002-9149(84)90506-x.
Krittayaphong R., Sriratanasathavorn C., Dumavibhat C., Pumprueg S., Boonyapisit W., Pooranawattanakul S., Phrudprisan S., Kangkagate C. Electrocardiographic predictors of long-term outcomes after radiofrequency ablation in patients with right-ventricular outflow tract tachycardia. Europace 2006; 8(8): 601-6. Doi: 10.1093/europace/eul067.
Komatsu Y., Nogami A., Kurosaki K., Morishima I., Masuda K., Ozawa T., Kaneshiro T., Hanaki Y., Shinoda Y., Talib AK., et al. Fascicular Ventricular Tachycardia Originating From Papillary Muscles: Purkinje Network Involvement in the Reentrant Circuit. Circ Arrhythm Electrophysiol 2017; 10(3): e004549. Doi: 10.1161/CIRCEP.116.004549.
Singh SN., Fletcher RD., Fisher SG., Singh BN., Lewis HD., Deedwania PC., Massie BM., Colling C., Lazzeri D. Amiodarone in patients with congestive heart failure and asymptomatic ventricular arrhythmia. Survival Trial of Antiarrhythmic Therapy in Congestive Heart Failure. N Engl J Med 1995; 333(2): 77-82. Doi: 10.1056/NEJM199507133330201
Callans DJ., Menz V., Schwartzman D., Gottlieb CD., Marchlinski FE. Repetitive monomorphic tachycardia from the left ventricular outflow tract: electrocardiographic patterns consistent with a left ventricular site of origin. J Am Coll Cardiol 1997; 29(5): 1023-7. Doi: 10.1016/s0735-1097(97)00004-1.
Kanagaratnam L., Tomassoni G., Schweikert R., Pavia S., Bash D., Beheiry S., Neibauer M., Saliba W., Chung M., Tchou P., et al. Ventricular tachycardias arising from the aortic sinus of valsalva: an under-recognized variant of left outflow tract ventricular tachycardia. J Am Coll Cardiol 2001; 37(5): 1408-14. Doi: 10.1016/s0735-1097(01)01127-5.
Lerman BB. Response of nonreentrant catecholamine-mediated ventricular tachycardia to endogenous adenosine and acetylcholine. Evidence for myocardial receptor-mediated effects. Circulation 1993; 87(2): 382-90. Doi: 10.1161/01.cir.87.2.382.
Baksiene D., Sileikiene R., Sileikis V., Kazakevicius T., Zabiela V., Zebiene M., Puodziukynas A. Idiopathic ventricular tachycardia in children: curative therapy with radiofrequency ablation. Medicina (Kaunas) 2007; 43(10): 803-7.
van Huls van Taxis CF., Piers SR., de Riva Silva M., Dekkers OM., Pijnappels DA., Schalij MJ., Wijnmaalen AP., Zeppenfeld K. Fatigue as Presenting Symptom and a High Burden of Premature Ventricular Contractions Are Independently Associated With Increased Ventricular Wall Stress in Patients With Normal Left Ventricular Function. Circ Arrhythm Electrophysiol 2015; 8(6): 1452-9. Doi: 10.1161/CIRCEP.115.003091.
Bogun F., Crawford T., Reich S., Koelling TM., Armstrong W., Good E., Jongnarangsin K., Marine JE., Chugh A., Pelosi F., et al. Radiofrequency ablation of frequent, idiopathic premature ventricular complexes: comparison with a control group without intervention. Heart Rhythm 2007; 4(7): 863-7. Doi: 10.1016/j.hrthm.2007.03.003.
Lee A., Denman R., Haqqani HM. Ventricular Ectopy in the Context of Left Ventricular Systolic Dysfunction: Risk Factors and Outcomes Following Catheter Ablation. Heart Lung Circ 2019; 28(3): 379-388. Doi: 10.1016/j.hlc.2018.01.012.
Mountantonakis SE., Frankel DS., Gerstenfeld EP., Dixit S., Lin D., Hutchinson MD., Riley M., Bala R., Cooper J., Callans D., et al. Reversal of outflow tract ventricular premature depolarization-induced cardiomyopathy with ablation: effect of residual arrhythmia burden and preexisting cardiomyopathy on outcome. Heart Rhythm 2011; 8(10): 1608-14. Doi: 10.1016/j.hrthm.2011.04.026.
Penela D., Van Huls Van Taxis C., Van Huls Vans Taxis C., Aguinaga L., Fernández-Armenta J., Mont L., Castel MA., Heras M., Tolosana JM., Sitges M., et al. Neurohormonal, structural, and functional recovery pattern after premature ventricular complex ablation is independent of structural heart disease status in patients with depressed left ventricular ejection fraction: a prospective multicenter study. J Am Coll Cardiol 2013; 62(13): 1195-202. Doi: 10.1016/j.jacc.2013.06.012.
Zang M., Zhang T., Mao J., Zhou S., He B. Beneficial effects of catheter ablation of frequent premature ventricular complexes on left ventricular function. Heart 2014; 100(10): 787-93. Doi: 10.1136/heartjnl-2013-305175.
Jabbari R., Engstrøm T., Glinge C., Risgaard B., Jabbari J., Winkel BG., Terkelsen CJ., Tilsted HH., Jensen LO., Hougaard M., et al. Incidence and risk factors of ventricular fibrillation before primary angioplasty in patients with first ST-elevation myocardial infarction: a nationwide study in Denmark. J Am Heart Assoc 2015; 4(1): e001399. Doi: 10.1161/JAHA.114.001399.
Orvin K., Eisen A., Goldenberg I., Gottlieb S., Kornowski R., Matetzky S., Golovchiner G., Kuznietz J., Gavrielov-Yusim N., Segev A., et al. Outcome of contemporary acute coronary syndrome complicated by ventricular tachyarrhythmias. Europace 2016; 18(2): 219-26. Doi: 10.1093/europace/euv027.
Demirel F., Rasoul S., Elvan A., Ottervanger JP., Dambrink JH., Gosselink AT., Hoorntje JC., Ramdat Misier AR., van 't Hof AW. Impact of out-of-hospital cardiac arrest due to ventricular fibrillation in patients with ST-elevation myocardial infarction admitted for primary percutaneous coronary intervention: Impact of ventricular fibrillation in STEMI patients. Eur Heart J Acute Cardiovasc Care 2015; 4(1): 16-23. Doi: 10.1177/2048872614547448.
Mehta RH., Starr AZ., Lopes RD., Hochman JS., et al. Incidence of and outcomes associated with ventricular tachycardia or fibrillation in patients undergoing primary percutaneous coronary intervention. JAMA 2009; 301(17): 1779-1789. Doi: 10.1001/jama.2009.600.
Demidova MM., Carlson J., Erlinge D., Platonov PG. Predictors of ventricular fibrillation at reperfusion in patients with acute ST-elevation myocardial infarction treated by primary percutaneous coronary intervention. The American Journal of Cardiology 2015; 115(4): 417-422. Doi: 10.1016/j.amjcard.2014.11.025.
Dumas F., Cariou A., Manzo-Silberman S., Grimaldi D., Vivien B., Rosencher J., Empana JP., Carli P., Mira JP., Jouven X., et al. Immediate percutaneous coronary intervention is associated with better survival after out-of-hospital cardiac arrest: insights from the PROCAT (Parisian Region Out of hospital Cardiac ArresT) registry. Circ Cardiovasc Interv 2010; 3(3): 200-7. Doi: 10.1161/CIRCINTERVENTIONS.109.913665
Cheng Y.-J., Li Z.-Y., Yao F.-J., Xu X.-J., et al. Early repolarization is associated with a significantly increased risk of ventricular arrhythmias and sudden cardiac death in patients with structural heart disease. Heart Rhythm 2017; 14(8): 1157-1164. Doi: 10.1016/j.hrthm.2017.04.022.
Dumas F., Bougouin W., Geri G., Lamhaut L., et al. Emergency percutaneous coronary intervention in post-cardiac arrest patients without ST-segment elevation pattern: insights from the PROCAT II registry. JACC 2016; 9(10): 1011-1018. Doi: 10.1016/j.jcin.2016.02.001.
Ibanez B., James S., Agewall S., Antunes MJ., Bucciarelli-Ducci C., et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). European Heart Journal 2018; 39(2): 119-177. Doi: 10.1093/eurheartj/ehx393.
Chatterjee S., Chaudhuri D., Vedanthan R., Fuster V., et al. Early intravenous beta-blockers in patients with acute coronary syndrome–a meta-analysis of randomized trials. International Journal of Cardiology 2013; 168(2): 915-921. Doi: 10.1016/j.ijcard.2012.10.050.
Windecker S., Koth P., Alfonso F., et al. 2014 ЕОК/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ЕОК) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). European Heart Journal 2014; 35(37): 2541-619. Doi: 10.1093/eurheartj/ehu278.
Roffi M., Patrono C., Cotter J.P., et al. 2015 ЕОК Guidelines for the Management of Acute Coronary Syndromes in Patients Presenting Without Persistent ST-Segment Elevation. European Heart Journal 2016; 37(3): 267-315. Doi: 10.1093/eurheartj/ehv320.
Steg PG., James SK., Atar D., et al. ЕОК Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. European Heart Journal 2012; 33(20): 2569-2619. Doi: 10.1093/eurheartj/ehs215.
Soholm H., Wachte UK., Nietsen SL., et al. Tertiary centres have improved survival compared to other hospitals in the Copenhagen area after out-of-hospital cardiac arrest. Resuscitation 2013; 84(2): 162-167. Doi: 10.1016/j.resuscitation.2012.06.029.
Boersma E., Maas AC., Deckers JW., Simoons ML. Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. Lancet 1996; 348(9030): 771-775. Doi: 10.1016/S0140-6736(96)02514-7.
Boersma E. Primary Coronary Angioplasty vs. Thrombolysis Group. Does time matter? A pooled analysis of randomized clinical trials comparing primary percutaneous coronary intervention and in-hospital fibrinolysis in acute myocardial infarction patients. European Heart Journal 2006; 27(7): 779-788. Doi: 10.1093/eurheartj/ehi810.
Keeley EC., Boura JA., Grines CL. Comparison of primary and facilitated percutaneous coronary interventions for ST-etevation myocardial infarction: quantitative review of randomised trials. Lancet 2006; 367(9510):5 79-88. Doi: 10.1016/S0140-6736(06)68148-8.
Spaulding CM., Joly LM., Rosenberg A., et al. Immediate coronary angiography in survivors of out-of-hospital cardiac arrest. The New England Journal of Medicine 1997; 336(23): 1629-33. Doi: 10.1056/NEJM199706053362302.
Bowers TR., O'Neitt WW., Grines C., et al. Effect of reperfusion on biventricular function and survival after right ventricular infarction. The New England Journal of Medicine 1998; 338(14): 933-940. Doi: 10.1056/NEJM199804023381401.
Gorenek B., Blomstrom Lundqvist C., Brugada P., Terradetlas J., et al. Cardiac arrhythmias in acute coronary syndromes: position paper from the joint EH RA, ACCA, and EAPCI task force. Europace 2015; 4(4): 386. Doi: 10.1177/2048872614550583.
Piccini JP., Hranitzky PM., Kilaru R., Rouleau JL., White HD., Aylward PE., Van de Werf F., Solomon SD., Califf RM., Velazquez EJ. Relation of mortality to failure to prescribe beta blockers acutely in patients with sustained ventricular tachycardia and ventricular fibrillation following acute myocardial infarction (from the VALsartan In Acute myocardial iNfarcTion trial [VALIANT] Registry). Am J Cardiol 2008; 102(11): 1427-32. Doi: 10.1016/j.amjcard.2008.07.033.
Huikuri HV., Castellanos A., Myerburg RJ. Sudden death due to cardiac arrhythmias. N Engl J Med 2001; 345(20): 1473-82. Doi: 10.1056/NEJMra000650.
Bougouin W., Marijon E., Puymirat E., Defaye P., Celermajer DS., Le Heuzey JY., Boveda S., Kacet S., Mabo P., Barnay C., Det al. Incidence of sudden cardiac death after ventricular fibrillation complicating acute myocardial infarction: a 5-year cause-of-death analysis of the FAST-MI 2005 registry. Eur Heart J 2014; 35(2): 116-22. Doi: 10.1093/eurheartj/eht453.
Nademanee K., Taylor R., Bailey WE., Rieders DE., Kosar EM. Treating electrical storm : sympathetic blockade versus advanced cardiac life support-guided therapy. Circulation 2000; 102(7): 742-7. Doi: 10.1161/01.cir.102.7.742.
Piccini JP., Schulte PJ., Pieper KS., Mehta RH., White HD., Van de Werf F., Ardissino D., Califf RM., Granger CB., Ohman EM., et al. Antiarrhythmic drug therapy for sustained ventricular arrhythmias complicating acute myocardial infarction. Crit Care Med 2011; 39(1): 78-83. Doi: 10.1097/CCM.0b013e3181fd6ad7.
Ahn JM., Lee KH., Yoo SY., Cho YR., Suh J., Shin ES., Lee JH., Shin DI., Kim SH., Baek SH., et al. Prognosis of Variant Angina Manifesting as Aborted Sudden Cardiac Death. J Am Coll Cardiol 2016; 68(2): 137-45. Doi: 10.1016/j.jacc.2016.04.050. P.
Sueda S., Kohno H. Optimal Medications and Appropriate Implantable Cardioverter-defibrillator Shocks in Aborted Sudden Cardiac Death Due to Coronary Spasm. Intern Med 2018; 57(10): 1361-1369. Doi: 10.2169/internalmedicine.8796-17.
Rodríguez-Mañero M., Oloriz T., le Polain de Waroux JB., Burri H., Kreidieh B., de Asmundis C., Arias MA., Arbelo E., Díaz Fernández B., Fernández-Armenta J., et al. Long-term prognosis of patients with life-threatening ventricular arrhythmias induced by coronary artery spasm. Europace 2018; 20(5): 851-858. Doi: 10.1093/europace/eux052.
Buxton AE., Lee KL., DiCarlo L., Gold MR., Greer GS., Prystowsky EN., O'Toole MF., Tang A., Fisher JD., Coromilas J., et al. Electrophysiologic testing to identify patients with coronary artery disease who are at risk for sudden death. Multicenter Unsustained Tachycardia Trial Investigators. N Engl J Med 2000; 342(26): 1937-45. Doi: 10.1056/NEJM200006293422602.
Exner DV., Kavanagh KM., Slawnych MP., Mitchell LB., Ramadan D., Aggarwal SG., Noullett C., Van Schaik A., Mitchell RT., Shibata MA., et al. Noninvasive risk assessment early after a myocardial infarction the REFINE study. J Am Coll Cardiol 2007; 50(24): 2275-84. Doi: 10.1016/j.jacc.2007.08.042.
Malik M., Camm AJ., Janse MJ., Julian DG., Frangin GA., Schwartz PJ. Depressed heart rate variability identifies postinfarction patients who might benefit from prophylactic treatment with amiodarone: a substudy of EMIAT (The European Myocardial Infarct Amiodarone Trial). J Am Coll Cardiol 2000; 35(5): 1263-75. Doi: 10.1016/s0735-1097(00)00571-4.
Allman KC., Shaw LJ., Hachamovitch R., Udelson JE. Myocardial viability testing and impact of revascularization on prognosis in patients with coronary artery disease and left ventricular dysfunction: a meta-analysis. J Am Coll Cardiol 2002; 39(7): 1151-8. Doi: 10.1016/s0735-1097(02)01726-6.
Altmann DR., Mutschelknauss M., Ehl N., Koller M., Schaer B., Jörg L., Ammann P., Kühne M., Rickli H., Osswald S., et al. Prevalence of severely impaired left ventricular ejection fraction after reperfused ST-elevation myocardial infarction. Swiss Med Wkly 2013; 143: w13869. Doi: 10.4414/smw.2013.13869.
Shen L., Jhund PS., Petrie MC., Claggett BL., Barlera S., Cleland JGF., Dargie HJ., Granger CB., Kjekshus J., Køber L., et al. Declining Risk of Sudden Death in Heart Failure. N Engl J Med 2017; 377(1): 41-51. Doi: 10.1056/NEJMoa1609758.
Gatzoulis KA., Tsiachris D., Arsenos P., Archontakis S., Dilaveris P., Vouliotis A., Sideris S., Skiadas I., Kallikazaros I., Stefanadis C. Prognostic value of programmed ventricular stimulation for sudden death in selected high risk patients with structural heart disease and preserved systolic function. Int J Cardiol 2014; 176(3): 1449-51. Doi: 10.1016/j.ijcard.2014.08.068.
Olshansky B., Hahn EA., Hartz VL., Prater SP., Mason JW. Clinical significance of syncope in the electrophysiologic study versus electrocardiographic monitoring (ESVEM) trial. The ESVEM Investigators. Am Heart J 1999; 137(5): 878-86. Doi: 10.1016/s0002-8703(99)70412-6.
Antiarrhythmics versus Implantable Defibrillators (AVID) Investigators. A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. N Engl J Med 1997; 337(22): 1576-83. Doi: 10.1056/NEJM199711273372202.
Pacifico A., Hohnloser SH., Williams JH., Tao B., Saksena S., Henry PD., Prystowsky EN. Prevention of implantable-defibrillator shocks by treatment with sotalol. d,l-Sotalol Implantable Cardioverter-Defibrillator Study Group. N Engl J Med 1999; 340(24): 1855-62. Doi: 10.1056/NEJM199906173402402.
Willems S., Tilz RR., Steven D., Kääb S., Wegscheider K., Gellér L., Meyer C., Heeger CH., Metzner A., Sinner MF., et al. BERLIN VT Investigators. Preventive or Deferred Ablation of Ventricular Tachycardia in Patients With Ischemic Cardiomyopathy and Implantable Defibrillator (BERLIN VT): A Multicenter Randomized Trial. Circulation 2020; 141(13): 1057-1067. Doi: 10.1161/CIRCULATIONAHA.119.043400.
Kuck KH., Schaumann A., Eckardt L., Willems S., Ventura R., Delacrétaz E., Pitschner HF., Kautzner J., Schumacher B., Hansen PS. VTACH study group. Catheter ablation of stable ventricular tachycardia before defibrillator implantation in patients with coronary heart disease (VTACH): a multicentre randomised controlled trial. Lancet 2010; 375(9708): 31-40. Doi: 10.1016/S0140-6736(09)61755-4.
Kuck KH., Tilz RR., Deneke T., Hoffmann BA., Ventura R., Hansen PS., Zarse M., Hohnloser SH., Kautzner J., Willems S. SMS Investigators. Impact of Substrate Modification by Catheter Ablation on Implantable Cardioverter-Defibrillator Interventions in Patients With Unstable Ventricular Arrhythmias and Coronary Artery Disease: Results From the Multicenter Randomized Controlled SMS (Substrate Modification Study). Circ Arrhythm Electrophysiol 2017; 10(3): e004422. Doi: 10.1161/CIRCEP.116.004422.
Pitt B., White H., Nicolau J., Martinez F., Gheorghiade M., Aschermann M., van Veldhuisen DJ., Zannad F., Krum H., Mukherjee R., et al. EPHESUS Investigators. Eplerenone reduces mortality 30 days after randomization following acute myocardial infarction in patients with left ventricular systolic dysfunction and heart failure. J Am Coll Cardiol 2005; 46(3): 425-31. Doi: 10.1016/j.jacc.2005.04.038.
Peck KY., Lim YZ., Hopper I., Krum H. Medical therapy versus implantable cardioverter -defibrillator in preventing sudden cardiac death in patients with left ventricular systolic dysfunction and heart failure: a meta-analysis of > 35,000 patients. Int J Cardiol 2014; 173(2): 197-203. Doi: 10.1016/j.ijcard.2014.02.014.
Chatterjee S., Udell JA., Sardar P., Lichstein E., Ryan JJ. Comparable benefit of β-blocker therapy in heart failure across regions of the world: meta-analysis of randomized clinical trials. Can J Cardiol 2014; 30(8): 898-903. Doi: 10.1016/j.cjca.2014.03.012.
Neumann FJ., Sousa-Uva M., Ahlsson A., Alfonso F., Banning AP., Benedetto U., Byrne RA., Collet JP., Falk V., Head SJ., et al. ESC Scientific Document Group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 2019; 40(2): 87-165. Doi: 10.1093/eurheartj/ehy394.
Dor V., Civaia F., Alexandrescu C., Sabatier M., Montiglio F. Favorable effects of left ventricular reconstruction in patients excluded from the Surgical Treatments for Ischemic Heart Failure (STICH) trial. J Thorac Cardiovasc Surg 2011; 141(4): 905-16, 916.e1-4. Doi: 10.1016/j.jtcvs.2010.10.026.
Jones RH., Velazquez EJ., Michler RE., Sopko G., Oh JK., O'Connor CM., Hill JA., Menicanti L., Sadowski Z., Desvigne-Nickens P., et al. STICH Hypothesis 2 Investigators. Coronary bypass surgery with or without surgical ventricular reconstruction. N Engl J Med 2009; 360(17): 1705-17. Doi: 10.1056/NEJMoa0900559.
Babokin V., Shipulin V., Batalov R., Popov S. Surgical ventricular reconstruction with endocardectomy along radiofrequency ablation-induced markings. J Thorac Cardiovasc Surg 2013; 146(5): 1133-8. Doi: 10.1016/j.jtcvs.2012.08.067.
Sartipy U., Albåge A., Insulander P., Lindblom D. Surgery for ventricular tachycardia in patients undergoing surgical ventricular restoration: the Karolinska approach. J Interv Card Electrophysiol 2007; 19(3): 171-8. Doi: 10.1007/s10840-007-9152-7.
Bayés de Luna A., Coumel P., Leclercq JF. Ambulatory sudden cardiac death: mechanisms of production of fatal arrhythmia on the basis of data from 157 cases. Am Heart J 1989; 117(1): 151-9. Doi: 10.1016/0002-8703(89)90670-4.
Josephson ME., Harken AH., Horowitz LN. Endocardial excision: a new surgical technique for the treatment of recurrent ventricular tachycardia. Circulation 1979; 60(7): 1430-9. Doi: 10.1161/01.cir.60.7.1430.
Reddy YM., Chinitz L., Mansour M., Bunch TJ., Mahapatra S., Swarup V., Di Biase L., Bommana S., Atkins D., Tung R., et al. Percutaneous left ventricular assist devices in ventricular tachycardia ablation: multicenter experience. Circ Arrhythm Electrophysiol 2014; 7(2): 244-50. Doi: 10.1161/CIRCEP.113.000548.
Dor V., Sabatier M., Montiglio F., Rossi P., Toso A., Di Donato M. Results of nonguided subtotal endocardiectomy associated with left ventricular reconstruction in patients with ischemic ventricular arrhythmias. J Thorac Cardiovasc Surg 1994; 107(5): 1301-7.
Molossi S., Agrawal H., Mery CM., Krishnamurthy R., et al. Outcomes in anomalous aortic origin of a coronary artery following a prospective standardized approach. Circulation: Cardiovascular Interventions 2020; 13(2): e008445. Doi: 10.1161/CIRCINTERVENTIONS.119.008445.
Krasuski RA., Magyar D., Hart S., Kalahasti V., et al. Long-term outcome and impact of surgery on adults with coronary arteries originating from the opposite coronary cusp. Circulation 2011; 123(2): 154-62. Doi: 10.1161/CIRCULATIONAHA.109.921106.
Jegatheeswaran A., Devlin PJ., McCrindle BW., Williams WG., et al. Features associated with myocardial ischemia in anomalous aortic origin of a coronary artery: a congenital heart surgeons’ society study. The Journal of Thoracic and Cardiovascular Surgery 2019; 158(3): 822-834.e3. Doi: 10.1016/j.jtcvs.2019.02.122.
Jegatheeswaran A., Devlin PJ., Williams WG., et al. Outcomes after anomalous aortic origin of a coronary artery repair: a congenital heart surgeons’ society study. The Journal of Thoracic and Cardiovascular Surgery 2020 Sep;160(3):757-771.e5. Doi: 10.1016/j.jtcvs.2020.01.114.
Elliott P., Andersson B., Arbustini E., et al. Classification of the cardiomyopathies: a position statement from the European Society Of Cardiology Working Group on Myocardial and Pericardial Diseases. European Heart Journal 2008; 29(2): 270-276. Doi: 10.1093/eurheartj/ehm342.
Ader F., De Groote P., Réant P., Rooryck-Thambo C., et al. FLNC pathogenic variants in patients with cardiomyopathies: prevalence and genotype-phenotype correlations. Clinical Genetics 2019; 96(4): 317-329. Doi: 10.1111/cge.13594.
Gigli M., Merlo M., Graw SL., Barbati G., et al. Genetic risk of arrhythmic phenotypes in patients with dilated cardiomyopathy. JACC 2019; 74(11): 1480-1490. Doi: 10.1016/j.jacc.2019.06.072.
Van den Hoogenhof MMG., Beqqali A., Amin AS., van der Made I., et al. RBM20 mutations induce an arrhythmogenic dilated cardiomyopathy related to disturbed calcium handling. Circulation 2018; 138(13): 1330-1342. Doi: 10.1161/CIRCULATIONAHA.117.031947
Kayvanpour E., Sedaghat-Hamedani F., Amr A., Lai A., Haas J., Holzer DB., et al. Genotype-phenotype associations in dilated cardiomyopathy: meta-analysis on more than 8000 individuals. Clinical Research in Cardiology 2017; 106(2): 127-139. Doi: 10.1007/s00392-016-1033-6.
Ortiz-Genga MF., Cuenca S., Dal Ferro M., Zorio E., et al. Truncating FLNC mutations are associated with high-risk dilated and arrhythmogenic cardiomyopathies. JACC 2016; 68(22): 2440-2451. Doi: 10.1016/j.jacc.2016.09.927.
Di Marco A., Anguera I., Schmitt M., Klem I., et al. Late gadolinium enhancement and the risk for ventricular arrhythmias or sudden death in dilated cardiomyopathy: systematic review and meta-analysis. JACC 2017; 5(1): 28-38. Doi: 10.1016/j.jchf.2016.09.017.
Francone M. Role of cardiac magnetic resonance in the evaluation of dilated cardiomyopathy: diagnostic contribution and prognostic significance. ISRN Radiology 2014; 365404. Doi: 10.1155/2014/365404. УДД 5 УУР С
Klem I., Klein M., Khan M., Yang E.Y., et al. Relationship of LVEF and myocardial scar to long-term mortality risk and mode of death in patients with nonischemic cardiomyopathy. Circulation 2021; 143(14): 1343-1358. Doi: 10.1161/CIRCULATIONAHA.120.048477.
Goldberger JJ., Subačius H., Patel T., et al. Sudden cardiac death risk stratification in patients with nonischemic dilated cardiomyopathy. JACC 2014; 63(18): 1879-1889. Doi: 10.1016/j.jacc.2013.12.021.
Link MS., Costeas XF., Griffith JL., Colburn CD., et al. High incidence of appropriate implantable cardioverter-defibrillator therapy in patients with syncope of unknown etiology and inducible ventricular arrhythmias. JACC 1997; 29(2): 370-375. Doi: 10.1016/s0735-1097(96)00477-9.
Pasotti M., Klersy C., Pilotto A., Marziliano N., Rapezzi C., Serio A., Mannarino S., Gambarin F., Favalli V., Grasso M., et al. Long-term outcome and risk stratification in dilated cardiolaminopathies. J Am Coll Cardiol 2008; 52(15): 1250-60. Doi: 10.1016/j.jacc.2008.06.044.
Skjølsvik ET., Hasselberg NE., Dejgaard LA., Lie ØH., Andersen K., Holm T., Edvardsen T., Haugaa KH. Exercise is Associated With Impaired Left Ventricular Systolic Function in Patients With Lamin A/C Genotype. J Am Heart Assoc 2020; 9(2): e012937. Doi: 10.1161/JAHA.119.012937.
Cardiac Arrhythmia Suppression Trial (CAST) Investigators. Preliminary report: effect of encainide and flecainide on mortality in a randomized trial of arrhythmia suppression after myocardial infarction. N Engl J Med 1989; 321(6): 406-12. Doi: 10.1056/NEJM198908103210629.
Connolly SJ., Camm AJ., Halperin JL., Joyner C., Alings M., Amerena J., Atar D., Avezum Á., Blomström P., Borggrefe M., et al. Dronedarone in high-risk permanent atrial fibrillation. N Engl J Med 2011; 365(24): 2268-76. Doi: 10.1056/NEJMoa1109867.
Beggs SAS., Jhund PS., Jackson CE., McMurray JJV., Gardner RS. Non-ischaemic cardiomyopathy, sudden death and implantable defibrillators: a review and meta-analysis. Heart 2018; 104(2): 144-150. Doi: 10.1136/heartjnl-2016-310850.
Zabel M., Willems R., Lubinski A., Bauer A., Brugada J., Conen D., Flevari P., Hasenfuß G., Svetlosak M., Huikuri HV., et al. Clinical effectiveness of primary prevention implantable cardioverter-defibrillators: results of the EU-CERT-ICD controlled multicentre cohort study. Eur Heart J 2020; 41(36): 3437-3447. Doi: 10.1093/eurheartj/ehaa226.
van Rijsingen IA., Arbustini E., Elliott PM., Mogensen J., Hermans-van Ast JF., van der Kooi AJ., van Tintelen JP., van den Berg MP., Pilotto A., Pasotti M., et al. Risk factors for malignant ventricular arrhythmias in lamin a/c mutation carriers a European cohort study. J Am Coll Cardiol 2012; 59(5): 493-500. Doi: 10.1016/j.jacc.2011.08.078.
Thuillot M., Maupain C., Gandjbakhch E., Waintraub X., Hidden-Lucet F., Isnard R., Ader F., Rouanet S., Richard P., Charron P. External validation of risk factors for malignant ventricular arrhythmias in lamin A/C mutation carriers. Eur J Heart Fail 2019; 21(2): 253-254. Doi: 10.1002/ejhf.1384.
Effect of prophylactic amiodarone on mortality after acute myocardial infarction and in congestive heart failure: meta-analysis of individual data from 6500 patients in randomised trials. Amiodarone Trials Meta-Analysis Investigators. Lancet 1997; 350(9089): 1417-24.
Di Marco A., Brown PF., Bradley J., Nucifora G., Claver E., de Frutos F., Dallaglio PD., Comin-Colet J., Anguera I., Miller CA., et al. Improved Risk Stratification for Ventricular Arrhythmias and Sudden Death in Patients With Nonischemic Dilated Cardiomyopathy. J Am Coll Cardiol 2021; 77(23): 2890-2905. Doi: 10.1016/j.jacc.2021.04.030.
Merlo M., Gentile P., Artico J., Cannatà A., Paldino A., De Angelis G., Barbati G., Alonge M., Gigli M., Pinamonti B., et al. Arrhythmic risk stratification in patients with dilated cardiomyopathy and intermediate left ventricular dysfunction. J Cardiovasc Med (Hagerstown) 2019; 20(5): 343-350. Doi: 10.2459/JCM.0000000000000792.
Mariani M.V., Pierucci N., Fanisio F. Inherited Arrhythmias in the Pediatric Population: An Updated Overview. Medicina (Kaunas) 2024; 60(1): 94. Doi: 10.3390/medicina60010094.
Zecchin M., Di Lenarda A., Gregori D., Merlo M., Pivetta A., Vitrella G., Sabbadini G., Mestroni L., Sinagra G. Are nonsustained ventricular tachycardias predictive of major arrhythmias in patients with dilated cardiomyopathy on optimal medical treatment? Pacing Clin Electrophysiol 2008; 31(3): 290-9. Doi: 10.1111/j.1540-8159.2008.00988.x.
Connolly SJ., Hallstrom AP., Cappato R., Schron EB., Kuck KH., Zipes DP., Greene HL., Boczor S., Domanski M., Follmann D., et al. Meta-analysis of the implantable cardioverter defibrillator secondary prevention trials. AVID, CASH and CIDS studies. Antiarrhythmics vs Implantable Defibrillator study. Cardiac Arrest Study Hamburg . Canadian Implantable Defibrillator Study. Eur Heart J 2000; 21(24): 2071-8. Doi: 10.1053/euhj.2000.2476.
Dinov B., Fiedler L., Schönbauer R., Bollmann A., Rolf S., Piorkowski C., Hindricks G., Arya A. Outcomes in catheter ablation of ventricular tachycardia in dilated nonischemic cardiomyopathy compared with ischemic cardiomyopathy: results from the Prospective Heart Centre of Leipzig VT (HELP-VT) Study. Circulation 2014; 129(7): 728-36. Doi: 10.1161/CIRCULATIONAHA.113.003063.
Ebert M., Wijnmaalen AP., de Riva M., Trines SA., Androulakis AFA., Glashan CA., Schalij MJ., Peter van Tintelen J., Jongbloed JDH., Zeppenfeld K. Prevalence and Prognostic Impact of Pathogenic Variants in Patients With Dilated Cardiomyopathy Referred for Ventricular Tachycardia Ablation. JACC Clin Electrophysiol 2020; 6(9): 1103-1114. Doi: 10.1016/j.jacep.2020.04.025.
Muser D., Santangeli P., Castro SA., Pathak RK., Liang JJ., Hayashi T., Magnani S., Garcia FC., Hutchinson MD., Supple GG., et al. Long-Term Outcome After Catheter Ablation of Ventricular Tachycardia in Patients With Nonischemic Dilated Cardiomyopathy. Circ Arrhythm Electrophysiol 2016; 9(10): e004328. Doi: 10.1161/CIRCEP.116.004328.
Tung R., Vaseghi M., Frankel DS., Vergara P., Di Biase L., Nagashima K., Yu R., Vangala S., Tseng CH., Choi EK., et al. Freedom from recurrent ventricular tachycardia after catheter ablation is associated with improved survival in patients with structural heart disease: An International VT Ablation Center Collaborative Group study. Heart Rhythm 2015; 12(9): 1997-2007. Doi: 10.1016/j.hrthm.2015.05.036.
Corrado D., Link MS., Calkins H. Arrhythmogenic Right Ventricular Cardiomyopathy. N Engl J Med 2017; 376(15): 1489-90. Doi: 10.1056/NEJMc1701400.
Aquaro GD., Barison A., Todiere G., Grigoratos C., Ait Ali L., Di Bella G., Emdin M., Festa P. Usefulness of Combined Functional Assessment by Cardiac Magnetic Resonance and Tissue Characterization Versus Task Force Criteria for Diagnosis of Arrhythmogenic Right Ventricular Cardiomyopathy. Am J Cardiol 2016; 118(11): 1730-1736. Doi: 10.1016/j.amjcard.2016.08.056.
Rastegar N., Te Riele AS., James CA., Bhonsale A., Murray B., Tichnell C., Calkins H., Tandri H., Bluemke DA., Kamel IR., et al. Fibrofatty Changes: Incidence at Cardiac MR Imaging in Patients with Arrhythmogenic Right Ventricular Dysplasia/Cardiomyopathy. Radiology 2016; 280(2): 405-12. Doi: 10.1148/radiol.2016150988.
te Riele AS., Bhonsale A., James CA., Rastegar N., Murray B., Burt JR., Tichnell C., Madhavan S., Judge DP., Bluemke DA., et al. Incremental value of cardiac magnetic resonance imaging in arrhythmic risk stratification of arrhythmogenic right ventricular dysplasia/cardiomyopathy-associated desmosomal mutation carriers. J Am Coll Cardiol 2013; 62(19): 1761-9. Doi: 10.1016/j.jacc.2012.11.087.
Cicenia M., Drago F. Arrhythmogenic Cardiomyopathy: Diagnosis, Evolution, Risk Stratification and Pediatric Population-Where Are We? J Cardiovasc Dev Dis 2022; 9(4): 98. Doi: 10.3390/jcdd9040098.
Bhonsale A., Groeneweg JA., James CA., Dooijes D., Tichnell C., Jongbloed JD., Murray B., te Riele AS., van den Berg MP., Bikker H., et al. Impact of genotype on clinical course in arrhythmogenic right ventricular dysplasia/cardiomyopathy-associated mutation carriers. Eur Heart J 2015; 36(14): 847-55. Doi: 10.1093/eurheartj/ehu509.
Rigato I., Bauce B., Rampazzo A., Zorzi A., Pilichou K., Mazzotti E., Migliore F., Marra MP., Lorenzon A., De Bortoli M., et al. Compound and digenic heterozygosity predicts lifetime arrhythmic outcome and sudden cardiac death in desmosomal gene-related arrhythmogenic right ventricular cardiomyopathy. Circ Cardiovasc Genet 2013; 6(6): 533-42. Doi: 10.1161/CIRCGENETICS.113.000288.
Bhonsale A., James CA., Tichnell C., Murray B., Gagarin D., Philips B., Dalal D., Tedford R., Russell SD., Abraham T., et al. Incidence and predictors of implantable cardioverter-defibrillator therapy in patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy undergoing implantable cardioverter-defibrillator implantation for primary prevention. J Am Coll Cardiol 2011; 58(14): 1485-96. Doi: 10.1016/j.jacc.2011.06.043.
Saguner AM., Medeiros-Domingo A., Schwyzer MA., On CJ., Haegeli LM., Wolber T., Hürlimann D., Steffel J., Krasniqi N., Rüeger S., et al. Usefulness of inducible ventricular tachycardia to predict long-term adverse outcomes in arrhythmogenic right ventricular cardiomyopathy. Am J Cardiol 2013; 111(2): 250-7. Doi: 10.1016/j.amjcard.2012.09.025.
Chivulescu M., Lie ØH., Popescu BA., Skulstad H., Edvardsen T., Jurcut RO., Haugaa KH. High penetrance and similar disease progression in probands and in family members with arrhythmogenic cardiomyopathy. Eur Heart J 2020; 41(14): 1401-1410. Doi: 10.1093/eurheartj/ehz570.
James CA., Bhonsale A., Tichnell C., Murray B., Russell SD., Tandri H., Tedford RJ., Judge DP., Calkins H. Exercise increases age-related penetrance and arrhythmic risk in arrhythmogenic right ventricular dysplasia/cardiomyopathy-associated desmosomal mutation carriers. J Am Coll Cardiol 2013; 62(14): 1290-1297. Doi: 10.1016/j.jacc.2013.06.033.
Lie ØH., Dejgaard LA., Saberniak J., Rootwelt C., Stokke MK., Edvardsen T., Haugaa KH. Harmful Effects of Exercise Intensity and Exercise Duration in Patients With Arrhythmogenic Cardiomyopathy. JACC Clin Electrophysiol 2018; 4(6): 744-753. Doi: 10.1016/j.jacep.2018.01.010.
Saberniak J., Hasselberg NE., Borgquist R., Platonov PG., Sarvari SI., Smith HJ., Ribe M., Holst AG., Edvardsen T., Haugaa KH. Vigorous physical activity impairs myocardial function in patients with arrhythmogenic right ventricular cardiomyopathy and in mutation positive family members. Eur J Heart Fail 2014; 16(12): 1337-44. Doi: 10.1002/ejhf.181.
Towbin JA., McKenna WJ., Abrams DJ., Ackerman MJ., Calkins H., Darrieux FCC., Daubert JP., de Chillou C., DePasquale EC., Desai MY., et al. 2019 HRS expert consensus statement on evaluation, risk stratification, and management of arrhythmogenic cardiomyopathy. Heart Rhythm 2019; 16(11): e301-e372. Doi: 10.1016/j.hrthm.2019.05.007.
Te Riele ASJM., James CA., Calkins H., Tsatsopoulou A. Arrhythmogenic Right Ventricular Cardiomyopathy in Pediatric Patients: An Important but Underrecognized Clinical Entity. Front Pediatr 2021; 9: 750916. Doi: 10.3389/fped.2021.750916.
Sawant AC., Te Riele AS., Tichnell C., Murray B., Bhonsale A., Tandri H., Judge DP., Calkins H., James CA. Safety of American Heart Association-recommended minimum exercise for desmosomal mutation carriers. Heart Rhythm 2016; 13(1): 199-207. Doi: 10.1016/j.hrthm.2015.08.035.
Denis A., Sacher F., Derval N., Lim HS., Cochet H., Shah AJ., Daly M., Pillois X., Ramoul K., Komatsu Y., et al. Diagnostic value of isoproterenol testing in arrhythmogenic right ventricular cardiomyopathy. Circ Arrhythm Electrophysiol 2014; 7(4): 590-7. Doi: 10.1161/CIRCEP.113.001224.
Marcus GM., Glidden DV., Polonsky B., et al. Efficacy of antiarrhythmic drugs in arrhythmogenic right ventricular cardiomyopathy: a report from the North American ARVC Registry. JACC 2009; 54(7): 609-615. Doi: 10.1016/j.jacc.2009.04.052.
Canpolat U., Aytemir K., Dural M., et al. Fragmented QRS complex predicts the arrhythmic events in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia: frQRS and outcomes in ARVC/D / Journal of Cardiovascular Electrophysiology 2013; 24(11): 1260-1266. Doi: 10.1111/jce.12202.
Corrado D., Calkins H., Link M.S., et al. Prophylactic implantable defibrillator in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia and no prior ventricular fibrillation or sustained ventricular tachycardia. Circulation 2010; 122(12): 1144-1152. Doi: 10.1161/CIRCULATIONAHA.109.913871
Martin A., Crawford J., Skinner JR., Smith W. High arrhythmic burden but low mortality during long-term follow-up in arrhythmogenic right ventricular cardiomyopathy. Heart, Lung and Circulation 2016; 25(3): 275-281. Doi: 10.1016/j.hlc.2015.08.019.
Mazzanti A., Ng K., Faragli A., Maragna R., et al. Arrhythmogenic right ventricular cardiomyopathy: clinical course and predictors of arrhythmic risk / JACC 2016; 68(23): 2540-2550. Doi: 10.1016/j.jacc.2016.09.951.
Santangeli P., Dello Russo A., Pieroni M., et al. Fragmented and delayed electrograms within fibrofatty scar predict arrhythmic events in arrhythmogenic right ventricular cardiomyopathy: Results from a prospective risk stratification study. Heart Rhythm 2012; 9(8): 1200-1206. Doi: 10.1016/j.hrthm.2012.03.057.
Hulot J.-S., Jouven X., Empana J.-P., et al. Natural history and risk stratification of arrhythmogenic right ventricular dysplasia/cardiomyopathy. Circulation 2004; 110(14): 1879-1884. Doi: 10.1161/01.CIR.0000143375.93288.82.
Corrado D., Leoni L., Link MS., et al. Implantable cardioverter-defibrillator therapy for prevention of sudden death in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circulation 2003; 108(25): 3084-3091. Doi: 10.1161/01.CIR.0000103130.33451.D2.
Wang W., Cadrin-Tourigny J., Bhonsale A., et al. Arrhythmic outcome of arrhythmogenic right ventricular cardiomyopathy patients without implantable defibrillators. Journal of Cardiovascular Electrophysiology 2018; 29(10): 1396-1402. Doi: 10.1111/jce.13668.
Link MS., Laidlaw D., Polonsky B., et al. Ventricular arrhythmias in the North American multidisciplinary study of ARVC: predictors, characteristics, and treatment. JACC 2014; 64(2): 119-125. Doi: 10.1016/j.jacc.2014.04.035.
Mahida S., Venlet J., Saguner A.M., et al. Ablation compared with drug therapy for recurrent ventricular tachycardia in arrhythmogenic right ventricular cardiomyopathy: results from a multicenter study. Heart Rhythm 2019; 16(4): 536-543. Doi: 10.1016/j.hrthm.2018.10.016.
Santangeli P., Zado E.S., Supple G.E., et al. Long-term outcome with catheter ablation of ventricular tachycardia in patients with arrhythmogenic right ventricular cardiomyopathy. Circ: Arrhythmia and Electrophysiology 2015; 8(6): 1413-1421. Doi: 10.1161/CIRCEP.115.003562.
Ommen SR., Mital S., Burke MA., et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic сardiomyopathy: executive summary: a report of the American College of Cardiology. American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2020; 142(25): e533-e557. Doi: 10.1161/CIR.0000000000000938.
Lorenzini M., Anastasiou Z., O’Mahony C., et al. Mortality among referral patients with hypertrophic cardiomyopathy vs the general European population. JAMA Cardiology 2020; 5(1): 73-80. Doi: 10.1001/jamacardio.2019.4534.
O’Mahony C., Jichi F., Ommen SR,. et al. International External Validation Study of the 2014 European Society of Cardiology Guidelines on Sudden Cardiac Death Prevention in Hypertrophic Cardiomyopathy (EVIDENCE-HCM). Circulation 2018; 137(10): 1015-1023. Doi: 10.1161/CIRCULATIONAHA.117.030437.
Vriesendorp PA., Schinkel AF., Liebregts M., Theuns DA., van Cleemput J., Ten Cate FJ., Willems R., Michels M. Validation of the 2014 European Society of Cardiology guidelines risk prediction model for the primary prevention of sudden cardiac death in hypertrophic cardiomyopathy. Circ Arrhythm Electrophysiol 2015; 8(4): 829-35. Doi: 10.1161/CIRCEP.114.002553.
O'Mahony C., Jichi F., Pavlou M., Monserrat L., Anastasakis A., Rapezzi C., Biagini E., Gimeno JR., Limongelli G., McKenna WJ., et al. A novel clinical risk prediction model for sudden cardiac death in hypertrophic cardiomyopathy (HCM risk-SCD). Eur Heart J 2014; 35(30): 2010-20. Doi: 10.1093/eurheartj/eht439.
Chan RH., Maron BJ., Olivotto I., Pencina MJ., Assenza GE., Haas T., Lesser JR., Gruner C., Crean AM., Rakowski H., et al. Prognostic value of quantitative contrast-enhanced cardiovascular magnetic resonance for the evaluation of sudden death risk in patients with hypertrophic cardiomyopathy. Circulation 2014; 130(6): 484-95. Doi: 10.1161/CIRCULATIONAHA.113.007094.
Smith BM., Dorfman AL., Yu S., Russell MW., Agarwal PP., Mahani MG., Lu JC. Clinical significance of late gadolinium enhancement in patients<20 years of age with hypertrophic cardiomyopathy. Am J Cardiol 2014; 113(7): 1234-9. Doi: 10.1016/j.amjcard.2013.12.034.
Miron A., Lafreniere-Roula M., Steve Fan CP., Armstrong KR., Dragulescu A., Papaz T., Manlhiot C., Kaufman B., Butts RJ., Gardin L., et al. A Validated Model for Sudden Cardiac Death Risk Prediction in Pediatric Hypertrophic Cardiomyopathy. Circulation 2020; 142(3): 217-229. Doi: 10.1161/CIRCULATIONAHA.
He D., Ye M., Zhang L., Jiang B. Prognostic significance of late gadolinium enhancement on cardiac magnetic resonance in patients with hypertrophic cardiomyopathy. Heart Lung 2018; 47(2): 122-126. Doi: 10.1016/j.hrtlng.2017.10.008.
Weissler-Snir A., Dorian P., Rakowski H., Care M., Spears D. Primary prevention implantable cardioverter-defibrillators in hypertrophic cardiomyopathy-Are there predictors of appropriate therapy? Heart Rhythm 2021; 18(1): 63-70. Doi: 10.1016/j.hrthm.2020.08.009.
Ho CY., Day SM., Ashley EA., Michels M., Pereira AC., Jacoby D., Cirino AL., Fox JC., Lakdawala NK., Ware JS., et al. Genotype and Lifetime Burden of Disease in Hypertrophic Cardiomyopathy: Insights from the Sarcomeric Human Cardiomyopathy Registry (SHaRe). Circulation 2018; 138(14): 1387-1398. Doi: 10.1161/CIRCULATIONAHA.117.033200.
Kim HY., Park JE., Lee SC., Jeon ES., On YK., Kim SM., Choe YH., Ki CS., Kim JW., Kim KH. Genotype-Related Clinical Characteristics and Myocardial Fibrosis and their Association with Prognosis in Hypertrophic Cardiomyopathy. J Clin Med 2020; 9(6): 1671. Doi: 10.3390/jcm9061671.
Maron BJ., Maron MS., Semsarian C. Double or compound sarcomere mutations in hypertrophic cardiomyopathy: a potential link to sudden death in the absence of conventional risk factors. Heart Rhythm 2012; 9(1): 57-63. Doi: 10.1016/j.hrthm.2011.08.009.
Rosmini S., Biagini E., O'Mahony C., Bulluck H., Ruozi N., Lopes LR., Guttmann O., Reant P., Quarta CC., Pantazis A., et al. Relationship between aetiology and left ventricular systolic dysfunction in hypertrophic cardiomyopathy. Heart 2017; 103(4): 300-306. Doi: 10.1136/heartjnl-2016-310138.
Wang J., Wang Y., Zou Y., Sun K., Wang Z., Ding H., Yuan J., Wei W., Hou Q., Wang H., et al. Malignant effects of multiple rare variants in sarcomere genes on the prognosis of patients with hypertrophic cardiomyopathy. Eur J Heart Fail 2014; 16(9): 950-7. Doi: 10.1002/ejhf.144.
Pelliccia A., Fagard R., Bjørnstad HH., Anastassakis A., Arbustini E., Assanelli D., Biffi A., Borjesson M., Carrè F., Corrado D., et al. Recommendations for competitive sports participation in athletes with cardiovascular disease: a consensus document from the Study Group of Sports Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur Heart J 2005; 26(14): 1422-45. Doi: 10.1093/eurheartj/ehi325.
Национальные Рекомендации по определению риска и профилактике внезапной сердечной смерти / Шляхто Е.В. и др. – Москва, 2008. – 167 с.
Norrish G., Ding T., Field E., Ziólkowska L., Olivotto I., Limongelli G., Anastasakis A., Weintraub R., Biagini E., Ragni L., et al. Development of a Novel Risk Prediction Model for Sudden Cardiac Death in Childhood Hypertrophic Cardiomyopathy (HCM Risk-Kids). JAMA Cardiol 2019; 4(9): 918-927. Doi: 10.1001/jamacardio.2019.2861.
Norrish G., Qu C., Field E., Cervi E., Khraiche D., Klaassen S., Ojala TH., Sinagra G., Yamazawa H., Marrone C., et al. External validation of the HCM Risk-Kids model for predicting sudden cardiac death in childhood hypertrophic cardiomyopathy. Eur J Prev Cardiol 2022; 29(4): 678-686. Doi: 10.1093/eurjpc/zwab181.
Elliott PM., Poloniecki J., Dickie S., Sharma S., Monserrat L., Varnava A., Mahon NG., McKenna WJ. Sudden death in hypertrophic cardiomyopathy: identification of high risk patients. J Am Coll Cardiol 2000; 36(7): 2212-8. Doi: 10.1016/s0735-1097(00)01003-2.
Rowin EJ., Maron BJ., Carrick RT., Patel PP., Koethe B., Wells S., Maron MS. Outcomes in Patients With Hypertrophic Cardiomyopathy and Left Ventricular Systolic Dysfunction. J Am Coll Cardiol 2020; 75(24): 3033-3043. Doi: 10.1016/j.jacc.2020.04.045.
Rowin EJ., Maron BJ., Haas TS., Garberich RF., Wang W., Link MS., Maron MS. Hypertrophic Cardiomyopathy With Left Ventricular Apical Aneurysm: Implications for Risk Stratification and Management. J Am Coll Cardiol. 2017 Feb 21;69(7):761-773. doi: 10.1016/j.jacc.2016.11.063. Erratum in: J Am Coll Cardiol 2017; 69(12): 1652. Doi: 10.1016/j.jacc.2017.02.014.
Sadoul N., Prasad K., Elliott PM., Bannerjee S., Frenneaux MP., McKenna WJ. Prospective prognostic assessment of blood pressure response during exercise in patients with hypertrophic cardiomyopathy. Circulation 1997; 96(9): 2987-91. Doi: 10.1161/01.cir.96.9.2987.
Cecchi F., Maron BJ., Epstein SE. Long-term outcome of patients with hypertrophic cardiomyopathy successfully resuscitated after cardiac arrest. J Am Coll Cardiol 1989; 13(6): 1283-8. Doi: 10.1016/0735-1097(89)90302-1.
Elliott PM., Sharma S., Varnava A., Poloniecki J., Rowland E., McKenna WJ. Survival after cardiac arrest or sustained ventricular tachycardia in patients with hypertrophic cardiomyopathy. J Am Coll Cardiol 1999; 33(6): 1596-601. Doi: 10.1016/s0735-1097(99)00056-x.
Maron BJ., Spirito P., Shen WK., Haas TS., Formisano F., Link MS., Epstein AE., Almquist AK., Daubert JP., Lawrenz T., et al. Implantable cardioverter-defibrillators and prevention of sudden cardiac death in hypertrophic cardiomyopathy. JAMA 2007; 298(4): 405-12. Doi: 10.1001/jama.298.4.405.
McKenna WJ., Oakley CM., Krikler DM., Goodwin JF. Improved survival with amiodarone in patients with hypertrophic cardiomyopathy and ventricular tachycardia. Br Heart J 1985; 53(4): 412-6. Doi: 10.1136/hrt.53.4.412.
Melacini P., Maron BJ., Bobbo F., Basso C., Tokajuk B., Zucchetto M., Thiene G., Iliceto S. Evidence that pharmacological strategies lack efficacy for the prevention of sudden death in hypertrophic cardiomyopathy. Heart 2007; 93(6): 708-10. Doi: 10.1136/hrt.2006.099416.
Dukkipati SR., d'Avila A., Soejima K., Bala R., Inada K., Singh S., Stevenson WG., Marchlinski FE., Reddy VY. Long-term outcomes of combined epicardial and endocardial ablation of monomorphic ventricular tachycardia related to hypertrophic cardiomyopathy. Circ Arrhythm Electrophysiol 2011; 4(2): 185-94. Doi: 10.1161/CIRCEP.110.957290.
Igarashi M., Nogami A., Kurosaki K., Hanaki Y., Komatsu Y., Fukamizu S., Morishima I., Kaitani K., Nishiuchi S., Talib AK., et al. Radiofrequency Catheter Ablation of Ventricular Tachycardia in Patients With Hypertrophic Cardiomyopathy and Apical Aneurysm. JACC Clin Electrophysiol 2018; 4(3): 339-350. Doi: 10.1016/j.jacep.2017.12.020.
Kristen AV., Dengler TJ., Hegenbart U., Schonland SO., Goldschmidt H., Sack FU., Voss F., Becker R., Katus HA., Bauer A. Prophylactic implantation of cardioverter-defibrillator in patients with severe cardiac amyloidosis and high risk for sudden cardiac death. Heart Rhythm 2008; 5(2): 235-40. Doi: 10.1016/j.hrthm.2007.10.016.
Shah MJ., Silka MJ., Silva JNA., Balaji S., Beach CM., Benjamin MN., Berul CI., Cannon B., Cecchin F., Cohen MI., et al. 2021 PACES expert consensus statement on the indications and management of cardiovascular implantable electronic devices in pediatric patients: Developed in collaboration with and endorsed by the Heart Rhythm Society (HRS), the American College of Cardiology (ACC), the American Heart Association (AHA), and the Association for European Paediatric and Congenital Cardiology (AEPC). Endorsed by the Asia Pacific Heart Rhythm Society (APHRS), the Indian Heart Rhythm Society (IHRS), and the Latin American Heart Rhythm Society (LAHRS). Cardiology in the Young 2021; 31(11): 1738-1769. Doi: 10.1017/S1047951121003413.
Bucci E., Testa M., Licchelli L., Frattari A., El Halabieh NA., Gabriele E., Pignatelli G., De Santis T., Fionda L., Vanoli F., et al. A 34-year longitudinal study on long-term cardiac outcomes in DM1 patients with normal ECG at baseline at an Italian clinical centre. J Neurol 2018; 265(4): 885-895. Doi: 10.1007/s00415-018-8773-3.
Breton R., Mathieu J. Usefulness of clinical and electrocardiographic data for predicting adverse cardiac events in patients with myotonic dystrophy. Can J Cardiol 2009; 25(2): e23-7. Doi: 10.1016/s0828-282x(09)70479-9.
Fayssoil A., Abasse S., Silverston K. Cardiac Involvement Classification and Therapeutic Management in Patients with Duchenne Muscular Dystrophy. J Neuromuscul Dis 2017; 4(1): 17-23. Doi: 10.3233/JND-160194.
Клинические рекомендации. Прогрессирующая мышечная дистрофия Дюшенна. Прогрессирующая мышечная дистрофия Беккера. Категория Дети. 2024.
Bhakta D., Groh MR., Shen C., Pascuzzi RM., Groh WJ. Increased mortality with left ventricular systolic dysfunction and heart failure in adults with myotonic dystrophy type 1. Am Heart J 2010; 160(6): 1137-41, 1141.e1. Doi: 10.1016/j.ahj.2010.07.032.
Merino JL., Carmona JR., Fernández-Lozano I., Peinado R., Basterra N., Sobrino JA. Mechanisms of sustained ventricular tachycardia in myotonic dystrophy: implications for catheter ablation. Circulation 1998; 98(6): 541-6. Doi: 10.1161/01.cir.98.6.541.
Wahbi K., Meune C., Porcher R., Bécane HM., Lazarus A., Laforêt P., Stojkovic T., Béhin A., Radvanyi-Hoffmann H., Eymard B., et al. Electrophysiological study with prophylactic pacing and survival in adults with myotonic dystrophy and conduction system disease. JAMA 2012; 307(12): 1292-301. Doi: 10.1001/jama.2012.346.
Sanna T., Dello Russo A., Toniolo D., Vytopil M., Pelargonio G., De Martino G., Ricci E., Silvestri G., Giglio V., Messano L., et al. Cardiac features of Emery-Dreifuss muscular dystrophy caused by lamin A/C gene mutations. Eur Heart J 2003; 24(24): 2227-36. Doi: 10.1016/j.ehj.2003.09.020.
Menon SC., Etheridge SP., Liesemer KN., Williams RV., Bardsley T., Heywood MC., Puchalski MD. Predictive value of myocardial delayed enhancement in Duchenne muscular dystrophy. Pediatr Cardiol 2014; 35(7): 1279-85. Doi: 10.1007/s00246-014-0929-z.
Prystowsky EN., Pritchett EL., Roses AD., Gallagher J. The natural history of conduction system disease in myotonic muscular dystrophy as determined by serial electrophysiologic studies. Circulation 1979; 60(6): 1360-4. Doi: 10.1161/01.cir.60.6.1360.
Rajdev A., Groh WJ. Arrhythmias in the muscular dystrophies. Card Electrophysiol Clin 2015; 7(2): 303-8. Doi: 10.1016/j.ccep.2015.03.011.
Shah Z, Mohammed M., Vuddanda V., Ansari M.W. National trends, gender, management, and outcomes of patients hospitalized for myocarditis. The American Journal of Cardiology 2019; 124(1): 131-136. Doi: 10.1016/j.amjcard.2019.03.036.
Rosier L., Zouaghi A., Barré V., Martins R., et al. High risk of sustained ventricular arrhythmia recurrence after acute myocarditis. Journal of Clinical Medicine 2020; 9(3): 848. Doi: 10.3390/jcm9030848.
Vaseghi M., Hu T.Y., Tung R., Vergara P., et al. Outcomes of catheter ablation of ventricular tachycardia based on etiology in nonischemic heart disease: an international ventricular tachycardia ablation center collaborative study. JACC 2018; 4(9): 1141-1150. Doi: 10.1016/j.jacep.2018.05.007.
Kandolin R., Lehtonen J., Airaksinen J., et al. Cardiac sarcoidosis: epidemiology, characteristics, and outcome over 25 years in a nationwide study. Circulation 2015; 131(7): 624-632. Doi: 10.1161/CIRCULATIONAHA.114.011522.
Nordenswan H.-K., Lehtonen J., Ekström K., Kandolin R., et al. Outcome of cardiac sarcoidosis presenting with high-grade atrioventricular block. Circulation: Arrhythmia and Electrophysiology 2018; 11(8): e006145. Doi: 10.1161/CIRCEP.117.006145.
Greulich S., Deluigi CC., Gloekler S., et al. CMR imaging predicts death and other adverse events in suspected cardiac sarcoidosis. JACC 2013; 6(4): 501-511. Doi: 10.1016/j.jcmg.2012.10.021.
Mehta D., Mori N., Goldbarg S.H., et al. Primary prevention of sudden cardiac death in silent cardiac sarcoidosis: role of programmed ventricular stimulation. Circ: Arrhythmia and Electrophysiology 2011; 4(1): 43-48. Doi: 10.1161/CIRCEP.110.958322.
Robinson M.L., Kobayashi T., Higgins Y., et al. Lyme carditis. Infectious Disease Clinics of North America 2015; 29(2): 255-268. Doi: 10.1016/j.idc.2015.02.003.
Kostić T. , Momčilović S., Perišić Z.D., et al. Manifestations of Lyme carditis. International Journal of Cardiology 2017; 232: 24-32. Doi: 10.1016/j.ijcard.2016.12.169.
Nagi K.S., Joshi R., Thakur R.K. Cardiac manifestations of Lyme disease: a review. Canadian Journal of Cardiology 1996;12(5): 503-506.
Esfandiar N., Beebe-Peat T., Quinlan A., et al. Lyme carditis complicated by polymorphic ventricular tachycardia and cardiac arrest: a case report. Journal of Investigative Medicine High Impact Case Reports 2022; 10: 23247096221098333. Doi: 10.1177/23247096221098333.
Stein C., Migliavaca C.B., Colpani V., et al. Amiodarone for arrhythmia in patients with chagas disease: a systematic review and individual patient data meta-analysis. PLOS Neglected Tropical Diseases 2018; 12(8): e0006742. Doi: 10.1371/journal.pntd.0006742.
Soto-Becerra R., Bazan V., Bautista W., et al. Ventricular tachycardia in the setting of chagasic cardiomyopathy: use of voltage mapping to characterize endoepicardial nonischemic scar distribution. Circulation: Arrhythmia and Electrophysiology 2017; 10(11): e004950. Doi: 10.1161/CIRCEP.116.004950.
Rassi FM, Minohara L., Rassi A., et al. Systematic review and meta-analysis of clinical outcome after implantable cardioverter-defibrillator therapy in patients with chagas heart disease. JACC: Clinical Electrophysiology 2019; 5(10): 1213-1223. Doi: 10.1016/j.jacep.2019.07.003
Eckart RE, Hruczkowski TW, Tedrow UB., et al. Sustained ventricular tachycardia associated with corrective valve surgery. Circulation 2007; 116(18): 2005-2011. Doi: 10.1161/CIRCULATIONAHA.107.703157
Rodríguez-Mañero M., Barrio-López MT, Assi EA., et al. Primary prevention of sudden death in patients with valvular cardiomyopathy. Revista Española de Cardiología (Engl Ed) 2016; 69(3): 272-278. Doi: 10.1016/j.rec.2015.05.016.
Sadek MM., Benhayon D., Sureddi R., Chik W., Santangeli P., Supple GE., Hutchinson MD., Bala R., Carballeira L., Zado ES., et al. Idiopathic ventricular arrhythmias originating from the moderator band: Electrocardiographic characteristics and treatment by catheter ablation. Heart Rhythm 2015; 12(1): 67-75. Doi: 10.1016/j.hrthm.2014.08.029.
Andersen ED., Krasilnikoff PA., Overvad H. Intermittent muscular weakness, extrasystoles, and multiple developmental anomalies. A new syndrome? Acta Paediatr Scand 1971; 60(5): 559-64. Doi: 10.1111/j.1651-2227.1971.tb06990.x.
Tawil R., Ptacek LJ., Pavlakis SG., DeVivo DC., Penn AS., Ozdemir C., Griggs RC. Andersen's syndrome: potassium-sensitive periodic paralysis, ventricular ectopy, and dysmorphic features. Ann Neurol 1994; 35(3): 326-30. Doi: 10.1002/ana.410350313.
Splawski I., Timothy KW., Decher N., Kumar P., Sachse FB., Beggs AH., Sanguinetti MC., Keating MT. Severe arrhythmia disorder caused by cardiac L-type calcium channel mutations. Proc Natl Acad Sci U S A 2005; 102(23): 8089-96; discussion 8086-8. Doi: 10.1073/pnas.0502506102.
JERVELL A., LANGE-NIELSEN F. Congenital deaf-mutism, functional heart disease with prolongation of the Q-T interval and sudden death. Am Heart J 1957; 54(1): 59-68. Doi: 10.1016/0002-8703(57)90079-0.
Schwartz PJ., Moss AJ., Vincent GM., Crampton RS. Diagnostic criteria for the long QT syndrome. An update. Circulation 1993; 88(2): 782-4. Doi: 10.1161/01.cir.88.2.782.
Schwartz PJ., Crotti L. QTc behavior during exercise and genetic testing for the long-QT syndrome. Circulation 2011; 124(20): 2181-4. Doi: 10.1161/CIRCULATIONAHA.111.062182.
Jons C., Moss AJ., Goldenberg I., Liu J., McNitt S., Zareba W., Qi M., Robinson JL. Risk of fatal arrhythmic events in long QT syndrome patients after syncope. J Am Coll Cardiol 2010; 55(8): 783-8. Doi: 10.1016/j.jacc.2009.11.042.
Schwartz PJ., Priori SG., Spazzolini C., Moss AJ., Vincent GM., Napolitano C., Denjoy I., Guicheney P., Breithardt G., Keating MT., et al. Genotype-phenotype correlation in the long-QT syndrome: gene-specific triggers for life-threatening arrhythmias. Circulation 2001; 103(1): 89-95. Doi: 10.1161/01.cir.103.1.89.
Priori SG., Napolitano C., Schwartz PJ., Grillo M., Bloise R., Ronchetti E., Moncalvo C., Tulipani C., Veia A., Bottelli G., et al. Association of long QT syndrome loci and cardiac events among patients treated with beta-blockers. JAMA 2004; 292(11): 1341-4. Doi: 10.1001/jama.292.11.1341.
Schwartz PJ., Woosley RL. Predicting the Unpredictable: Drug-Induced QT Prolongation and Torsades de Pointes. J Am Coll Cardiol 2016; 67(13): 1639-1650. Doi: 10.1016/j.jacc.2015.12.063.
Kannankeril P., Roden DM., Darbar D. Drug-induced long QT syndrome. Pharmacol Rev 2010; 62(4): 760-81. Doi: 10.1124/pr.110.003723.
Ahn J., Kim HJ., Choi JI., Lee KN., Shim J., Ahn HS., Kim YH. Effectiveness of beta-blockers depending on the genotype of congenital long-QT syndrome: A meta-analysis. PLoS One 2017; 12(10): e0185680. Doi: 10.1371/journal.pone.0185680.
Went TR., Sultan W., Sapkota A., Khurshid H., Qureshi IA., Jahan N., Tara A., Win M., Wiltshire DA., Kannan A., et al. A Systematic Review on the Role of Βeta-Blockers in Reducing Cardiac Arrhythmias in Long QT Syndrome Subtypes 1-3. Cureus 2021; 13(9): e17632. Doi: 10.7759/cureus.17632.
Yoshinaga M., Kucho Y., Sarantuya J., Ninomiya Y., Horigome H., Ushinohama H., Shimizu W., Horie M. Genetic characteristics of children and adolescents with long-QT syndrome diagnosed by school-based electrocardiographic screening programs. Circ Arrhythm Electrophysiol 2014; 7(1): 107-12. Doi: 10.1161/CIRCEP.113.000426.
Rodríguez-Mañero M., Casado-Arroyo R., Sarkozy A., Leysen E., et al. The clinical significance of pregnancy in Brugada syndrome. Revista Española de Cardiología (Engl Ed) 2014; 67(3): 176-180. Doi: 10.1016/j.rec.2013.06.023.
578 Gupta T., Khera S., Kolte D., Aronow WS., Iwai S. Antiarrhythmic properties of ranolazine: A review of the current evidence. Int J Cardiol 2015; 187: 66-74. Doi: 10.1016/j.ijcard.2015.03.324.
579 Bunch TJ., Mahapatra S., Murdock D., Molden J., Weiss JP., May HT., Bair TL., Mader KM., Crandall BG., Day JD., et al. Ranolazine reduces ventricular tachycardia burden and ICD shocks in patients with drug-refractory ICD shocks. Pacing Clin Electrophysiol 2011; 34(12): 1600-6. Doi: 10.1111/j.1540-8159.2011.03208.x.
Zareba W, Daubert JP, Beck CA, Huang DT, Alexis JD, Brown MW, Pyykkonen K, McNitt S, Oakes D, Feng C, Aktas MK, Ayala-Parades F, Baranchuk A, Dubuc M, Haigney M, Mazur A, McPherson CA, Mitchell LB, Natale A, Piccini JP, Raitt M, Rashtian MY, Schuger C, Winters S, Worley SJ, Ziv O, Moss AJ; RAID Trial Investigators. Ranolazine in High-Risk Patients With Implanted Cardioverter-Defibrillators: The RAID Trial. J Am Coll Cardiol. 2018 Aug 7;72(6):636-645.
Ruan Y., Liu N., Bloise R., Napolitano C., Priori SG. Gating properties of SCN5A mutations and the response to mexiletine in long-QT syndrome type 3 patients. Circulation 2007; 116(10): 1137-44. Doi: 10.1161/CIRCULATIONAHA.107.707877.
Moss AJ., Zareba W., Schwarz KQ., Rosero S., McNitt S., Robinson JL. Ranolazine shortens repolarization in patients with sustained inward sodium current due to type-3 long-QT syndrome. J Cardiovasc Electrophysiol 2008; 19(12): 1289-93. Doi: 10.1111/j.1540-8167.2008.01246.x.
Chorin E., Hu D., Antzelevitch C., Hochstadt A., Belardinelli L., Zeltser D., Barajas-Martinez H., Rozovski U., Rosso R., Adler A., et al. Ranolazine for Congenital Long-QT Syndrome Type III: Experimental and Long-Term Clinical Data. Circ Arrhythm Electrophysiol 2016; 9(10): e004370. Doi: 10.1161/CIRCEP.116.004370.
Chorin E., Taub R., Medina A., Flint N., Viskin S., Benhorin J. Long-term flecainide therapy in type 3 long QT syndrome. Europace 2018; 20(2): 370-376. Doi: 10.1093/europace/euw439.
Windle JR., Geletka RC., Moss AJ., Zareba W., Atkins DL. Normalization of ventricular repolarization with flecainide in long QT syndrome patients with SCN5A: DeltaKPQ mutation. Ann Noninvasive Electrocardiol 2001; 6(2): 153-8. Doi: 10.1111/j.1542-474x.2001.tb00100.x.
Umeda M., Morimoto A., Yokoyama K., Tateishi E., Makino K., Yamamoto K., Nakagawa Y., Fukuhara S., Takase E. [Despite medication, overdrive pacing is required to stabilize the electrical storm associated with acute coronary syndrome: a case report]. J Cardiol 2007; 50(4): 263-9.
Yoshida T., Naito Y., Nishimura K. Temporary ventricular overdrive pacing for electrical storm after coronary artery bypass grafting. Gen Thorac Cardiovasc Surg 2011; 59(11): 756-9. Doi: 10.1007/s11748-010-0771-z.
Schwartz PJ., Spazzolini C., Priori SG., Crotti L., Vicentini A., Landolina M., Gasparini M., Wilde AA., Knops RE., Denjoy I., et al. Who are the long-QT syndrome patients who receive an implantable cardioverter-defibrillator and what happens to them?: data from the European Long-QT Syndrome Implantable Cardioverter-Defibrillator (LQTS ICD) Registry. Circulation 2010; 122(13): 1272-82. Doi: 10.1161/CIRCULATIONAHA.110.950147.
Ajijola OA., Lellouche N., Bourke T., Tung R., Ahn S., Mahajan A., Shivkumar K. Bilateral cardiac sympathetic denervation for the management of electrical storm. J Am Coll Cardiol 2012; 59(1): 91-2. Doi: 10.1016/j.jacc.2011.09.043.
Schwartz PJ., Priori SG., Locati EH., Napolitano C., Cantù F., Towbin JA., Keating MT., Hammoude H., Brown AM., Chen LS., et al. Long QT syndrome patients with mutations of the SCN5A and HERG genes have differential responses to Na+ channel blockade and to increases in heart rate. Implications for gene-specific therapy. Circulation 1995; 92(12): 3381-6. Doi: 10.1161/01.cir.92.12.3381.
Hofferberth SC., Cecchin F., Loberman D., Fynn-Thompson F. Left thoracoscopic sympathectomy for cardiac denervation in patients with life-threatening ventricular arrhythmias. J Thorac Cardiovasc Surg 2014; 147(1): 404-9. Doi: 10.1016/j.jtcvs.2013.07.064.
Gollob MH., Redpath CJ., Roberts JD. The short QT syndrome: proposed diagnostic criteria. J Am Coll Cardiol 2011; 57(7): 802-12. Doi: 10.1016/j.jacc.2010.09.048.
Suzuki H., Horie M., Ozawa J., Sumitomo N., Ohno S., Hoshino K., Ehara E., Takahashi K., Maeda Y., Yoshinaga M., et al. Novel electrocardiographic criteria for short QT syndrome in children and adolescents. Europace 2021; 23(12): 2029-2038. Doi: 10.1093/europace/euab097.
Giustetto C., Schimpf R., Mazzanti A., Scrocco C., Maury P., Anttonen O., Probst V., Blanc JJ., Sbragia P., Dalmasso P., et al. Long-term follow-up of patients with short QT syndrome. J Am Coll Cardiol 2011; 58(6): 587-95. Doi: 10.1016/j.jacc.2011.03.038.
Dewi IP., Dharmadjati BB. Short QT syndrome: The current evidences of diagnosis and management. J Arrhythm 2020; 36(6): 962-966. Doi: 10.1002/joa3.12439.
Mazzanti A., Kanthan A., Monteforte N., Memmi M., Bloise R., Novelli V., Miceli C., O'Rourke S., Borio G., Zienciuk-Krajka A., et al. Novel insight into the natural history of short QT syndrome. J Am Coll Cardiol 2014; 63(13): 1300-1308. Doi: 10.1016/j.jacc.2013.09.078.
Gaita F., Giustetto C., Bianchi F., Wolpert C., et al. Short QT syndrome: a familial cause of sudden death. Circulation 2003; 108(8): 965-970. Doi: 10.1161/01.CIR.0000085071.28695.C4.
Gaita F., Giustetto C., Bianchi F., et al. Short QT syndrome: pharmacological treatment. JACC 2004; 43(8): 1494-1499. Doi: 10.1016/j.jacc.2004.02.034.
Priori SG., Napolitano C., Gasparini M., et al. Natural history of Brugada syndrome: insights for risk stratification and management. Circulation 2002; 105(11): 1342-1347. Doi: 10.1161/hc1102.105288.
Maury P., Hocini M., Haissaguerre M. Electrical storms in Brugada syndrome: review of pharmacologic and ablative therapeutic options. Indian Pacing Electrophysiology. 2005; 5(1): 25-34.
Marquez MF., Bonny A., Hemandez-Castillo E., et al. Long-term efficacy of low doses of quinidine on malignant arrhythmias in Brugada syndrome with an implantable cardioverter-defibrillator: a case series and literature review. Heart Rhythm 2012; 9(12): 1995-2000. Doi: 10.1016/j.hrthm.2012.08.027.
Brugada J., Brugada R., Brugada P. Determinants of sudden cardiac death in individuals with the electrocardiographic pattern of Brugada syndrome and no previous cardiac arrest. Circulation 2003; 108(25): 3092-3096. Doi: 10.1161/01.CIR.0000104568.13957.4F.
Nademanee K., Veerakul G., Chandanamattha P., et al. Prevention of ventricular fibrillation episodes in Brugada syndrome by catheter ablation over the anterior right ventricular outflow tract epicardium. Circulation 2011; 123(12): 1270-1279. Doi: 10.1161/CIRCULATIONAHA.110.972612.
Argenziano M., Antzelevitch C. Recent advances in the treatment of Brugada syndrome. Expert Review of Cardiovascular Therapy 2018; 16(6): 387-404. Doi: 10.1080/14779072.2018.1475230.
Haissaguerre M., Extramiana F., Hocini M., et al. Mapping and ablation of ventricular fibrillation associated with Long-QT and Brugada syndromes. Circulation 2003; 108(8): 925-928. Doi: 10.1161/01.CIR.0000088781.99943.95.
Nademanee K., Haissaguerre M., Hocini M., et al. Mapping and ablation of ventricular fibrillation associated with early repolarization syndrome. Circulation 2019; 140(18): 1477-1490. Doi: 10.1161/CIRCULATIONAHA.118.039022.
Leenhardt A., Lucet V., Denjoy I., et al. Catecholaminergic Polymorphic Ventricular Tachycardia in Children A 7-Year Follow-up of 21 Patients. Circulation 1995; 91(5): 1512-1519. Doi: 10.1161/01.cir.91.5.1512.
Макаров Л.М., Курылева Т.А., Чупрова С.Н. Укорочение интервала PR, брадикардия и полиморфная желудочковая тахикардия. Клинико-электрокардиографический синдром с высоким риском внезапной смерти у детей. Кардиология 2003; 7: 34-37.
Makarov L., Kyrileva T., Komoliatova T., et al. New ECG pattern in young patients with polymorphic catecholaminergic ventricular tachycardia. JACC 2007; 49 (9): 916-242.
Priori SG., Napolitano C., Memmi M., et al. Clinical and molecular characterization of patients with catecholaminergic polymorphic ventricular tachycardia / Priori S.G., Napolitano C., Memmi M. et al. Circulation 2002; 106(1): 69-74. Doi: 10.1161/01.cir.0000020013.73106.d8.
Hayashi M., Denjoy I., Extramiana F., et al Incidence and risk factors of arrhythmic events in catecholaminergic polymorphic ventricutar tachycardia. Circulation 2009; 119(18): 2426-2434. Doi: 10.1161/CIRCULATIONAHA.108.829267.
Watanabe H., Chopra N., Laver D., Hwang HS., Davies SS., Roach DE., Duff HJ., Roden DM., Wilde AA., Knollmann BC. Flecainide prevents catecholaminergic polymorphic ventricular tachycardia in mice and humans. Nat Med 2009; 15(4): 380-3. Doi: 10.1038/nm.1942.
Beaufort-Krol GC., Dijkstra SS., Bink-Boelkens MT. Natural history of ventricular premature contractions in children with a structurally normal heart: does origin matter? Europace 2008; 10(8): 998-1003. Doi: 10.1093/europace/eun121.
Khairy P., Harris L., Landzberg MJ., Viswanathan S., Barlow A., Gatzoulis MA., Fernandes SM., Beauchesne L., Therrien J., Chetaille P., et al. Implantable cardioverter-defibrillators in tetralogy of Fallot. Circulation 2008; 117(3): 363-70. Doi: 10.1161/CIRCULATIONAHA.107.726372.
Berul CI., Van Hare GF., Kertesz NJ., Dubin AM., Cecchin F., Collins KK., Cannon BC., Alexander ME., Triedman JK., Walsh EP., et al. Results of a multicenter retrospective implantable cardioverter-defibrillator registry of pediatric and congenital heart disease patients. J Am Coll Cardiol 2008; 51(17): 1685-91. Doi: 10.1016/j.jacc.2008.01.033.
Koyak Z., de Groot JR., Van Gelder IC., Bouma BJ., van Dessel PF., Budts W., van Erven L., van Dijk AP., Wilde AA., Pieper PG., et al. Implantable cardioverter defibrillator therapy in adults with congenital heart disease: who is at risk of shocks? Circ Arrhythm Electrophysiol 2012; 5(1): 101-10. Doi: 10.1161/CIRCEP.111.966754.
Gallego P., Gonzalez AE., Sanchez-Recalde A., Peinado R., Polo L., Gomez-Rubin C., Lopez-Sendon JL., Oliver JM. Incidence and predictors of sudden cardiac arrest in adults with congenital heart defects repaired before adult life. Am J Cardiol 2012; 110(1): 109-17. Doi: 10.1016/j.amjcard.2012.02.057.
Ghai A., Silversides C., Harris L., Webb GD., Siu SC., Therrien J. Left ventricular dysfunction is a risk factor for sudden cardiac death in adults late after repair of tetralogy of Fallot. J Am Coll Cardiol 2002; 40(9): 1675-80. Doi: 10.1016/s0735-1097(02)02344-6.
Gatzoulis MA., Balaji S., Webber SA., Siu SC., Hokanson JS., Poile C., Rosenthal M., Nakazawa M., Moller JH., Gillette PC., et al. Risk factors for arrhythmia and sudden cardiac death late after repair of tetralogy of Fallot: a multicentre study. Lancet 2000; 356(9234): 975-81. Doi: 10.1016/S0140-6736(00)02714-8.
Khairy P., Landzberg MJ., Gatzoulis MA., Lucron H., Lambert J., Marçon F., Alexander ME., Walsh EP. Value of programmed ventricular stimulation after tetralogy of fallot repair: a multicenter study. Circulation 2004; 109(16): 1994-2000. Doi: 10.1161/01.CIR.0000126495.11040.BD.
Khairy P., Harris L., Landzberg MJ., Fernandes SM., Barlow A., Mercier LA., Viswanathan S., Chetaille P., Gordon E., Dore A., et al. Sudden death and defibrillators in transposition of the great arteries with intra-atrial baffles: a multicenter study. Circ Arrhythm Electrophysiol 2008; 1(4): 250-7. Doi: 10.1161/CIRCEP.108.776120.
Koyak Z., Harris L., de Groot JR., Silversides CK., Oechslin EN., Bouma BJ., Budts W., Zwinderman AH., Van Gelder IC., Mulder BJ. Sudden cardiac death in adult congenital heart disease. Circulation 2012; 126(16): 1944-54. Doi: 10.1161/CIRCULATIONAHA.112.104786.
Atallah J., Gonzalez Corcia MC., Walsh EP.; Participating Members of the Pediatric and Congenital Electrophysiology Society. Ventricular Arrhythmia and Life-Threatening Events in Patients With Repaired Tetralogy of Fallot. Am J Cardiol 2020; 132: 126-132. Doi: 10.1016/j.amjcard.2020.07.012.
Koyak Z., de Groot JR., Bouma BJ., Van Gelder IC., Budts W., Zwinderman AH., Mulder BJ. Symptomatic but not asymptomatic non-sustained ventricular tachycardia is associated with appropriate implantable cardioverter therapy in tetralogy of Fallot. Int J Cardiol 2013; 167(4): 1532-5. Doi: 10.1016/j.ijcard.2012.04.103.
Sabate Rotes A., Connolly HM., Warnes CA., Ammash NM., Phillips SD., Dearani JA., Schaff HV., Burkhart HM., Hodge DO., Asirvatham SJ., et al. Ventricular arrhythmia risk stratification in patients with tetralogy of Fallot at the time of pulmonary valve replacement. Circ Arrhythm Electrophysiol 2015; 8(1): 110-6. Doi: 10.1161/CIRCEP.114.001975.
Miyazaki A., Sakaguchi H., Ohuchi H., Matsuoka M., Komori A., Yamamoto T., Yasuda K., Satomi K., Hoashi T., Kamakura S., Yamada O. Efficacy of hemodynamic-based management of tachyarrhythmia after repair of tetralogy of Fallot. Circ J 2012; 76(12): 2855-62. Doi: 10.1253/circj.cj-12-0208.
Harrison DA., Harris L., Siu SC., MacLoghlin CJ., Connelly MS., Webb GD., Downar E., McLaughlin PR., Williams WG. Sustained ventricular tachycardia in adult patients late after repair of tetralogy of Fallot. J Am Coll Cardiol 1997; 30(5): 1368-73. Doi: 10.1016/s0735-1097(97)00316-1.
van Zyl M., Kapa S., Padmanabhan D., Chen FC., Mulpuru SK., Packer DL., Munger TM., Asirvatham SJ., McLeod CJ. Mechanism and outcomes of catheter ablation for ventricular tachycardia in adults with repaired congenital heart disease. Heart Rhythm 2016; 13(7): 1449-54. Doi: 10.1016/j.hrthm.2016.03.002.
Laredo M., Frank R., Waintraub X., Gandjbakhch E., Iserin L., Hascoët S., Himbert C., Gallais Y., Hidden-Lucet F., Duthoit G. Ten-year outcomes of monomorphic ventricular tachycardia catheter ablation in repaired tetralogy of Fallot. Arch Cardiovasc Dis 2017; 110(5): 292-302. Doi: 10.1016/j.acvd.2017.01.009.
Kapel GF., Reichlin T., Wijnmaalen AP., Piers SR., Holman ER., Tedrow UB., Schalij MJ., Stevenson WG., Zeppenfeld K. Re-entry using anatomically determined isthmuses: a curable ventricular tachycardia in repaired congenital heart disease. Circ Arrhythm Electrophysiol 2015; 8(1): 102-9. Doi: 10.1161/CIRCEP.114.001929.
Kapel GF., Sacher F., Dekkers OM., Watanabe M., Blom NA., Thambo JB., Derval N., Schalij MJ., Jalal Z., Wijnmaalen AP., et al. Arrhythmogenic anatomical isthmuses identified by electroanatomical mapping are the substrate for ventricular tachycardia in repaired Tetralogy of Fallot. Eur Heart J 2017; 38(4): 268-276. Doi: 10.1093/eurheartj/ehw202.
Zeppenfeld K., Schalij MJ., Bartelings MM., Tedrow UB., Koplan BA., Soejima K., Stevenson WG. Catheter ablation of ventricular tachycardia after repair of congenital heart disease: electroanatomic identification of the critical right ventricular isthmus. Circulation 2007; 116(20): 2241-52. Doi: 10.1161/CIRCULATIONAHA.
Collins KK., Schaffer MS., Liberman L., Saarel E., Knecht M., Tanel RE., Bradley D., Dubin AM., Paul T., Salerno J., et al. Pediatric and Congenital Electrophysiology Society. Fascicular and nonfascicular left ventricular tachycardias in the young: an international multicenter study. J Cardiovasc Electrophysiol 2013; 24(6): 640-8. Doi: 10.1111/jce.12105.
Schneider HE., Kriebel T., Jung K., Gravenhorst VD., Paul T. Catheter ablation of idiopathic left and right ventricular tachycardias in the pediatric population using noncontact mapping. Heart Rhythm 2010; 7(6): 731-9. Doi: 10.1016/j.hrthm.2010.02.031.
Kammeraad JA., van Deurzen CH., Sreeram N., Bink-Boelkens MT., Ottenkamp J., Helbing WA., Lam J., Sobotka-Plojhar MA., Daniels O., Balaji S. Predictors of sudden cardiac death after Mustard or Senning repair for transposition of the great arteries. J Am Coll Cardiol 2004; 44(5): 1095-102. Doi: 10.1016/j.jacc.2004.05.073.
Seth R., Moss AJ., McNitt S., Zareba W., Andrews ML., Qi M., Robinson JL., Goldenberg I., Ackerman MJ., Benhorin J., et al. Long QT syndrome and pregnancy. J Am Coll Cardiol 2007; 49(10): 1092-8. Doi: 10.1016/j.jacc.2006.09.054.
Rashba EJ., Zareba W., Moss AJ., Hall WJ., Robinson J., Locati EH., Schwartz PJ., Andrews M. Influence of pregnancy on the risk for cardiac events in patients with hereditary long QT syndrome. LQTS Investigators. Circulation 1998; 97(5): 451-6. Doi: 10.1161/01.cir.97.5.451.
Ishibashi K., Aiba T., Kamiya C., Miyazaki A., Sakaguchi H., Wada M., Nakajima I., Miyamoto K., Okamura H., Noda T., et al. Arrhythmia risk and β-blocker therapy in pregnant women with long QT syndrome. Heart 2017; 103(17): 1374-1379. Doi: 10.1136/heartjnl-2016-310617.
Cheung CC., Lieve KV., Roston TM., van der Ree MH., Deyell MW., Andrade JG., Laksman ZW., Nannenberg EA., Tadros R., Pang B., et al. Pregnancy in Catecholaminergic Polymorphic Ventricular Tachycardia. JACC Clin Electrophysiol 2019; 5(3): 387-394. Doi: 10.1016/j.jacep.2018.10.019.
Wu L., Liang E., Fan S., Zheng L., Hu F., Liu S., Liu L., Hu Z., Li G., Yao Y. Effect of Pregnancy in Arrhythmogenic Right Ventricular Cardiomyopathy. Am J Cardiol 2020; 125(4): 613-617. Doi: 10.1016/j.amjcard.2019.11.008.
Bauce B., Daliento L., Frigo G., Russo G., Nava A. Pregnancy in women with arrhythmogenic right ventricular cardiomyopathy/dysplasia. Eur J Obstet Gynecol Reprod Biol 2006; 127(2): 186-9. Doi: 10.1016/j.ejogrb.2005.10.011.
Gandjbakhch E., Varlet E., Duthoit G., Fressart V., Charron P., Himbert C., Maupain C., Bordet C., Hidden-Lucet F., Nizard J. Pregnancy and newborn outcomes in arrhythmogenic right ventricular cardiomyopathy/dysplasia. Int J Cardiol 2018; 258: 172-178. Doi: 10.1016/j.ijcard.2017.11.067.
Regitz-Zagrosek V., Roos-Hesselink JW., Bauersachs J., Blomström-Lundqvist C., Cífková R., De Bonis M., Iung B., Johnson MR., Kintscher U., Kranke P., et al. 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J 2018; 39(34): 3165-3241. Doi: 10.1093/eurheartj/ehy340.
Wang YC., Chen CH., Su HY., Yu MH. The impact of maternal cardioversion on fetal haemodynamics. Eur J Obstet Gynecol Reprod Biol 2006; 126(2): 268-9. Doi: 10.1016/j.ejogrb.2005.11.021.
И. Стрюк, Ю.А. Бунин, В.М. Гурьева, О.Б. Иртюга, Л.С. Коков, О.Е. Коломацкая, О.М. Моисеева, С.Р. Мравян, А.И. Чесникова, В.С. Чулков, и др. Диагностика и лечение сердечно-сосудистых заболеваний при беременности 2018. Национальные рекомендации. Российский кардиологический журнал 2018; (3): 91-134. Doi: 10.15829/1560-4071-2018-3-91-134
Cleary-Goldman J, Salva CR, Infeld JI, Robinson JN. Verapamil-sensitive idiopathic left ventricular tachycardia in pregnancy. J Matern Fetal Neonatal Med. 2003 Aug;14(2):132-5.
Abello M., Peinado R., Merino JL., Gnoatto M., Mateos M., Silvestre J., Dominguez JL. Cardioverter defibrillator implantation in a pregnant woman guided with transesophageal echocardiography. Pacing Clin Electrophysiol 2003; 26(9): 1913-4. Doi: 10.1046/j.1460-9592.2003.00293.x.
Tuzcu V., Kilinc OU. Implantable cardioverter defibrillator implantation without using fluoroscopy in a pregnant patient. Pacing Clin Electrophysiol 2012; 35(9): e265-6. Doi: 10.1111/j.1540-8159.2011.03221.x.
Driver K., Chisholm CA, Darby AE., et al. Catheter ablation of arrhythmia during pregnancy. Journal of Cardiovascular Electrophysiology 2015; 26(6): 698-702. Doi: 10.1111/jce.1267
Silversides CK., Harris L., Haberer K., Sermer M., et al. Recurrence rates of arrhythmias during pregnancy in women with previous tachyarrhythmia and impact on fetal and neonatal outcomes. The American Journal of Cardiology 2006; 97(8): 1206-1212. Doi: 10.1016/j.amjcard.2005.11.041.
Barnes E.J., Eben F., Patterson D. Direct current cardioversion during pregnancy should be performed with facilities available for fetal monitoring and emergency caesarean section. BJOG 2002; 109(12): 1406-1407. Doi: 10.1046/j.1471-0528.2002.02113.x.
Miyoshi T., Kamiya CA., Katsuragi S., Ueda H., et al. Safety and efficacy of implantable cardioverter-defibrillator during pregnancy and after delivery. Circulaton 2013; 77(5): 1166-1170. Doi: 10.1253/circj.cj-12-1275.
Hartz J., Clark BC., Ito S., Sherwin ED., Berul CI. Transvenous nonfluoroscopic pace maker implantation during pregnancy guided by 3-dimensional electroanatomic mapping. HeartRhythm Case Reports 2017; 3(10): 490-492. Doi: 10.1016/j.hrcr.2017.07.020.
Sliwa K., Mebazaa A., Hilfiker-Kleiner D., Petrie MC,. et al. Clinical characteristics of patients from the worldwide registry on peripartum cardiomyopathy (PPCM): EURObservational Research Programme in conjunction with the Heart Failure Association of the European Society of Cardiology Study Group on PPCM. European Journal of Heart Failure 2017; 19(9): 1131-1141. Doi: 10.1002/ejhf.780.
Jeejeebhoy FM., Zelop CM., Lipman S., et al. Cardiac arrest in pregnancy: a scientific statement from the American heart association. Circulation 2015; 132(18): 1747-1773. Doi: 10.1161/CIR.0000000000000300.
European Society of Gynecology (ESG), Association for European Paediatric Cardiology (AEPC), German Society for Gender Medicine (DGesGM), Regitz-Zagrosek V., Blomstrom Lundqvist C., Borghi C., et al. ESC Guidelines on the management of cardiovascular diseases during pregnancy: the task force on the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC). European Heart Journal 2011; 32(24): 3147-3197. Doi: 10.1093/eurheartj/ehr218.
Benito B., Berruezo A. Brugada syndrome and pregnancy: delving into the role of sex hormones in ion channelopathies. Revista Española de Cardiología (Engl Ed) 2014; 67(3): 165-167. Doi: 10.1016/j.rec.2013.09.021.
Wang Z., Chen YW., Jiang YH., et al. Electrophysiological characteristics and therapeutic efficacy of radiofrequency ablation of focal atrial tachycardia originating from the right atrial appendage during pregnancy. Zhonghua Xin Xue Guan Bing Za Zhi 2020; 48(10): 859-865. Doi: 10.3760/cma.j.cn112148-20191104-00683.
Ware JS, Li J., Mazaika E., Yasso CM., et al. Shared genetic predisposition in peripartum and dilated cardiomyopathies. The New England Journal of Medicine 2016; 374(3): 233-241. Doi: 10.1056/NEJMoa1505517.
Bauersachs J., König T., van der Meer P., Petrie MC., et al. Pathophysiology, diagnosis and management of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Study Group on peripartum cardiomyopathy. European Journal of Heart Failure 2019; 21(7): 827-843. Doi: 10.1002/ejhf.1493.
Sliwa K., Blauwet L., Tibazarwa K., Libhaber E., et al. Evaluation of bromocriptine in the treatment of acute severe peripartum cardiomyopathy: a proof-of-concept pilot study. Circulation 2010; 121(13): 1465-1473. Doi: 10.1161/CIRCULATIONAHA.109.901496.
Hilfiker-Kleiner D., Haghikia A., Berliner D., Vogel-Claussen J., et al. Bromocriptine for the treatment of peripartum cardiomyopathy: a multicentre randomized study. European Heart Journal 2017; 38(35): 2671-2679. Doi: 10.1093/eurheartj/ehx355
Fröhlich GM., Holzmeister J., Hübler M., et al. Prophylactic implantable cardioverter defibrillator treatment in patients with end-stage heart failure awaiting heart transplantation. Heart 2013; 99(16): 1158-1165. Doi: 10.1136/heartjnl-2013-304185.
Joglar JA., Wan EY., Chung MK., Gutierrez A., Slaughter MS., Bateson BP., Loguidice M., Drazner M., Kistler PM., Saour B., et al. Management of Arrhythmias After Heart Transplant: Current State and Considerations for Future Research. Circ Arrhythm Electrophysiol 2021; 14(3): e007954. Doi: 10.1161/CIRCEP.120.007954.
Garcia R., Combes N., Defaye P., Narayanan K., Guedon-Moreau L., Boveda S., Blangy H., Bouet J., Briand F., Chevalier P., et al. Wearable cardioverter-defibrillator in patients with a transient risk of sudden cardiac death: the WEARIT-France cohort study. Europace 2021; 23(1): 73-81. Doi: 10.1093/europace/euaa268.
Costanzo MR., Dipchand A., Starling R., Anderson A., Chan M., Desai S., Fedson S., Fisher P., Gonzales-Stawinski G., Martinelli L., et al. The International Society of Heart and Lung Transplantation Guidelines for the care of heart transplant recipients. J Heart Lung Transplant 2010; 29(8): 914-56. Doi: 10.1016/j.healun.2010.05.034.
Alba AC., Foroutan F., Ng Fat Hing NKV., Fan CS., Manlhiot C., Ross HJ. Incidence and predictors of sudden cardiac death after heart transplantation: A systematic review and meta-analysis. Clin Transplant 2018; 32(3): e13206. Doi: 10.1111/ctr.13206.
Vakil K., Taimeh Z., Sharma A., Abidi KS., Colvin M., Luepker R., Levy WC., Adabag S. Incidence, predictors, and temporal trends of sudden cardiac death after heart transplantation. Heart Rhythm 2014; 11(10): 1684-90. Doi: 10.1016/j.hrthm.2014.07.016.
Pelliccia A., Sharma S., Gati S., Bäck M., Börjesson M., Caselli S., Collet JP., Corrado D., Drezner JA., Halle M., et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J. 2021 Jan 1;42(1):17-96. doi: 10.1093/eurheartj/ehaa605. Erratum in: Eur Heart J 2021; 42(5): 548-549. Doi: 10.1093/eurheartj/ehaa835.
Corrado D., Zorzi A. Sudden death in athletes. Int J Cardiol 2017; 237: 67-70. Doi: 10.1016/j.ijcard.2017.03.034.
Holst AG., Winkel BG., Theilade J., Kristensen IB., Thomsen JL., Ottesen GL., Svendsen JH., Haunsø S., Prescott E., Tfelt-Hansen J. Incidence and etiology of sports-related sudden cardiac death in Denmark--implications for preparticipation screening. Heart Rhythm 2010; 7(10): 1365-71. Doi: 10.1016/j.hrthm.2010.05.021.
Corrado D., Schmied C., Basso C., Borjesson M., Schiavon M., Pelliccia A., Vanhees L., Thiene G. Risk of sports: do we need a pre-participation screening for competitive and leisure athletes? Eur Heart J 2011; 32(8): 934-44. Doi: 10.1093/eurheartj/ehq482.
Drezner JA., Peterson DF., Siebert DM., Thomas LC., Lopez-Anderson M., Suchsland MZ., Harmon KG., Kucera KL. Survival After Exercise-Related Sudden Cardiac Arrest in Young Athletes: Can We Do Better? Sports Health 2019;11(1): 91-98. Doi: 10.1177/1941738118799084.
Drezner JA., Rogers KJ., Horneff JG. Automated external defibrillator use at NCAA Division II and III universities. Br J Sports Med 2011; 45(15): 1174-8. Doi: 10.1136/bjsm.2009.070052.
Malhotra A., Dhutia H., Finocchiaro G., Gati S., Beasley I., Clift P., Cowie C., Kenny A., Mayet J., Oxborough D., et al. Outcomes of Cardiac Screening in Adolescent Soccer Players. N Engl J Med 2018; 379(6): 524-534. Doi: 10.1056/NEJMoa1714719.
Maestrini V, Torlasco C, Hughes R, Moon JC. Cardiovascular Magnetic Resonance and Sport Cardiology: a Growing Role in Clinical Dilemmas. J Cardiovasc Transl Res. 2020 Jun;13(3):296-305.
Kragholm K., Wissenberg M., Mortensen RN., Hansen SM., Malta Hansen C., Thorsteinsson K., Rajan S., Lippert F., Folke F., Gislason G., et al. Bystander Efforts and 1-Year Outcomes in Out-of-Hospital Cardiac Arrest. N Engl J Med 2017; 376(18): 1737-1747. Doi: 10.1056/NEJMoa1601891.
Pediatric and Congenital Electrophysiology Society (PACES); Heart Rhythm Society (HRS); American College of Cardiology Foundation (ACCF); American Heart Association (AHA); American Academy of Pediatrics (AAP); Canadian Heart Rhythm Society (CHRS); Cohen MI., Triedman JK., Cannon BC., Davis AM., et al. PACES/HRS expert consensus statement on the management of the asymptomatic young patient with a Wolff-Parkinson-White (WPW, ventricular preexcitation) electrocardiographic pattern: developed in partnership between the Pediatric and Congenital Electrophysiology Society (PACES) and the Heart Rhythm Society (HRS). Endorsed by the governing bodies of PACES, HRS, the American College of Cardiology Foundation (ACCF), the American Heart Association (AHA), the American Academy of Pediatrics (AAP), and the Canadian Heart Rhythm Society (CHRS). Heart Rhyth. 2012; 9(6): 1006-24. Doi: 10.1016/j.hrthm.2012.03.050.
Gill JS., Ward DE., Camm AJ. Comparison of verapamil and diltiazem in the suppression of idiopathic ventricular tachycardia. Pacing Clin Electrophysiol 1992; 15(11 Pt 2): 2122-6. Doi: 10.1111/j.1540-8159.1992.tb03033.x.
Elming MB., Nielsen JC., Haarbo J., Videbæk L., Korup E., Signorovitch J., Olesen LL., Hildebrandt P., Steffensen FH., Bruun NE., et al. Age and Outcomes of Primary Prevention Implantable Cardioverter-Defibrillators in Patients With Nonischemic Systolic Heart Failure. Circulation 2017; 136(19): 1772-1780. Doi: 10.1161/CIRCULATIONAHA.117.028829.
Wang S., Zhu W., Hamilton RM., Kirsh JA., Stephenson EA., Gross GJ. Diagnosis-specific characteristics of ventricular tachycardia in children with structurally normal hearts. Heart Rhythm 2010; 7(12): 1725-31. Doi: 10.1016/j.hrthm.2010.07.037.
М.А. Школьникова, В.В. Березницкая. Желудочковые аритмии. Клинические рекомендации по детской кардиологии и ревматологии 2011. 5: 133–159.
Blaufox AD., Felix GL., Saul JP. Pediatric Catheter Ablation Registry. Radiofrequency catheter ablation in infants </=18 months old: when is it done and how do they fare?: short-term data from the pediatric ablation registry. Circulation 2001; 104(23): 2803-8. Doi: 10.1161/hc4801.100028.
Li G., Zhang L. The role of mexiletine in the management of long QT syndrome. J Electrocardiol 2018; 51(6): 1061-1065. Doi: 10.1016/j.jelectrocard.2018.08.035.
Yeh SJ., Kou HC., Lin FC., Hung JS., Wu D. Effects of oral diltiazem in paroxysmal supraventricular tachycardia. Am J Cardiol 1983; 52(3): 271-8. Doi: 10.1016/0002-9149(83)90121-2.
Buckley MM., Grant SM., Goa KL., McTavish D., Sorkin EM. Diltiazem. A reappraisal of its pharmacological properties and therapeutic use. Drugs 1990; 39(5): 757-806. Doi: 10.2165/00003495-199039050-00009.
Lapage MJ., Bradley DJ., Dick M. 2nd. Verapamil in infants: an exaggerated fear? Pediatr Cardiol 2013; 34(7): 1532-4. Doi: 10.1007/s00246-013-0739-8.
Kirk CR., Gibbs JL., Thomas R., Radley-Smith R., Qureshi SA. Cardiovascular collapse after verapamil in supraventricular tachycardia. Arch Dis Child 1987; 62(12): 1265-6. Doi: 10.1136/adc.62.12.1265.
Surman TL., Stuklis RG., Chan JC. Thoracoscopic Sympathectomy for Long QT Syndrome. Literature Review and Case Study. Heart Lung Circ 2019; 28(3): 486-494. Doi: 10.1016/j.hlc.2018.02.005.
А. Ш. Ревишвили. Клинические рекомендации по проведению электрофизиологических исследований, катетерной абляции и применению имплантируемых антиаритмических устройств. Всероссийское научное общество специалистов по клинической электрофизиологии, аритмологии и кардиостимуляции 2013; 595: 16.
Wenger NK., Froelicher ES., Smith LK., Ades PA., Berra K., Blumenthal JA., Certo CM., Dattilo AM., Davis D., DeBusk RF., et al. Cardiac rehabilitation as secondary prevention. Agency for Health Care Policy and Research and National Heart, Lung, and Blood Institute. Clin Pract Guidel Quick Ref Guide Clin 1995; (17): 1-23.
Thomas R. J., et al. AACVPR/ACC/AHA 2007 performance measures on cardiac rehabilitation for referral to and delivery of cardiac rehabilitation/secondary prevention services endorsed by the American College of Chest Physicians, American College of Sports Medicine, American Physical Therapy Association, Canadian Association of Cardiac Rehabilitation, European Association for Cardiovascular Prevention and Rehabilitation, Inter-American Heart Foundation, National Association of Clinical Nurse Specialists, Preventive Cardiovascular Nurses Association, and the Society of Thoracic Surgeons. JACC 2007; 50(14): 1400 –33.
Клинические рекомендации «Желудочковые аритмии» МЗ РФ, ФГБУ «ННПЦССХ им. А.Н. Бакулева» МЗ РФ Центр хирургической и интервенционной аритмологии. – Москва, 2017. – 38 с.
Morady F., Kadish AH., DiCarlo L., Kou WH., et al. Long term results of catheter ablation of idiopathic right ventricular tachycardia. Circulation 1990; 82(6): 2093-2099. Doi: 10.1161/01.cir.82.6.2093.
Tada H., Hiratsuji T., Naito S., Kurosaki K., et al. Prevalence and characteristics of idiopathic outflow tract tachycardia with QRS alteration following catheter ablation requiring additional radiofrequency ablation at a different point in the outflow tract. Pacing Clinical Electrophysiology 2004; 27(9): 1240-1249. Doi: 10.1111/j.1540-8159.2004.00615.x.
Klein LS., Shih HT., Hackett FK., Zipes DP., et al. Radiofrequency catheter ablation of ventricular tachycardia in patients without structural heart disease. Circulation 1992; 85(5): 1666-1674. Doi: 10.1161/01.cir.85.5.1666.
Della Bella P., Baratto F., Tsiachris D., et al. Management of ventricular tachycardia in the setting of a dedicated unit for the treatment of complex ventricular arrhythmias: long-term outcome after ablation. Circulation 2013; 127(13): 1359-1368. Doi: 10.1161/CIRCULATIONAHA.112.000872.
Koruth JS., Aryana A., Dukkipati SR., et al. Unusual complications of percutaneous epicardial access and epicardial mapping and ablation of cardiac arrhythmias. Circulation: Arrhythmia and Electrophysiology 2011; 4(6): 882-888. Doi: 10.1161/CIRCEP.111.965731.
Roberts-Thomson KC., Steven D., Seller J., et al. Coronary artery injury due to catheter ablation in adults: presentations and outcomes. Circulation 2009; 120(15): 1465-1473. Doi: 10.1161/CIRCULATIONAHA.109.870790.
Makimoto H., Zhang Q., Tilz RR. et al. Aborted sudden cardiac death due to radiofrequency ablation within the coronary sinus and subsequent total occlusion of the circumflex artery. Journal of Cardiovascular Electrophysiology 2013; 24(8): 929-932. Doi: 10.1111/jce.12083.
Schwartz PJ., Stramba–Badiate M., Crotti L., et al. Prevalence of the congenital long QT syndrome. Circulation 2009; 120(18): 1761-1767. Doi: 10.1161/CIRCULATIONAHA.109.863209.
Corrado D., Petticcia A., Bjornstad HH., et al. Cardiovascular pre–participation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol. Consensus Statement of the Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. European Heart Journal 2005; 26(5): 516-524. Doi: 10.1093/eurheartj/ehi108.
Maron BJ., Thompson PD., Ackerman MJ., et al. Recommendations and considerations related to preparticipation screening for cardiovascutar abnormalities in competitive athletes: 2007 update: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: endorsed by the American College of Cardiology Foundation. Circulation 2007; 115(12): 1643-1455. Doi: 10.1161/CIRCULATIONAHA.107.181423.
Ljungqvist A., Jenoure P., Engebretsen L., et al. The International Olympic Committee (IOC) consensus statement on periodic health evaluation of elite athletes, March 2009. British Journal of Sports Medicine 2009; 43(9): 631-643. Doi: 10.1136/bjsm.2009.064394.
Steinvil A., Chundadze T., Zeltser D., et al. Mandatory etectrocardiographic screening of athletes to reduce their risk for sudden death: proven fact or wishful thinking? JACC 2011; 57(11): 1291-1296. Doi: 10.1016/j.jacc.2010.10.037. .
Kaltman JR., Thompson PD., Lantos J., Berul CI., Botkin J., Cohen JT., Cook NR., Corrado D., Drezner J., Frick KD., et al. Screening for sudden cardiac death in the young: report from a national heart, lung, and blood institute working group. Circulation 2011; 123(17): 1911-8. Doi: 10.1161/CIRCULATIONAHA.110.017228.
Narain R., Mayers J., Dhutia H., Malhotra A., Merghani A., Millar L., Sheikh N., Paradakis M., Sharma S. Preventing sudden cardiac death in the young: results from a population-based screening program in the UK. European Journal of Preventive Cardiology 2014; 21: S1–S6. DOI:10.1016/j.ihj.2014.10.194 УДД 4 УУР С (взрослые, дети)
Charron P., Arad M., Arbustini E., Basso C., Bilinska Z., Elliott P., Helio T., Keren A., McKenna WJ., Monserrat L., et al. Genetic counselling and testing in cardiomyopathies: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J 2010; 31(22): 2715-26. Doi: 10.1093/eurheartj/ehq271.
Ormondroyd E., Oates S., Parker M., Blair E., Watkins H. Pre-symptomatic genetic testing for inherited cardiac conditions: a qualitative exploration of psychosocial and ethical implications. Eur J Hum Genet 2014; 22(1): 88-93. Doi: 10.1038/ejhg.2013.81.
Ingles J., Yeates L., Hunt L., McGaughran J., Scuffham PA., Atherton J., Semsarian C. Health status of cardiac genetic disease patients and their at-risk relatives. Int J Cardiol 2013; 165(3): 448-53. Doi: 10.1016/j.ijcard.2011.08.083.
Battista RN., Blancquaert I., Laberge AM., van Schendel N., Leduc N. Genetics in health care: an overview of current and emerging models. Public Health Genomics 2012; 15(1): 34-45. Doi: 10.1159/000328846.
Чазов Е.И., Агеев Ф.Т., Акчурин Р.С., Буза В.В., Власова Э.Е., Голицин С.П., Ефремова Ю.Е., Карпов Ю.А., Кухарчук В.В., Малкина Т.А., Мартынюк Т.В. и др. Рекомендации по диспансерному наблюдению больных с сердечно-сосудистыми заболеваниями. – Москва, 2014. – 28 с.
Nolan JP., Soar J., Zideman DA., Biarent D., Bossaert LL., Deakin C., Koster RW., Wyllie J., Böttiger B.; ERC Guidelines Writing Group. European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summary. Resuscitation 2010; 81(10): 1219-76. Doi: 10.1016/j.resuscitation.2010.08.021.
Monsieurs KG., Nolan JP., Bossaert LL., Greif R., Maconochie IK., Nikolaou NI., Perkins GD., Soar J., Truhlář A., Wyllie J., et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 1. Executive summary. Resuscitation 2015; 95: 1-80. Doi: 10.1016/j.resuscitation.2015.07.038.
Chiu DT., Shapiro NI., Sun BC., Mottley JL., Grossman SA. Are echocardiography, telemetry, ambulatory electrocardiography monitoring, and cardiac enzymes in emergency department patients presenting with syncope useful tests? A preliminary investigation. J Emerg Med 2014; 47(1): 113-8. Doi: 10.1016/j.jemermed.2014.01.018.
Приказ Министерства здравоохранения Российской Федерации от 10.08.2017 № 514н «О порядке прохождения несовершеннолетними медицинских осмотров, в том числе при поступлении в образовательные учреждения и в период обучения в них»: Приложение №1.
Школьникова М.А., Харлап М.С., Ильдарова Р.А. Генетически детерминированные нарушения ритма сердца. Российский кардиологический журнал 2011; 1 (87): 8–25.
Adler A., Halkin A., Viskin S. Wearable cardioverter-defibrillators. Circulation 2013; 127(7): 854-60. Doi: 10.1161/CIRCULATIONAHA.112.146530.
Hallstrom AP., Ornato JP., Weisfeldt M., Travers A., Christenson J., McBurnie MA., Zalenski R., Becker LB., Schron EB., Proschan M.; Public Access Defibrillation Trial Investigators. Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med 2004; 351(7): 637-46. Doi: 10.1056/NEJMoa040566.
Quill TE., Brody H. Physician recommendations and patient autonomy: finding a balance between physician power and patient choice. Ann Intern Med 1996; 125(9): 763-9. Doi: 10.7326/0003-4819-125-9-199611010-00010.
Stewart GC., Weintraub JR., Pratibhu PP., Semigran MJ., Camuso JM., Brooks K., Tsang SW., Anello MS., Nguyen VT., Lewis EF., et al. Patient expectations from implantable defibrillators to prevent death in heart failure. J Card Fail 2010; 16(2): 106-13. Doi: 10.1016/j.cardfail.2009.09.003.
Ottenberg AL., Mueller PS., Topazian RJ., Kaufman S., Swetz KM. "It's not broke, so let's not try to fix it": why patients decline a cardiovascular implantable electronic device. Pacing Clin Electrophysiol 2014; 37(10): 1306-14. Doi: 10.1111/pace.12433.
Sherazi S., Zareba W., Daubert JP., McNitt S., Shah AH., Aktas MK., Block RC. Physicians' knowledge and attitudes regarding implantable cardioverter-defibrillators. Cardiol J 2010; 17(3): 267-73.
Charles C., Gafni A., Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med 1997; 44(5): 681-92. Doi: 10.1016/s0277-9536(96)00221-3.
Lewis KB., Stacey D., Matlock DD. Making decisions about implantable cardioverter-defibrillators from implantation to end of life: an integrative review of patients' perspectives. Patient 2014; 7(3): 243-60. Doi: 10.1007/s40271-014-0055-2.
The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): a randomised trial. Lancet 1999; 353(9146): 9-13.
Packer M., Bristow MR., Cohn JN., Colucci WS., Fowler MB., Gilbert EM., Shusterman NH. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. U.S. Carvedilol Heart Failure Study Group. N Engl J Med 1996; 334(21): 1349-55. Doi: 10.1056/NEJM199605233342101.
Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet. 1999; 353(9169): 2001-7.
A randomized trial of propranolol in patients with acute myocardial infarction. I. Mortality results. JAMA 1982; 247(12): 1707-14. Doi: 10.1001/jama.1982.03320370021023.
Hirsowitz G., Podrid PJ., Lampert S., Stein J., Lown B. The role of beta blocking agents as adjunct therapy to membrane stabilizing drugs in malignant ventricular arrhythmia. Am Heart J 1986; 111(5): 852-60. Doi: 10.1016/0002-8703(86)90633-2.
Peltenburg PJ., Kallas D., Bos JM., Lieve KVV., Franciosi S., Roston TM., et al. An international multicenter cohort study on β-blockers for the treatment of symptomatic children with catecholaminergic polymorphic ventricular tachycardia. Circulation 2022; 145(5): 333-344. Doi: 10.1161/CIRCULATIONAHA.121.056018.
Yager N., Wang K., Keshwani N., Torosoff M. Phenytoin as an effective treatment for polymorphic ventricular tachycardia due to QT prolongation in a patient with multiple drug intolerances. BMJ Case Rep 2015; 2015: bcr2015209521. Doi:10.1136/bcr-2015-209521.
Ito M., Maeda Y., Arita M., Ito S., Saikawa T., Omura I., et al. Effects of oral 784 diltiazem on ventricular premature contractions. J Electrocardiol 1986; 19(1): 59-66. Doi: 10.1016/s0022-0736(86)80008-5.
Garson AJr., Gillette PC., McVey P., Hesslein PS., Porter CJ., Angell LK., Kaldis LC., Hittner HM. Amiodarone treatment of critical arrhythmias in children and young adults. J Am Coll Cardiol 1984; 4(4): 749-755. Doi: 10.1016/s0735-1097(84)80402-7.
Yu Y., Liting T., Xiaoqin W. et al. Clinical and genetic profiles of chinese pediatric patients with catecholaminergic polymorphic ventricular tachycardia. Orphanet J Rare Dis 2023; 18(1): 380. Doi: 10.1186/s13023-023-02991-0.
Ильдарова Р.А., Щербакова Н.В., Березницкая В.В., Школьникова М.А. Сердечные и внесердечные проявления синдрома Джервелла-Ланге-Нильсена. Вестник аритмологии. 2021; 28(3): 37-44. https://doi.org/10.35336/VA-2021-3-37-44. УДД 4 УУР С (дети)
Wang Y., Yang Y., Xu N., Xiao Y., Zuo C., Chen Z. Clinical characteristics and follow-up of complex arrhythmias associated with RYR2 gene mutations in children. Front Genet 2024; 15: 1405437. Doi: 10.3389/fgene.2024.1405437.
Schupp T, Behnes M, Abumayyaleh M, Weidner K, Rusnak J, Mashayekhi K, Bertsch T, Akin I. Carvedilol versus Metoprolol in Patients with Ventricular Tachyarrhythmias. J Cardiovasc Dev Dis. 2022 Aug 16;9(8):274.
Joglar JA, Kapa S, Saarel EV, Dubin AM, Gorenek B, Hameed AB, Lara de Melo S, Leal MA, Mondésert B, Pacheco LD, Robinson MR, Sarkozy A, Silversides CK, Spears D, Srinivas SK, Strasburger JF, Tedrow UB, Wright JM, Zelop CM, Zentner D. 2023 HRS expert consensus statement on the management of arrhythmias during pregnancy. Heart Rhythm. 2023 Oct;20(10):e175-e264.
Дроздов Д.В., Макаров Л.М., Баркан В.С., Газашвили Т.М., Ефимова В.П., Жук М.Ю., Иртюга О.Б., Калинин Л.А., Ковалёв И.А.,Комолятова В.Н., Пармон Е.В., Рогоза А.Н., Стручков П.В., Татаринова А.А., Терегулов Ю. Э., Трешкур Т.В., Шутов Д.В. Регистрация электрокардиограммы покоя в 12 общепринятых отведениях взрослым и детям 2023 Методические рекомендации. Российский кардиологический журнал. 2023;28(10):5631. doi:10.15829/1560-4071-2023-5631.
Мацкеплишвили С.Т., Саидова М.А., Мироненко М.Ю., Сафарова А.Ф., Павлюкова Е.Н., Бощенко А.А., Ярославская Е.И., Ахунова С.Ю., Скидан В.И., Иртюга О.Б., Козленок А.В., Федорова Д.Н. Выполнение стандартной трансторакальной эхокардиографии. Методические рекомендации 2024 Российский кардиологический журнал. 2025;30(2):6271. https://doi.org/10.15829/1560-4071-2025-6271.
Bratton S, Taylor MK, Cortez P, Schiattarella A, Fochesato C, Sisti G. Does atenolol use during pregnancy cause small for gestational age neonates? A meta-analysis. J Perinat Med. 2024 Aug 8;52(8):858-862. doi: 10.1515/jpm-2024-0114. PMID: 39115600.
Регистр лекарственных средств России РЛС Энциклопедия лекарств. – 16-й вып./Гл. ред. Г.Л. Вышковский. – М.: «РЛС - 2008», 2007. – 1456 с.
Приказ Минздрава России от 15.11.2012 № 918н"Об утверждении порядка оказания медицинской помощи больным с сердечно-сосудистыми заболеваниями"(Зарегистрировано в Минюсте России 29.12.2012 № 26483).
Yeh SJ, Wen MS, Wang CC, Lin FC, Wu D. Adenosine-sensitive ventricular tachycardia from the anterobasal left ventricle. J Am Coll Cardiol. 1997 Nov 1;30(5):1339-45. doi: 10.1016/s0735-1097(97)00291-x. PMID: 9350937.
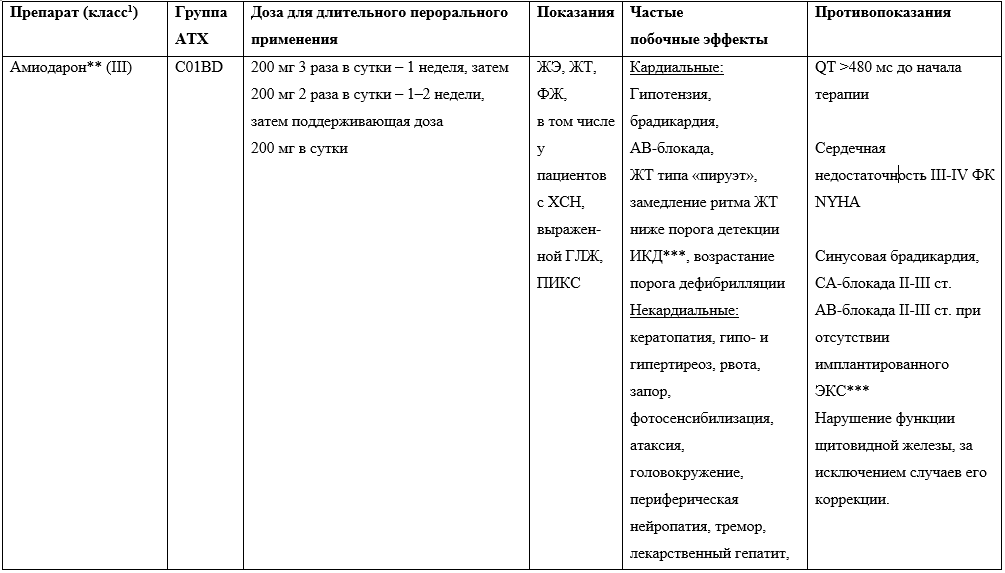
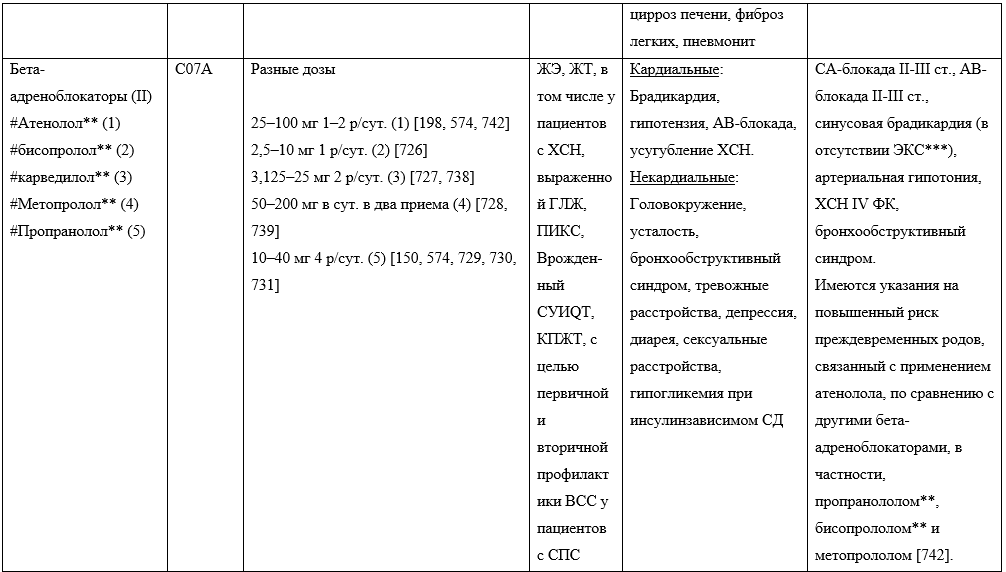
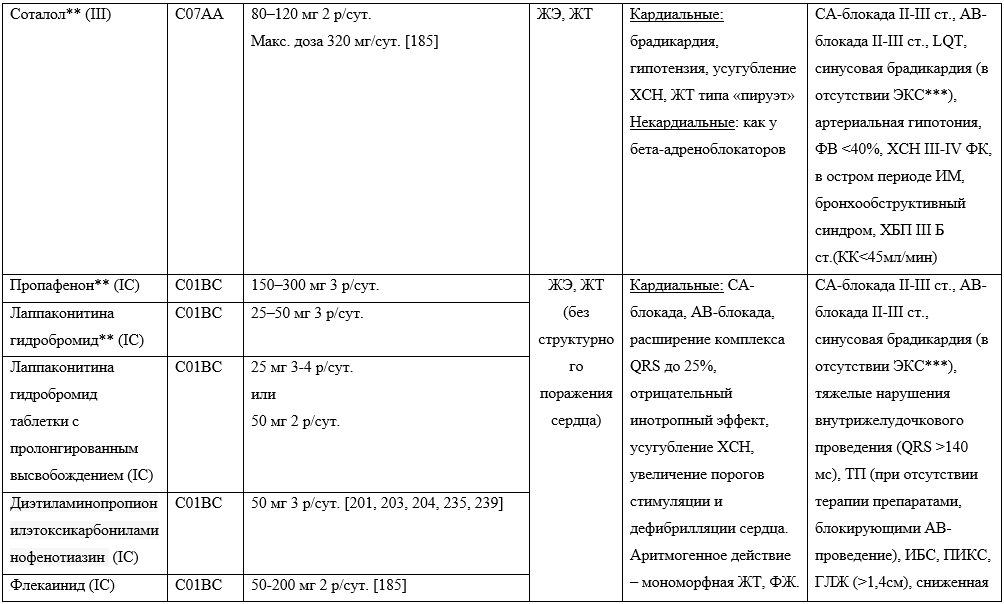
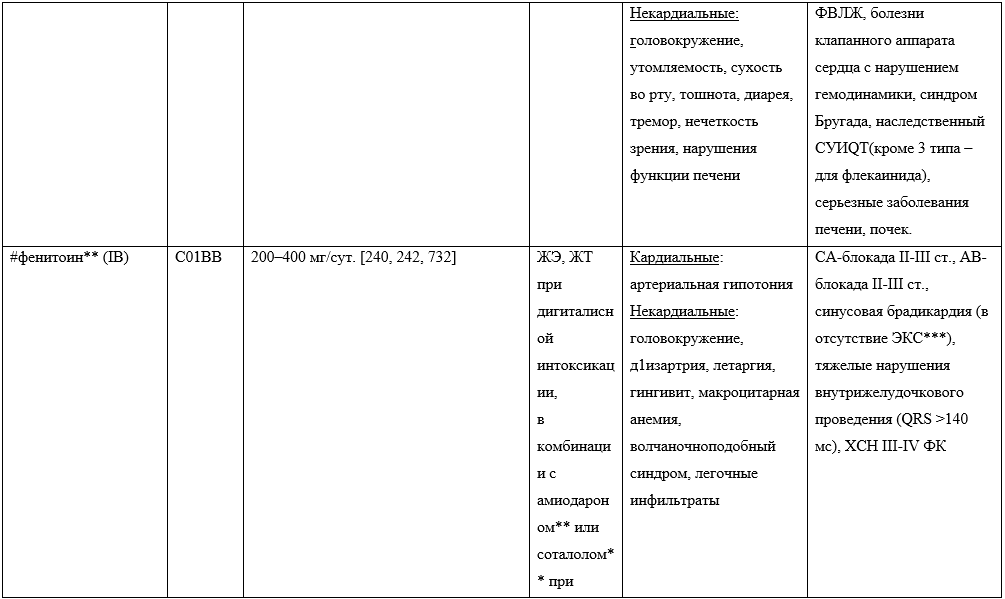
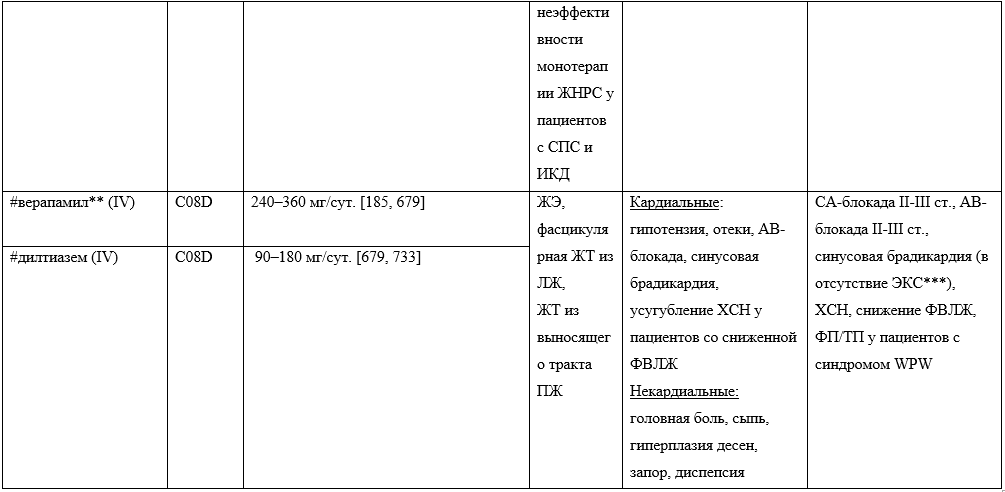 Примечания: 1согласно классификации E.Vaughan Williams в модификации D.Harrison.
Примечания: 1согласно классификации E.Vaughan Williams в модификации D.Harrison.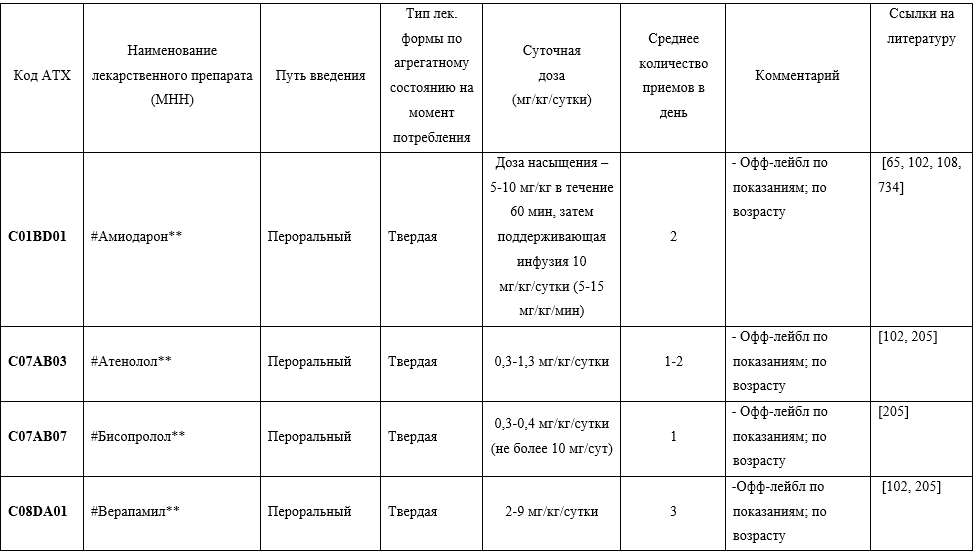
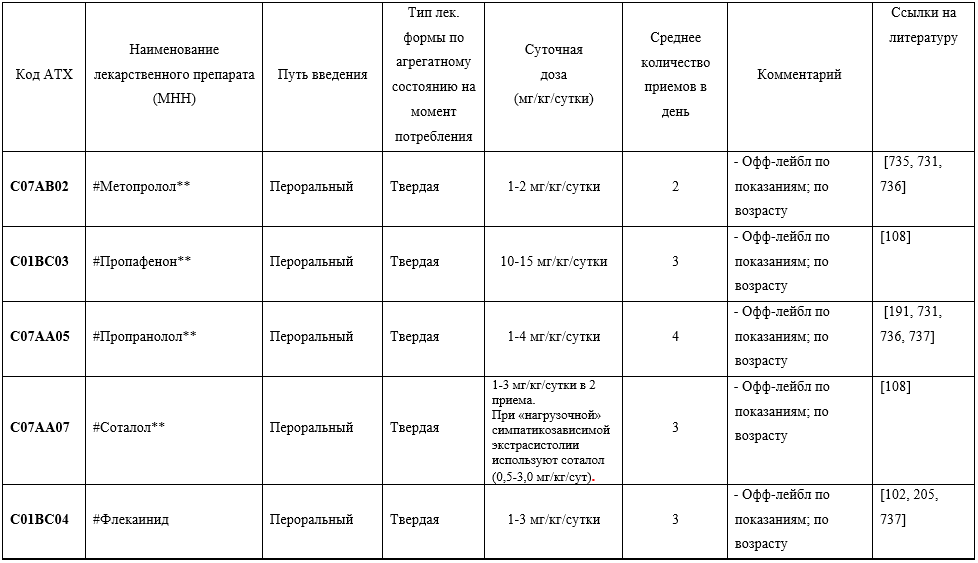
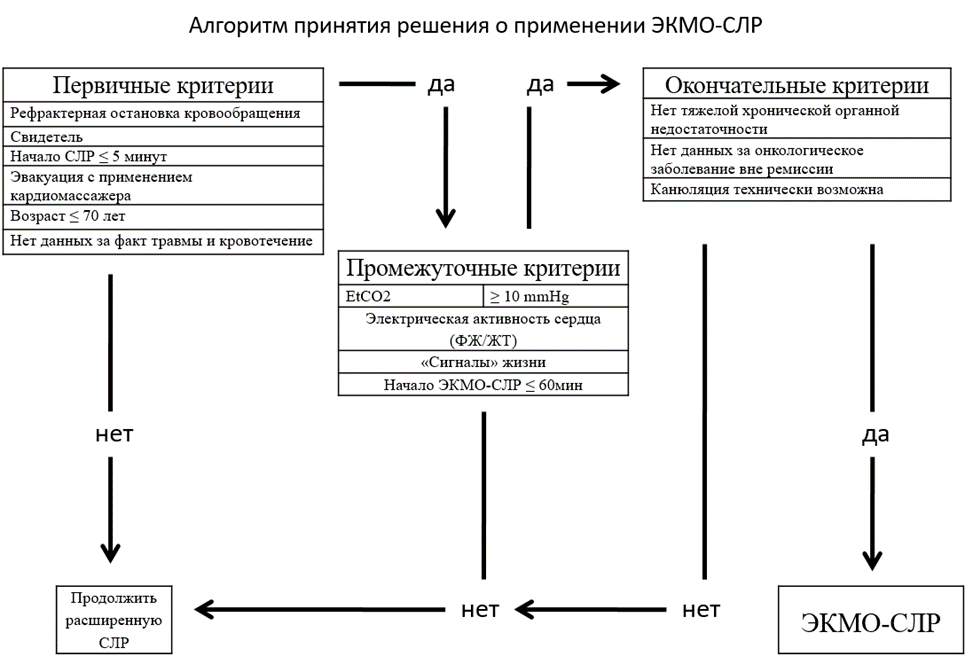 Критерии применения венозно-артериальной ЭКМО при проведении СЛР
Критерии применения венозно-артериальной ЭКМО при проведении СЛР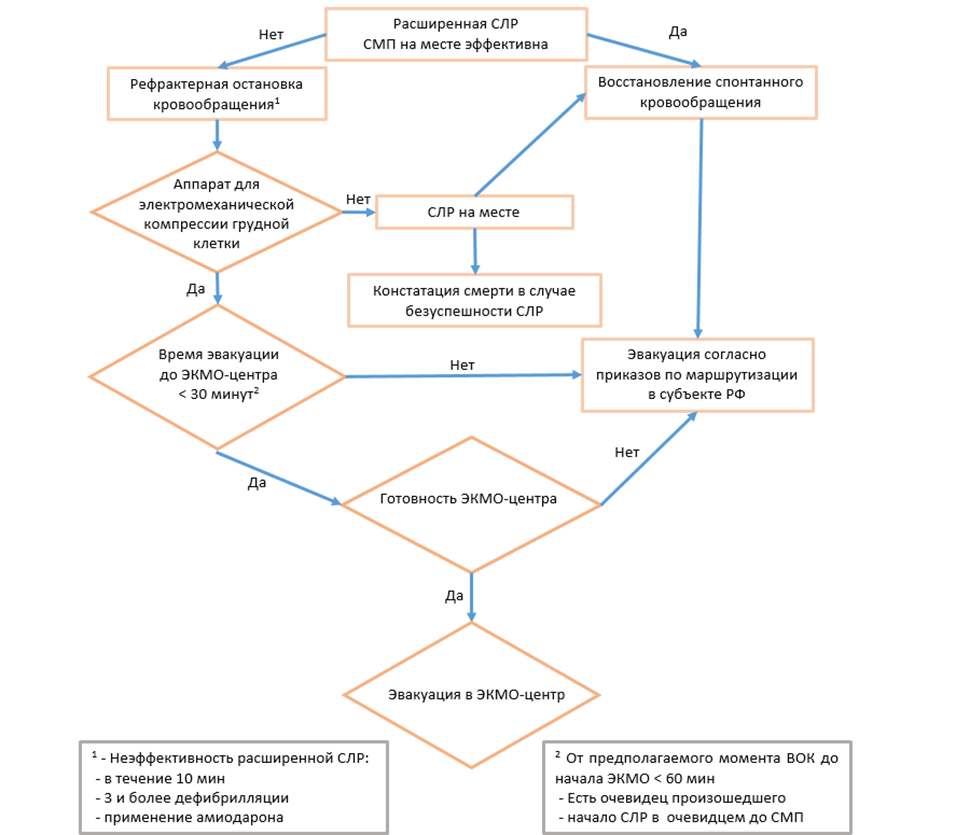 СРЛ – сердечно-легочная реанимация; ЭКМО – экстракорпоральная мембранная оксигенация; СМП – скорая медицинская помощь.
СРЛ – сердечно-легочная реанимация; ЭКМО – экстракорпоральная мембранная оксигенация; СМП – скорая медицинская помощь.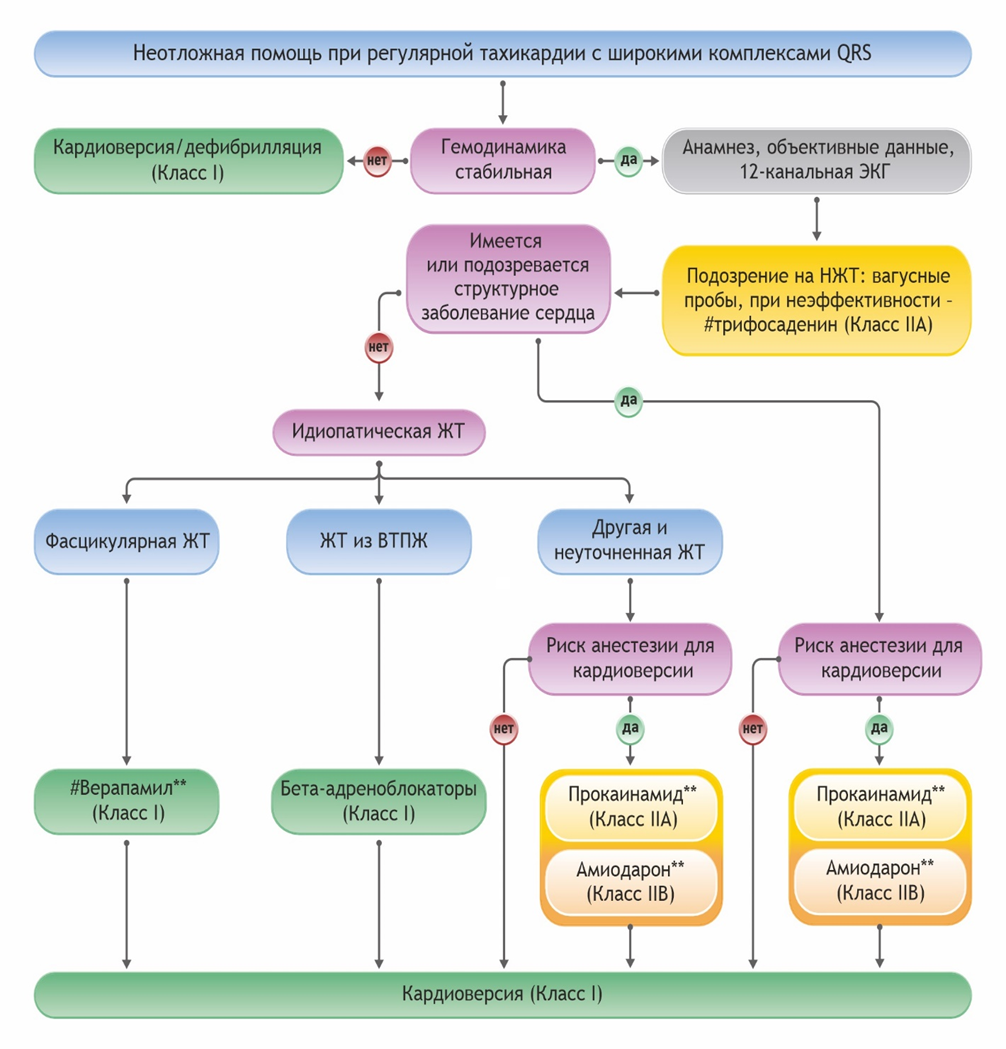 Примечание: НЖТ - наджелудочковая тахикардия, ЖТ – желудочковая тахикардия, ВТПЖ – выводной тракт правого желудочка (адаптировано из [8]).
Примечание: НЖТ - наджелудочковая тахикардия, ЖТ – желудочковая тахикардия, ВТПЖ – выводной тракт правого желудочка (адаптировано из [8]).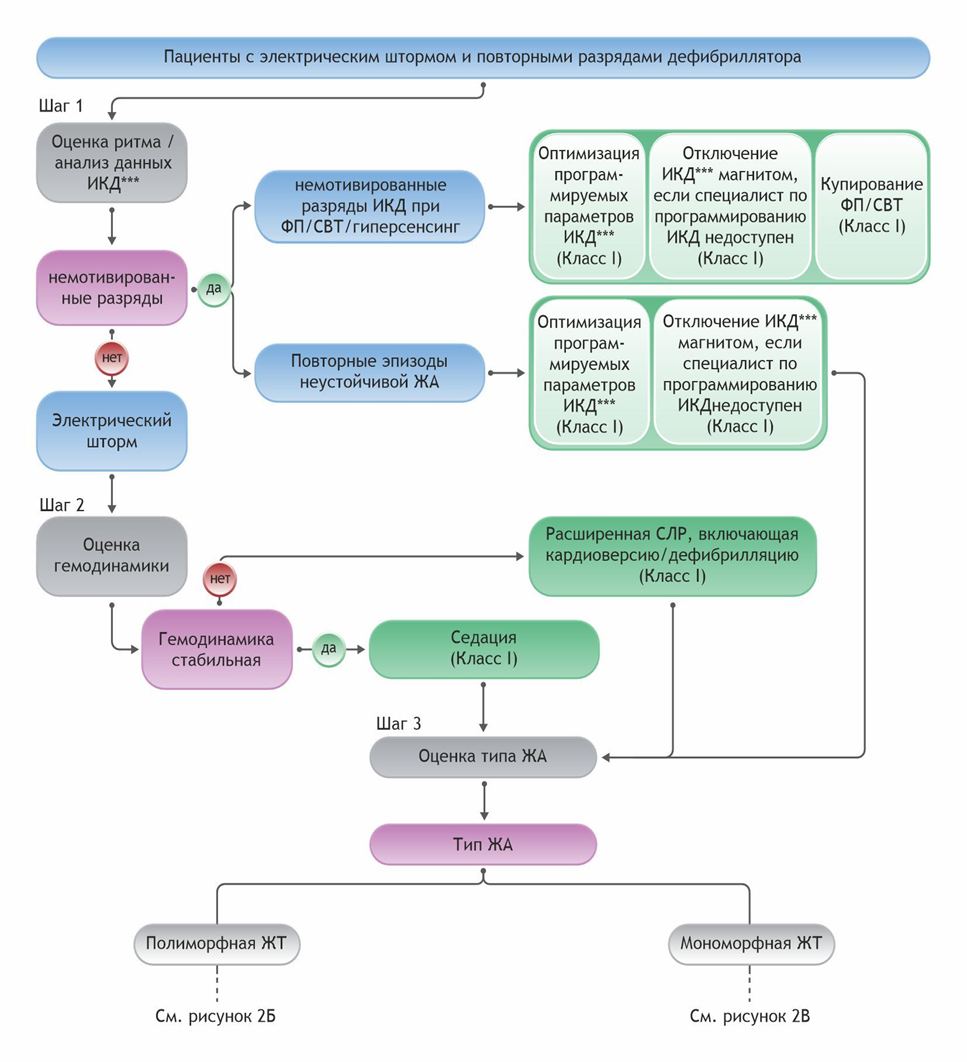
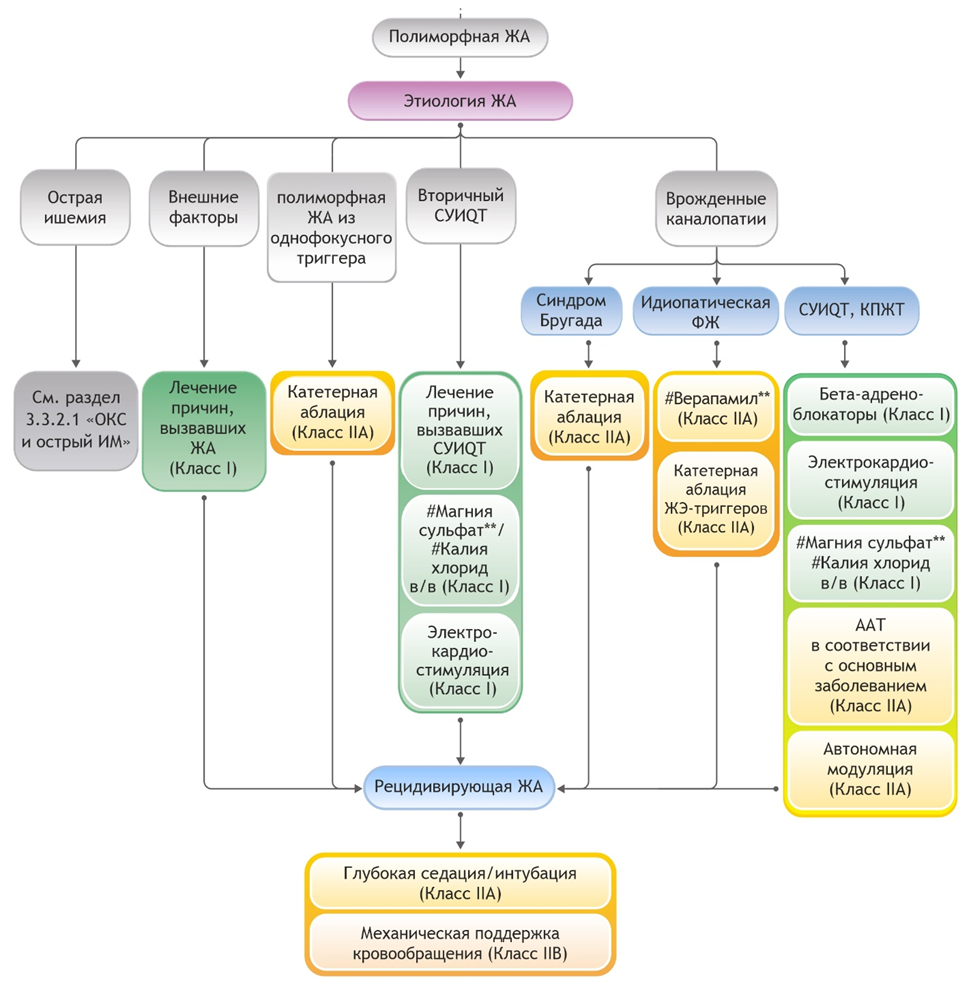 Примечание: ЖА – желудочковая аритмия, СУИQT – синдром удлиненного интервала QT, ФЖ – фибрилляция желудочков, КПЖТ – катехоламинергическая полиморфная желудочковая тахикардия, ОКС – острый коронарный синдром, ИМ – инфаркт миокарда, ЖЭ – желудочковая экстрасистолия, в/в – внутривенно, ААТ – антиаритмическая терапия (адаптировано из [8]).
Примечание: ЖА – желудочковая аритмия, СУИQT – синдром удлиненного интервала QT, ФЖ – фибрилляция желудочков, КПЖТ – катехоламинергическая полиморфная желудочковая тахикардия, ОКС – острый коронарный синдром, ИМ – инфаркт миокарда, ЖЭ – желудочковая экстрасистолия, в/в – внутривенно, ААТ – антиаритмическая терапия (адаптировано из [8]). 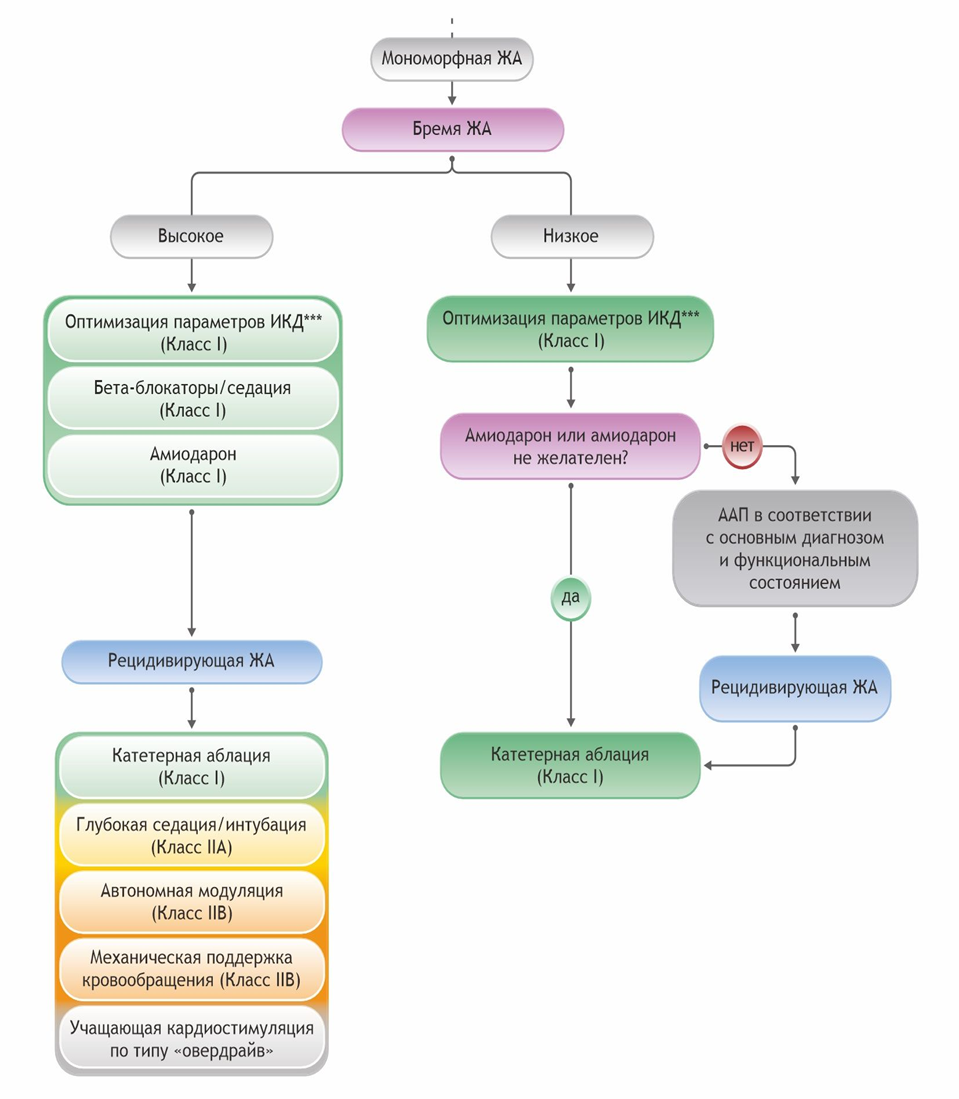 Примечание: ЖА – желудочковая аритмия, ИКД – кардиовертер-дефибриллятор имплантируемый***, ААП – антиаритмические препараты (адаптировано из [8]).
Примечание: ЖА – желудочковая аритмия, ИКД – кардиовертер-дефибриллятор имплантируемый***, ААП – антиаритмические препараты (адаптировано из [8]).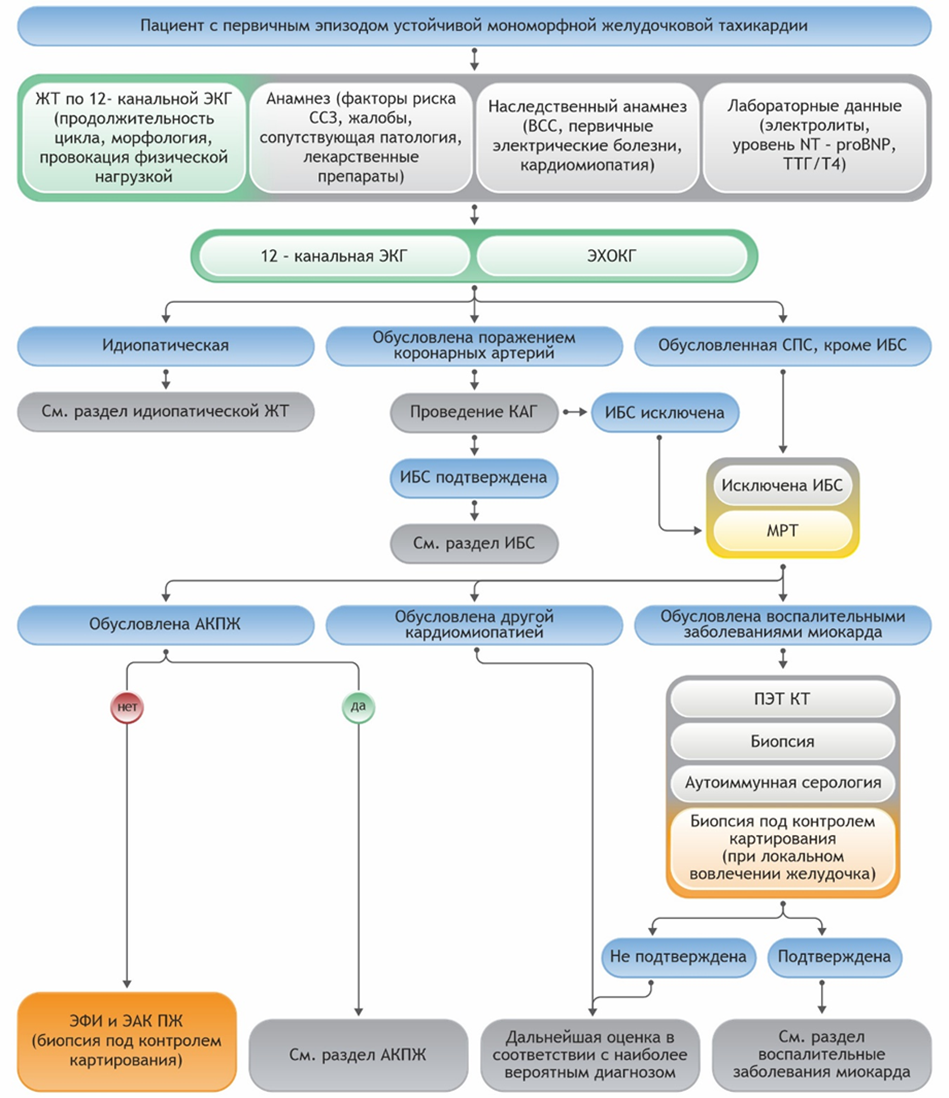 Примечание: ЖТ – желудочковая тахикардия, ССЗ – сердечно-сосудистые заболевания, ВСС – внезапная сердечная смерть, ТТГ – тиреотропный гормон, ЭХОКГ – эхокардиография, КАГ – коронароангиография, СПС – структурная патология сердца, ИБС – ишемическая болезнь сердца, МРТ – магнитно-резонансная томография сердца, АКПЖ – аритмогенная кардиомиопатия правого желудочка, ПЭТ КТ – позитронно-эмиссионная компьютерная томография, ЭФИ – электрофизиологическое исследование, ЭАК ПЖ – электроанатомическое картирование правого желудочка (адаптировано из [8]).
Примечание: ЖТ – желудочковая тахикардия, ССЗ – сердечно-сосудистые заболевания, ВСС – внезапная сердечная смерть, ТТГ – тиреотропный гормон, ЭХОКГ – эхокардиография, КАГ – коронароангиография, СПС – структурная патология сердца, ИБС – ишемическая болезнь сердца, МРТ – магнитно-резонансная томография сердца, АКПЖ – аритмогенная кардиомиопатия правого желудочка, ПЭТ КТ – позитронно-эмиссионная компьютерная томография, ЭФИ – электрофизиологическое исследование, ЭАК ПЖ – электроанатомическое картирование правого желудочка (адаптировано из [8]).