1. Детская гематология Под ред: А.Г. Румянцева, А.А. Масчана, Е.В. Жуковской. 2015. 656 p.
2. Pui C.-H. Childhood leukemias. 2012. 880 p.
3. Савченко В.Г., Паровичникова Е.Н. Острые лейкозы // Клиническая онкогематология: руководство для врачей. Под ред. Волковой М.А.. 2-е изд., перераб. и доп. 2007. P. 409–502.
4. Паровичникова Е.Н. et al. Клинический протокол ОМЛ-01.10 по лечению острых миелоидных лейкозов взрослых // Программное лечение заболеваний крови, под ред. Савченко В.Г. М.: Практика, 2012. P. 153–207.
5. Shallis R.M. et al. Epidemiology of acute myeloid leukemia: Recent progress and enduring challenges. // Blood Rev. 2019. Vol. 36. P. 70–87.
6. Swerdlow S.H. et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms // Blood. 2016.
7. Arber D.A. et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia // Blood. 2016.
8. Acute Myeloid Leukemia. National Comprehensive Cancer Network (NCCN) Guidelines. 2-2020. [Electronic resource]. URL: https://www.nccn.org/professionals/physician_gls/pdf/aml.pdf.
9. Kulsoom B. et al. Clinical presentation of acute myeloid leukaemia - A decade-long institutional follow-up. // J. Pak. Med. Assoc. 2017. Vol. 67, № 12. P. 1837–1842.
10. Godley L.A. Inherited predisposition to acute myeloid leukemia. // Semin. Hematol. 2014. Vol. 51, № 4. P. 306–321.
11. Rubnitz J.E., Gibson B., Smith F.O. Acute Myeloid Leukemia // Hematology/Oncology Clinics of North America. 2010. Vol. 24, № 1. P. 35–63.
12. Agis H. et al. A comparative study on demographic, hematological, and cytogenetic findings and prognosis in acute myeloid leukemia with and without leukemia cutis. // Ann. Hematol. 2002. Vol. 81, № 2. P. 90–95.
13. Avni B. et al. Clinical implications of acute myeloid leukemia presenting as myeloid sarcoma. // Hematol. Oncol. 2012. Vol. 30, № 1. P. 34–40.
14. Creutzig U. et al. Diagnosis and management of acute myeloid leukemia in children and adolescents: Recommendations from an international expert panel // Blood. American Society of Hematology, 2012. Vol. 120, № 16. P. 3167–3205.
15. Ku G.H. et al. Venous thromboembolism in patients with acute leukemia: Incidence, risk factors, and effect on survival // Blood. 2009. Vol. 113, № 17. P. 3911–3917.
16. Муфтахова Г.М., Аксенова М.Е. Поздние эффекты противоопухолевой терапии со стороны мочеполовой системы (отсроченное влияние противоопухолевой терапии на органы мочеполовой системы) // Российский журнал детской гематологии и онкологии. 2019. Vol. 5, № 4. P. 114–119.
17. Fang R.C., Aboulafia D.M. HIV infection and myelodysplastic syndrome/acute myeloid leukemia // HIV-Associated Hematological Malignancies. 2016. P. 133–144.
18. Freeman A.J. et al. Estimating progression to cirrhosis in chronic hepatitis C virus infection. // Hepatology. 2001. Vol. 34, № 4 Pt 1. P. 809–816.
19. Ribas A. et al. How important is hepatitis C virus (HCV)-infection in persons with acute leukemia? // Leuk. Res. 1997. Vol. 21, № 8. P. 785–788.
20. Lam M.T. et al. Herpes simplex infection in acute myelogenous leukemia and other hematologic malignancies: a prospective study. // Cancer. 1981. Vol. 48, № 10. P. 2168–2171.
21. Averbuch D. et al. Targeted therapy against multi-resistant bacteria in leukemic and hematopoietic stem cell transplant recipients: Guidelines of the 4th European conference on Infections in Leukemia (ECIL-4, 2011) // Haematologica. 2013. Vol. 98, № 12. P. 1836–1847.
22. Averbuch D. et al. European guidelines for empirical antibacterial therapy for febrile neutropenic patients in the era of growing resistance: Summary of the 2011 4th European Conference on Infections in Leukemia // Haematologica. 2013. Vol. 98, № 12. P. 1826–1835.
23. Leahy M.F., Mukhtar S.A. From blood transfusion to patient blood management: a new paradigm for patient care and cost assessment of blood transfusion practice. // Intern. Med. J. 2012. Vol. 42, № 3. P. 332–338.
24. Döhner H. et al. Diagnosis and management of acute myeloid leukemia in adults: Recommendations from an international expert panel, on behalf of the European LeukemiaNet // Blood. 2010. Vol. 115, № 3. P. 453–474.
25. Döhner H. et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel // Blood. 2017. Vol. 129, № 4. P. 424–447.
26. Olsen R.J. et al. Acute leukemia immunohistochemistry: a systematic diagnostic approach. // Arch. Pathol. Lab. Med. 2008. Vol. 132, № 3. P. 462–475.
27. Bene M.C. et al. Proposals for the immunological classification of acute leukemias. European Group for the Immunological Characterization of Leukemias (EGIL). // Leukemia. 1995. Vol. 9, № 10. P. 1783–1786.
28. Wu D. et al. Efficacy and safety of different doses of cytarabine in consolidation therapy for adult acute myeloid leukemia patients: A network meta-analysis // Sci. Rep. 2017. Vol. 7, № 1. P. 9509.
29. Ravandi F., Walter R.B., Freeman S.D. Evaluating measurable residual disease in acute myeloid leukemia. // Blood Adv. 2018. Vol. 2, № 11. P. 1356–1366.
30. Лобанова Т.И., Гальцева И.В., Паровичникова Е.Н. Исследование минимальной остаточной болезни у пациентов с острыми миелоидными лейкозами методом многоцветной проточной цитофлуориметрии (обзор литературы) // Онкогематология. 2018. Vol. 13, № 1. P. 83–102.
31. Лобанова Т.И. “Клиренс опухолевого клона у пациентов с разными молекулярно-генетическими вариантами острых миелоидных лейкозов”: диссертация ... кандидата медицинских наук: 14.01.21. 2018. 166 p.
32. Herrmann J. et al. Evaluation and management of patients with heart disease and cancer: Cardio-oncology // Mayo Clin. Proc. 2014. Vol. 89, № 9. P. 1287–1306.
33. Roberts A.S. et al. Extramedullary haematopoiesis: radiological imaging features // Clinical Radiology. 2016. Vol. 71, № 9. P. 807–814.
34. Fritz J. et al. Radiologic spectrum of extramedullary relapse of myelogenous leukemia in adults. // AJR. Am. J. Roentgenol. 2007. Vol. 189, № 1. P. 209–218.
35. Arrigan M. et al. Imaging findings in recurrent extramedullary leukaemias // Cancer Imaging. 2013. Vol. 13, № 1. P. 26–35.
36. Almond L.M. et al. Myeloid Sarcoma: Presentation, Diagnosis, and Treatment // Clinical Lymphoma, Myeloma and Leukemia. Elsevier Inc., 2017. Vol. 17, № 5. P. 263–267.
37. Winestone L.E. et al. Disparities in pediatric acute myeloid leukemia (AML) clinical trial enrollment // Leuk. Lymphoma. Taylor and Francis Ltd, 2019. Vol. 60, № 9. P. 2190–2198.
38. Perel Y. et al. Treatment of childhood acute myeloblastic leukemia: Dose intensification improves outcome and maintenance therapy is of no benefit - Multicenter studies of the French LAME (Leucémie Aiguë Myéloblastique Enfant) Cooperative Group // Leukemia. Nature Publishing Group, 2005. Vol. 19, № 12. P. 2082–2089.
39. Rasche M. et al. Successes and challenges in the treatment of pediatric acute myeloid leukemia: a retrospective analysis of the AML-BFM trials from 1987 to 2012 // Leukemia. Nature Publishing Group, 2018. Vol. 32, № 10. P. 2167–2177.
40. Шнейдер М.М. Эффективность риск-адаптированной терапии острого миелоидного лейкоза у детей с использованием режимов интенсивного тайминга и трансплантации гемопоэтических стволовых клеток. Диссертация на соискание ученой степени доктора медицинских наук. 2009. 223 p.
41. Olmos-Jiménez R. et al. Practical aspects of the use of intrathecal chemotherapy Aspectos prácticos de la utilización de quimioterapia intratecal // Farm Hosp. 2017. Vol. 41, № 1. P. 105–129.
42. Creutzig U. et al. CNS irradiation in pediatric acute myleoid leukemia: Equal results by 12 or 18 Gy in studies AML-BFM98 and 2004 // Pediatr. Blood Cancer. 2011. Vol. 57, № 6. P. 986–992.
43. Stevens R.F. et al. Marked improvements in outcome with chemotherapy alone in paediatric acute myeloid leukaemia: Results of the United Kingdom Medical Research Council’s 10th AML trial // Br. J. Haematol. 1998. Vol. 101, № 1. P. 130–140.
44. Ravindranath Y. et al. Pediatric Oncology Group (POG) studies of acute myeloid leukemia (AML): A review of four consecutive childhood AML trials conducted between 1981 and 2000 // Leukemia. Nature Publishing Group, 2005. Vol. 19, № 12. P. 2101–2116.
45. Kardos G. et al. Treatment strategy and results in children treated on three Dutch Childhood Oncology Group acute myeloid leukemia trials // Leukemia. Nature Publishing Group, 2005. Vol. 19, № 12. P. 2063–2071.
46. Smith F.O. et al. Long-term results of children with acute myeloid leukemia: A report of three consecutive Phase III trials by the Children’s Cancer Group: CCG 251, CCG 213 and CCG 2891 // Leukemia. Nature Publishing Group, 2005. Vol. 19, № 12. P. 2054–2062.
47. Perel Y. et al. Maintenance therapy in childhood acute myeloid leukemia // Ann. Hematol. 2004. Vol. Supp. 1. P. S116–S119.
48. Toyama D. et al. Successful Treatment of Pediatric Refractory/Relapsed AML with KIR-Ligand-Mismatched Cord Blood Transplant after FLAG-IDA Reinduction Therapy with or without the GO Regimen // Case Rep. Hematol. Hindawi Limited, 2020. Vol. 2020.
49. Hashmi K.U. et al. FLAG-IDA in the treatment of refractory/relapsed acute leukaemias: Single centre study // J. Pak. Med. Assoc. 2005. Vol. 55, № 6. P. 234–238.
50. Safaian N.N. et al. Sorafenib (Nexavar®) induces molecular remission and regression of extramedullary disease in a patient with FLT3-ITD+ acute myeloid leukemia // Leuk. Res. 2009. Vol. 33, № 2. P. 348–350.
51. Osone S. et al. Sorafenib Therapy for Pediatric Acute Myeloid Leukemia with FMS-like Tyrosine Kinase 3 -internal Tandem Duplication Mutations: 2 Case Reports // J. Pediatr. Hematol. Oncol. Lippincott Williams and Wilkins, 2017. Vol. 39, № 4. P. e199–e202.
52. Crews K.R. et al. Interim comparison of a continuous infusion versus a short daily infusion of cytarabine given in combination with cladribine for pediatric acute myeloid leukemia // J. Clin. Oncol. 2002. Vol. 20, № 20. P. 4217–4224.
53. Румянцев А.Г., Масчан А.А., Самочатова Е.В. Сопроводительная терапия и контроль инфекций при гематологических и онкологических заболеваниях. 2009. 448 p.
54. Coiffier B. et al. Guidelines for the management of pediatric and adult tumor lysis syndrome: An evidence-based review // Journal of Clinical Oncology. 2008. Vol. 26, № 16. P. 2767–2778.
55. Cairo M.S. et al. Recommendations for the evaluation of risk and prophylaxis of tumour lysis syndrome (TLS) in adults and children with malignant diseases: An expert TLS panel consensus // Br. J. Haematol. 2010. Vol. 149, № 4. P. 578–586.
56. Детская онкология. Национальное руководство. Под ред. М.Д. Алиева, В.Г. Полякова, Г.Л. Менткевича, С.А. Маяковой. М.: Издательская группа РОНЦ. Практическая медицина, 2012. 684 p.
57. Maertens J. et al. ECIL guidelines for preventing Pneumocystis jirovecii pneumonia in patients with haematological malignancies and stem cell transplant recipients // J. Antimicrobal Chemother. 2016. Vol. 71, № 9. P. 2397–2404.
58. Chen M. et al. Pyridoxine for Prevention of Hand-Foot Syndrome Caused by Chemotherapy: A Systematic Review // PLoS One. Public Library of Science, 2013. Vol. 8, № 8.
59. Korula A. et al. Invasive fungal infection following chemotherapy for acute myeloid leukaemia—Experience from a developing country // Mycoses. Blackwell Publishing Ltd, 2017. Vol. 60, № 10. P. 686–691.
60. Fisher B.T. et al. Effect of Caspofungin vs Fluconazole Prophylaxis on Invasive Fungal Disease among Children and Young Adults with Acute Myeloid Leukemia: A Randomized Clinical Trial // JAMA - J. Am. Med. Assoc. American Medical Association, 2019. Vol. 322, № 17. P. 1673–1681.
61. Mandhaniya S. et al. Oral voriconazole versus intravenous low dose amphotericin B for primary antifungal prophylaxis in pediatric acute leukemia induction: A prospective, randomized, clinical study // J. Pediatr. Hematol. Oncol. 2011. Vol. 33, № 8. P. e333-41.
62. Cornely O.A. et al. Posaconazole vs. fluconazole or itraconazole prophylaxis in patients with neutropenia // N. Engl. J. Med. Massachussetts Medical Society, 2007. Vol. 356, № 4. P. 348–359.
63. Ueda M. et al. Immunoglobulin therapy in hematologic neoplasms and after hematopoietic cell transplantation. // Blood Rev. 2018. Vol. 32, № 2. P. 106–115.
64. Nellis M.E., Goel R., Karam O. Transfusion Management in Pediatric Oncology Patients // Hematology/Oncology Clinics of North America. W.B. Saunders, 2019. Vol. 33, № 5. P. 903–913.
65. Szczepiorkowski Z.M., Dunbar N.M. Transfusion guidelines: when to transfuse. // Hematology / the Education Program of the American Society of Hematology. American Society of Hematology. Education Program. 2013. Vol. 2013. P. 638–644.
66. Абузарова Г.Р. et al. Обезболивание взрослых и детей при оказании медицинской помощи. Методические рекомендации. ФГБОУ ВО РНИМУ им. Н.И. Пирогова Минздрава России., 2016. 94 p.
67. Paul K.L. Rehabilitation and exercise considerations in hematologic malignancies. // Am. J. Phys. Med. Rehabil. 2011. Vol. 90, № 5 Suppl 1. P. S88-94.
68. Tramsen L. et al. Lack of effectiveness of neutropenic diet and social restrictions as anti-infective measures in children with acute myeloid leukemia: An analysis of the AML-BFM 2004 trial // J. Clin. Oncol. American Society of Clinical Oncology, 2016. Vol. 34, № 23. P. 2776–2783.
69. Milligan D.W. et al. Fludarabine and cytosine are less effective than standard ADE chemotherapy in high-risk acute myeloid leukemia, and addition of G-CSF and ATRA are not beneficial: Results of the MRC AML-HR randomized trial // Blood. American Society of Hematology, 2006. Vol. 107, № 12. P. 4614–4622.
70. Gibson B.E.S. et al. Results of a randomized trial in children with Acute Myeloid Leukaemia: Medical Research Council AML12 trial // Br. J. Haematol. 2011. Vol. 155, № 3. P. 366–376.
71. Creutzig U. et al. Toxicity and effectivity of high-dose Idarubicin during AML induction therapy: Results of a pilot study in children // Klin. Padiatr. 2000. Vol. 212, № 4. P. 163–168.
72. Creutzig U. et al. Improved treatment results in high-risk pediatric acute myeloid leukemia patients after intensification with high-dose cytarabine and mitoxantrone: Results of study acute myeloid Leukemia-Berlin-Frankfurt-Münster 93 // J. Clin. Oncol. Lippincott Williams and Wilkins, 2001. Vol. 19, № 10. P. 2705–2713.
73. Acute myeloid leukemia. NCCN evidence blocks. 2020.
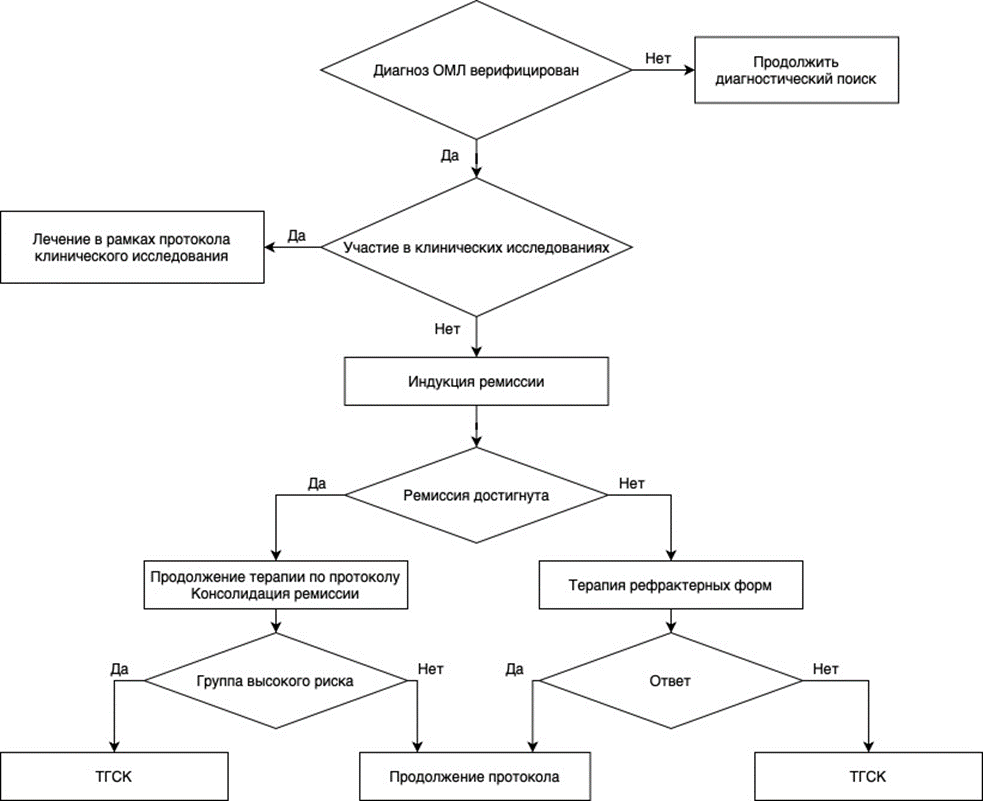
74. Uffmann M. et al. Therapy reduction in patients with Down syndrome and myeloid leukemia: the international ML-DS 2006 trial // Blood. American Society of Hematology, 2017. Vol. 129, № 25. P. 3314–3321.
75. Cornelissen J.J. et al. The European LeukemiaNet AML Working Party consensus statement on allogeneic HSCT for patients with AML in remission: An integrated-risk adapted approach // Nature Reviews Clinical Oncology. 2012. Vol. 9, № 10. P. 579–590 76.
76. Abildgaard L, Ellebaek E, Gustafsson G, Abrahamsson J, Hovi L, Jonmundsson G, Zeller B, Hasle H. Optimal treatment intensity in children with Down syndrome and myeloid leukaemia: data from 56 children treated on NOPHO-AML protocols and a review of the literature. Ann Hematol. 2006 May;85(5):275-80.
77. Hassler A, Bochennek K, Gilfert J, Perner C, Schöning S, Creutzig U, Reinhardt D, Lehrnbecher T. Infectious Complications in Children With Acute Myeloid Leukemia and Down Syndrome: Analysis of the Prospective Multicenter Trial AML-BFM 2004. Pediatr Blood Cancer. 2016 Jun;63(6):1070-4.
78. Bertrums EJM, Zwaan CM, Hasegawa D, De Haas V, Reinhardt DN, Locatelli F, De Moerloose B, Dworzak M, Buijs A, Smisek P, Kolenova A, Pronk CJ, Klusmann JH,
Carboné A, Ferster A, Antoniou E, Meshinchi S, Raimondi SC, Niemeyer CM, Hasle H, Van den Heuvel-Eibrink MM, Goemans BF. Guideline for management of non-Down
syndrome neonates with a myeloproliferative disease on behalf of the I-BFM AML Study Group and EWOG-MDS. Haematologica. 2022 Mar 1;107(3):759-764.
79. Kudo K, Hama A, Kojima S, Ishii R, Morimoto A, Bessho F, Sunami S, Kobayashi N, Kinoshita A, Okimoto Y, Tawa A, Tsukimoto I. Mosaic Down syndrome-associated
acute myeloid leukemia does not require high-dose cytarabine treatment for induction and consolidation therapy. Int J Hematol. 2010 May;91(4):630-5
80. Taga T, Shimomura Y, Horikoshi Y, Ogawa A, Itoh M, Okada M, Ueyama J, Higa T, Watanabe A, Kanegane H, Iwai A, Saiwakawa Y, Kogawa K, Yamanaka J, Tsurusawa M.
Continuous and high-dose cytarabine combined chemotherapy in children with down syndrome and acute myeloid leukemia: Report from the Japanese children's cancer
and leukemia study group (JCCLSG) AML 9805 down study. Pediatr Blood Cancer. 2011 Jul 15;57(1):36-40.
81. Ravindranath Y, Abella E, Krischer JP, Wiley J, Inoue S, Harris M, Chauvenet A, Alvarado CS, Dubowy R, Ritchey AK, et al. Acute myeloid leukemia (AML) in
Down's syndrome is highly responsive to chemotherapy: experience on Pediatric Oncology Group AML Study 8498. Blood. 1992 Nov 1;80(9):2210-4.
82. Uffmann M, Rasche M, Zimmermann M, von Neuhoff C, Creutzig U, Dworzak M, Scheffers L, Hasle H, Zwaan CM, Reinhardt D, Klusmann JH. Therapy reduction in
patients with Down syndrome and myeloid leukemia: the international ML-DS 2006 trial. Blood. 2017 Jun 22;129(25):3314-3321.
83. Lange BJ, Kobrinsky N, Barnard DR, Arthur DC, Buckley JD, Howells WB, Gold S, Sanders J, Neudorf S, Smith FO, Woods WG. Distinctive demography, biology, and outcome of acute myeloid leukemia and myelodysplastic syndrome in children with Down syndrome: Children's Cancer Group Studies 2861 and 2891. Blood. 1998 Jan 15;91(2):608-15
84. Инструкция по медицинскому применению лекарственного препарата Венклекста. Государственный реестр лекарственных средств: https://grls.rosminzdrav.ru/Grls_View_v2.aspx?routingGuid=a1111a51-349d-4ff6-b92a-40e2bc0da33d Доступ от 17.04.2023.
85. Omima M, Khalid A, Aeshah A, Naglla E, Mohammed B.A. and Wasil J. FLAG/FLAG-IDA regimen for children with relapsed/refractory acute leukemiain the era of targeted novel therapies. Journal of Oncology Pharmacy Practice. 2019. Vol. 25(8): 1831-1838
86. Международных рекомендациях Национального онкологического общества по терапии ОМЛ (NCCN), США. Международные рекомендации Национального онкологического общества (NCCN), США (NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Acute Myeloid leukemia Version. 2. 2023) [Электронный ресурс]. Доступ от 22.03.2023. Режим доступа: https://www.nccn.org/professionals/physician_gls/pdf/aml.pdf
87. Европейских рекомендациях по лечению острого миелоидного лейкоза (ESMO). Европейские рекомендации по лечению острого миелоидного лейкоза (Acute myeloid leukaemia in adult patients: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up) Heuser M, Ofran Y, Boissel N, Mauri SB, Craddock C, Janssen J,Wierzbowska A, Buske C, on behalf of the ESMO Guidelines Committee, Acute myeloid leukaemia inadult patients: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up†, Annals of Oncology (2020), [Электронный ресурс]. Доступ от 22.03.2023. Режим доступа: https://www.annalsofoncology.org/article/S0923-7534(20)36079-8/fulltext
88. Trus MR, Yang L, Saiz FSet al. The histone deacetylase inhibitor valproic acid alters sensitivity towards all trans retinoic acid in acute myeloblastic leukemia cells. Leukemia. 2005;19:1161–1168. doi: 10.1038/sj.leu.2403773.
89. Попа А.В., Горохова Е.В., Флейшман Е.В. и др. Эпигенетическая терапия – важная составляющая в лечении детей, больных острым миелоидным лейкозом. Клиническая онкогематология. 2011;4(1):20–26.
90. А. В. Попа, В. С. Немировченко, Е. В. Флейшман, О. И. Сокова, Н. Н. Субботина, И. Н. Серебрякова, Л. Ю. Гривцова, Г. Л. Менткевич. Ингибиторы гистондеацетилазы и ДНК-метилтрансферазы в лечении детей, больных острым миелоидным лейкозом, их эффективность и место в терапии. Российский журнал детской гематологии и онкологии. 2016, Т. 3, №4, с.48-54
91. А.В. Попа, О.А. Тиганова, О.И. Сокова, Н.Н. Субботина, Ю.В. Ольшанская, Б.В. Курдюков, И.Н. Серебрякова, А.Д. Палладина, Н.Н. Тупицын, О.Б. Курасова, А.Б. Моисеев, Г.Л. Менткевич. Значение эпигенетической терапии в лечении детей, больных острым миелоидным лейкозом. Вопросы онкологии, гематологии, иммунологии 2025, 24(1) (статья сдана в печать).
92 Г.А. Новичкова, А.В. Попа, А.А. Масчан и др. Промежуточные результаты лечения детей с ОМЛ по протоколу AML MRD-2018. Вопросы онкологии, гематологии, иммунологии 2025, 24(1) (статья сдана в печать).
93. Tierens A, Arad-Cohen N, Cheuk D, De Moerloose B, Fernandez Navarro JM, Hasle H, Jahnukainen K, Juul-Dam KL, Kaspers G, Kovalova Z, Lausen B, Norén-Nyström U, Palle J, Pasauliene R, Jan Pronk C, Saks K, Zeller B, Abrahamsson J. Mitoxantrone Versus Liposomal Daunorubicin in Induction of Pediatric AML With Risk Stratification Based on Flow Cytometry Measurement of Residual Disease. J Clin Oncol. 2024 Jun 20;42(18):2174-2185. doi: 10.1200/JCO.23.01841
94. Saro H. Armenian, and Matthew J. Ehrhardt. Optimizing Cardiovascular Care in Children With Acute Myeloid Leukemia to Improve Cancer-Related Outcomes. JCO. 2018; 37(1): 1-7
95. Katerin Tarlock, Todd A Alonzo, Robert B G
erbing, Susana C Raimondi, et al. Gemtuzumab ozogamicin reduces relapse risk in FLT3/ITD acute myeloid leukemia: a report from the Children’s Oncology Group. Clin Cancer Res. 2016 April 15; 22(8): 1951–1957. doi:10.1158/1078-0432.CCR-15-1349
96. Creutzig U, Zimmermann M, Ritter О, Reinhardt D, et al. Treatment strategies and long-term results in pediatric patients treated in four consecutive AML-BFM trials. Leukemia.2005; 19:2030–2042. DOI: 10.1038/sj.leu.2403920
97. Rasche M, Zimmermann M, Borschel L, et al. Successes and challenges in the treatment of pediatric acute myeloid leukemia: a retrospective analysis of the AML-BFM trials from 1987 to 2012. Leukemia. 2018; 32: 2167–2177. DOI: 10.1038/s41375-018-0071-7
98. Adriana Trabal, Amber Gibson, Jiasen HeM, et al/ Venetoclax for Acute Myeloid Leukemia in Pediatric Patients: A Texas Medical Center Experience. Cancers 2023, 15:1983-1999. https://doi.org/10.3390/ cancers15071983
99. Mathilde Penel-Page, Adriana Plesa, Sandrine Girard, et al. Association of fludarabin, cytarabine, and fractioned gemtuzumab followed by hematopoietic stem cell transplantation for first-line refractory acute myeloid leukemia in children: A single-center experience. Pediatr Blood Cancer. 2020; 67:e28305. DOI: 10.1002/pbc.28305
100. Todd M. Coope, Janet Franklin, Robert B. Gerbing et al. MD15AAML03P1, a Pilot Study of the Safety ofGemtuzumab Ozogamicin in CombinationWith Chemotherapy for Newly DiagnosedChildhood Acute Myeloid Leukemia. Cancer, 2012, v.118, issure 3, pp 579-769
101. U. Creutzig, M. Zimmermann, J-P Bourquin et al. Favorable outcome in infants with AML after intensive first- and second-line treatment: an AML-BFM study group report. Leukemia (2012) 26, 654–661. doi:10.1038/leu.2011.267
102. Creutzig U, Zimmermann M, Lehrnbecher T, Graf N, Hermann J, Niemeyer CM, et al. Less toxicity by optimizing chemotherapy, but not by addition of granulocyte colony-stimulating factor in children and adolescents with acute myeloid leukemia: results of AML-BFM 98. J Clin Oncol. 2006; 24:4499–506.
103. Tavil B., Aytac S., MD, Balcı YI et al. Fludarabine, cytarabine, granulocyte colony-stimulating factor, and idarubicin (flag-ida) for the treatment of children with poor-prognosis acute leukemia: the hacettepe experience. Pediatr Hematol Oncol. 2010; 27(7): 517-528
104. Jeffrey E. Rubnitz, Hiroto Inaba, Gary Dahl et al. Minimal Residual Disease-Directed Therapy for Childhood Acute Myeloid Leukemia: Results of the AML02 Multicenter Trial. Lancet Oncol. 2010 June ; 11(6): 543–552. doi:10.1016/S1470-2045(10)70090-5
105. Kuderer NM, Dale DC, Crawford J, Cosler LE, Lyman GH. Mortality, morbidity and cost associated with febrile neutropenia in adult cancer patients. Cancer, 2006; 106(10): 2258-2266
106. Mikulska M, Viscoli C, Orasch C, Livermore DM, Averbuch D, Cordonnier C et al. Aetiology and resistance in bacteriaemias among adult and paediatric haematology and cancer patients. Jornal of infection (2014), 68: 321-331
107. Lyman GH, Rolston KVI. How we treat febrile neutropenia in patients receiving cancer chemotherapy. Journal of oncology practice, 2010; 6(3): 149-152
108. Averbuch D, Orasch C, Cordonnier C, Livermore DM, Mikulska M, Viscoli C et al. European guidelines for empirical antibacterial therapy for febrile neutropenic patients in the era of growing resistance: summary of the 2011 4th European Conference of Infections in Luekemia. Нaematologica 2013; 98 (12): 1826-1835
109. De la Court J.R. et al The Dutch working party on antibiotic policy (SWAB) recommendation for the diagnosis and management of febrile neutropenia in patients with cancer.// Infect Dis Ther 2022; 11(6): 2063-2098
110. Hakim H, Flynn PM, Knapp KM, Srivastava DK, Gaur AH. Etiology and clinical course of febrile neutropenia in children with cancer. J Pediatr Hematol Oncol, 2009; 31(9): 623-629
111. Hartman S et al A new Framework to implement model-informed dosing in clinical guidelines: piperacillin and amikacin as proof of concept.// Front Pharmacol 2020; 11:592204
112. Miranda M., Nadel S. Pediatric Sepsis: a Summary of Current Definitions and Management Recommendations // Curr Pediatr Rep. Springer Nature, 2023. Vol. 11, № 2. P. 29–39.
113. Lehrnbecher T, Phillips R, Alexander S, Alvaro F, Carlesse F, Fisher B et al. Guidlenes for the management of fever and neutropenia in children with cancer and/or undergoing hematopoietic stem-cell transplantation. J Сlin Оncol, 2012; 30(35): 4427-4438
114. Simon A. et al. Surveillance of bloodstream infections in pediatric cancer centers – what have we learned and how do we move on? // GMS Hyg Infect Control. German Medical Science, 2016. Vol. 11. P. Doc11.
115. Bard J.D., TeKippe E.M.E. Diagnosis of Bloodstream Infections in Children // J Clin Microbiol. J Clin Microbiol, 2016. Vol. 54, № 6. P. 1418–1424.
116. Petty L.A. et al. Repeated Blood Cultures in Pediatric Febrile Neutropenia: Would Following the Guidelines Alter the Outcome? // Pediatr Blood Cancer. Pediatr Blood Cancer, 2016. Vol. 63, № 7. P. 1244–1249.
117. Scheler M. et al. Management of children with fever and neutropenia: results of a survey in 51 pediatric cancer centers in Germany, Austria, and Switzerland // Infection. Springer Science and Business Media Deutschland GmbH, 2020. Vol. 48, № 4. P. 607–618.
118. Lee A. et al. Detection of bloodstream infections in adults: how many blood cultures are needed? // J Clin Microbiol. J Clin Microbiol, 2007. Vol. 45, № 11. P. 3546–3548.
119. Белобородов В.Б., Голощапов О.В., Гусаров В.Г., Дехнич А.В., Замятин М.Н., Зубарева Н.А., Зырянов С.К., Камышова Д.А., Климко Н.Н., Козлов Р.С., Кулабухов В.В., Петрушин М.А., Полушин Ю.С., Попов Д.А., Руднов В.А., Сидоренко С.В., Соколов Д.В., Шлык И.В., Эйдельштейн М.В., Яковлев С.В. Методические рекомендации Российской некоммерческой общественной организации «Ассоциация анестезиологов-реаниматологов», Межрегиональной общественной организации «Альянс клинических химиотерапевтов и микробиологов», Межрегиональной ассоциации по клинической микробиологии и антимикробной химиотерапии (МАКМАХ), общественной организации «Российский Сепсис Форум» «Диагностика и антимикробная терапия инфекций, вызванных полирезистентными штаммами микроорганизмов» (обновление 2022 г.). Вестник анестезиологии и реаниматологии. 2022;19(2):84-114. https://doi.org/10.21292/2078-5658-2022-19-2-84-114
120. Cattaneo C. et al. Bloodstream infections in haematological cancer patients colonized by multidrug-resistant bacteria // Annals of Hematology, 2018 Vol.97, p. 1717-1726.
121. Jaiswal S.R. et al. Gut Colonization with Carbapenem-resistant Enterobacteriaceae Adversely Impacts the Outcome in Patients with Hematological Malignancies: Results of A Prospective Surveillance Study // Mediterr J Hematol Infect Dis. Catholic University in Rome, 2018. Vol. 10, № 1. P. 2018025.
122. Girmenia C. et al. Incidence, Risk Factors and Outcome of Pre-engraftment Gram-Negative Bacteremia After Allogeneic and Autologous Hematopoietic Stem Cell Transplantation: An Italian Prospective Multicenter Survey // Clin Infect Dis. Clin Infect Dis, 2017. Vol. 65, № 11. P. 1884–1896.
123. Tang Girdwood S. et al β-lactam precision dosing in critically ill children: current state and knowledge gaps// Front Pharmacol 2022; 13:1044683
124. Morrissey C., Gilroy N., Macesic N., Walker P., Nanda-Rajah M. et al. Consensus guidelines for the use of empiric and diagnostic-driven antifungal treatment strategies in haematological malignancy, 2014. Intern Med J, 2014; 44: 1298–1314.
125. Groll AH, Werner C, Tebbe J, Solopova G, Becker K et al. Pulmonale Infectionen in der pädiatrischen Hämatologie und Oncologie. Monatsschr Kinderheilkd, 2011; 159: 233-241
126. Ruhnke M and Schwartz S. Recent developments in the management of invasive fungal infections in patients with oncohematological diseases. Ther Adv Hematol, 2016; 7(6): 345–359
127. Tissot F., Agrawai S., Pagano L., Petrikkos G., Groll A.H. et al. ECIL-6 Guidelines for the Treatment of Invasive Candidiasis, Aspergillosis and Mucormycosis in Liekemia and Hematopoietic Stem Cell Transplant Patients. Hematologica, 2017; 102: 433-444
128. Heussel C., Kauczor H., Heussel G., Fischer B., Begrich M. et al. Pneumonia in febrile neutropenic patients and in bone marrow and blood stem-cell transplant recipients: use of high-resolution computed tomography. J Clin Oncol, 1999; 17: 796–805.
129. Новичкова Г.А., Горонкова О.В., Балашов Д.Н., Байдильдина Д.Д., Жарикова Л.И. и др. Диагностика, клиника и лечение инвазивного аспергиллеза у детей с приобретенной апластической анемией: анализ 20 собственных случаев. Гематология и трансфузиология, январь 2005.
130. Soudani N. et al Prevalence and characteristics of acute respiratory virus infections in pediatric cancer patients // J Med Virol 2019; 91(7): 1191-1201.
131. Солопова Г.Г., Цыганова Е.В., Кондрашова А.В., Гордеева Г.Н., Розанцева Е.В., Бегунова С.В., Воронин К.А., Копосова А.О., Новичкова Г.А. «Особенности течения новой коронавирусной инфекции COVID-19 у детей с онкологическими, онкогематологическими и тяжелыми иммунологическими заболеваниями. Опыт НМИЦ ДГОИ им. Дмитрия Рогачева». Вопросы гематологии/онкологии и иммунопатологии в педиатрии 2021 т.20 №4: 89-99
132. Righini-Grunder F et al/ Frequency of oral mucositis and local virus reactivation in herpes simplex virus seropositive children with myelosupressive therapy// Klin Padiatr. 2015; 227(6-7): 335-8
133. Spruit J L, Knight T, Sweeney C, Salimnia H, Savaşan S. Clostridium difficile infection in a children's hospital with specific patterns among pediatric oncology and hematopoietic stem cell transplantation populations Pediatr Hematol Oncol. 2020 Apr;37(3):211-222. doi: 10.1080/08880018.2019.1711473
134. Tai E, Richardson LC, Townsend J, Howard E, Mcdonald LC Clostridium difficile infection among children with cancer Pediatr Infect Dis J. 2011 Jul;30(7):610-2.
135. Castagnola E., Ruberto E., Guarino A. Gastrointestinal and liver infections in children undergoing antineoplastic chemotherapy in the years 2000 // World J Gastroenterol. Baishideng Publishing Group Inc, 2016. Vol. 22, № 25. P. 5853.
136. Maertens J.A. et al. Optimization of the cutoff value for the Aspergillus double-sandwich enzyme immunoassay // Clin Infect Dis. Clin Infect Dis, 2007. Vol. 44, № 10. P. 1329–1336.
137. Lehrnbecher T, Robinson PD, Fisher BT, Castagnola E, Groll AH, Steinbach WJ, Zaoutis TE, Negeri ZF, Beyene J, Phillips B, Sung L. Galactomannan, β-D-Glucan, and Polymerase Chain Reaction-Based Assays for the Diagnosis of Invasive Fungal Disease in Pediatric Cancer and Hematopoietic Stem Cell Transplantation: A Systematic Review and Meta-Analysis. Clin Infect Dis. 2016 Nov 15;63(10):1340-1348. doi: 10.1093/cid/ciw592
138. Warris A , Lehrnbecher T Progress in the Diagnosis of Invasive Fungal Disease in Children Curr Fungal Infect Rep. 2017;11(2):35-44. doi: 10.1007/s12281-017-0274-9.
139. Gupta A, Capoor MR, Shende T, Sharma B, Mohindra R, Suri JC, Gupta DK. Comparative evaluation of galactomannan test with bronchoalveolar lavage and serum for the diagnosis of invasive aspergillosis in patients with hematological malignancies.
J Lab Physicians. 2017 Oct-Dec;9(4):234-238. doi: 10.4103/JLP.JLP_127_16.
140. Mikulska M, Calandra T, Sanguinetti M, Poulain D, Viscoli C. The use of mannan antigen and anti-mannan antibodies in the diagnosis of invasive candidiasis: recommendations from the Third European Conference on Infections in Leukemia.
Crit Care. 2010;14(6):R222. doi: 10.1186/cc9365
141. Fisher BT et al Multicenter prospective study of biomarkers for diagnosis of invasive candidiasis in children and adolescents.// Clin Infect Dis 2022; 75(2): 248-259
142. Chang CC, Harrison TS, Bicanic TA, Chayakulkeeree M, Sorrell TC, Warris A, et al. Global guideline for the diagnosis and management of cryptococcosis: an initiative of the ECMM and ISHAM in cooperation with the ASM. . Lancet Infect Dis. 2024 Feb 9:S1473-3099(23)00731-4. doi: 10.1016/S1473-3099(23)00731-4.
143. Freifeld A.G. et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of america // Clin Infect Dis. Clin Infect Dis, 2011. Vol. 52, № 4.
144. Lehrnbecher T, Robinson P, Fisher B, Alexander S, Ammann RA, et al. Guideline for the Management of Fever and Neutropenia in Children With Cancer and Hematopoietic Stem-Cell Transplantation Recipients: 2017 Update. J Clin Oncol. 2017 Jun 20;35(18):2082-2094. doi: 10.1200/JCO.2016.71.7017
145. Lehrnbecher T. et al. Guideline for the Management of Fever and Neutropenia in Pediatric Patients With Cancer and Hematopoietic Cell Transplantation Recipients: 2023 Update // J Clin Oncol. J Clin Oncol, 2023. Vol. 41, № 9. P. 1774–1785.
146. Lehrnbecher T. et al. 8th European Conference on Infections in Leukaemia: 2020 guidelines for the use of antibiotics in paediatric patients with cancer or post-haematopoietic cell transplantation // Lancet Oncol. Lancet Oncol, 2021. Vol. 22, № 6. P. e270–e280.
147. Солопова Г.Г., Новичкова Г.А. Опыт внедрения алгоритма эмпирической антибактериальной терапии при развитии фебрильной нейтропении в Центре детской гематологии/онкологии // Вопросы гематологии/онкологии и иммунопатологии в педиатрии. 2017. Vol. 16, № 3. P. 35–47.
148. Lehrnbecher Т. Treatment of fever in neutropenia in pediatric oncology patients Current Opinion in Pediatrics 31(1):p 35-40, February 2019. | DOI: 10.1097/MOP.0000000000000708
149. Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H et al. Surviving sepsis campain: international guidlines for management of severe sepsis and septic shock, 2012. Intensive Care Med, 2013; 39(2): 165-228
150. Ferrer R. et al. Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: results from a guideline-based performance improvement program // Crit Care Med. Crit Care Med, 2014. Vol. 42, № 8. P. 1749–1755.
151. Van Vliet M. et al. How prompt is prompt in daily practice? Earlier initiation of empirical antibacterial therapy for the febrile neutropenic patient // Eur J Cancer Care (Engl). Eur J Cancer Care (Engl), 2011. Vol. 20, № 5. P. 679–685.
152. Morales Castro D. et al. Pharmacokinetic Alterations Associated with Critical Illness // Clin Pharmacokinet. Adis, 2023. Vol. 62, № 2. P. 209–220.
153. Groll AH et al Fourth European conference on infections in luekaemia (ECIL-4): guidelines for diagnosis, prevention, and treatment of invasive fungal diseases in paediatric patients with cancer or allogeneic hematopoietic stem-cell transplantation.//Lancet.Oncol. 2014;15:327-340
154. Groll AH, Pana D, Lanternier F, Mesini A, Ammann RA8th European Conference on Infections in Leukaemia: 2020 guidelines for the diagnosis, prevention, and treatment of invasive fungal diseases in paediatric patients with cancer or post-haematopoietic cell transplantation. Lancet Oncol. 2021 Jun;22(6):e254-e269. doi: 10.1016/S1470-2045(20)30723-3
155. Солопова Г.Г., Масчан А.А., Новичкова Г.Г. «Рекомендации 2020 года по диагностике и терапии инвазивного аспергиллеза у детей с онкогематологическими заболеваниями». Вопросы гематологии/онкологии и иммунопатологии. 2020 т.19 №1, стр. 158-166
156. Soler-Palacin P. et al Voriconazole drug monitoring in the management of invasive fungal infection in immunocompromised children: a prospective trile. J Antimicrob Chemother 2012; 67(3):700-706
157. Papachristou S. et al Invasive aspergillosis in pediatric leukemia patients: prevention and treatment.// J Fungi 2019; 5(1):14
158. De Pauw B., Walsh T.J., Donnelly J.P., Stevens E.E., Edwards J.E. et al. Revised Definitions of Invasive Fungal Disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis, 2008; 46(12): 1813-1821
159. Patterson TF, Thompson GR, Denning DW, Fishman JA, Hadley S et al. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the infectious diseases society of America. Clin Infect Dis, 2016; 63(4): e1 – e60
160. Hsu AJ. Et al Challenges in the treatment of invasive aspergillosis in immunocompromised children.//Antimicrob Agents Chemother 2022; 66(7): e02156-21
161. Cornely O., Rikan-Akdagli S., Dannaoui E., Groll A., Lagrou, K. et al. ESCMID and ECMM joint clinical guidelines for the diagnosis and management of mucormycosis 2013. Clin Microbiol Infect, 2014; 20 (Suppl. 3): 5–26
162. Солопова Г.Г, Рачков В.Е., Ускова Н.Г., Оганесян Р.С., Коновалов Д.М. и Новичкова Г.А. Мукормикоз гастроинтестинальной локализации у пациента с острым миелобластным лейкозом. Вопросы гематологии/онкологии и иммунопатологии в педиатрии, 2014; 13(4): 69 – 74
163. Pana Z., Seidel D., Skiada A., Groll A., Petrikkos G. et al. Invasive mucormycosis in children: an epidemiologic study in European and non-European countries based on two registries. BMC Infect Dis, 2016;16(1):667
164. Liu L-P et al High risk of bloodstream infection of carbapenem-resisstant Enterobacteriaceae carriers in neutropenic children with hematological diseases.//Antimicrob Resist Infect Control.2023; 12(1):66
165. Castagnola E. Et al/ Antibiotic Resistant Bloodstream Infections in Pediatric Patients Receveiving Chemotherapy or Hematopoietic Stem Cell Transplant: Factors Associated with Development of Resistance, Intensive Care Admission and Mortality// Antibiotics 2021; 10(3): 266
166. Kontou A. et al. Use of newer and repurposed antibiotics against gram-negative bacteria in neonates.// Antibiotics 2023; 12(6):1072
167. Chiotos K. et al Treatment of carbapenem-resistant Enterobacteriaceae incections in children
168. Hassan H et al Dosage regimen for meropenem in children with Pseudomonas infections do not meet serum concentration targets.//Clin Transl Sci 2020; 13(2):301-308
169. Patel K, Goldman J L. Safety Concerns Surrounding Quinolone Use in children.// J Clin Pharmacol 2016; 56(9):1060-1075
170. Aslan K. et al Clinical and laboratory responses to tigecycline in children.// J Clin Pharm Ther 2022; 47(10):1585-1590
171. Rodriguez BA et al. Ceftazidime/avibactam and ceftalosane/tazobactam: novel therapy for multidrug resistant gram negative infections in children
172. Papachatzi E et al Daptomycin use for persistent coagulase-negative staphylococcal bacteremia in a neonatal intensive care unit.//Antibiotics 2024; 13(3): 254
173. Decembrino N et al A case series and literature review of isavuconazole use in pediatric patients with hemato-oncologic diseases and hematopoietic stem cell transplantation.// Antimicrob Agents Chemother 2020; 64(3): e01783-19
174. Fernandez Ladesma B et al Isavuconazole use and TDM in real-word pediatric practice.// Antimicrob Agents Chemother 2023; 67(12): e00829-23
175. SO Lie, J Abrahamsson, N Clausen et al. Long-term results in children with AML: NOPHO-AML Study Group – report of three consecutive trials. Leukemia. 2005. Vol. 19: 2090–2100
176. Wang Q. et al. Venetoclax for arsenic-resistant acute promyelocytic leukaemia. Br J Haematol. 2022 Feb 17. pp 1 – 3
177. Zhang X. et al. Treatment of Central Nervous System Relapse in Acute Promyelocytic Leukemia by Venetoclax: A Case Report. Front. Oncol., 05 July 2021, Volume 11, pp 1 5.
178. Gamis А, Alonzo Т, Meshinchi S, Sung L, Gerbing R, et al. Gemtuzumab Ozogamicin in Children and Adolescents With De NovoAcute Myeloid Leukemia Improves Event-Free Survival by Reducing Relapse Risk: Results From the Randomized Phase III Children’s Oncology Group Trial AAML0531. J Clin Oncol. 2014. 32 (27):3021-3032.
179. Haynes A. et al Time for a Change considering vancomycin alternatives for pediatric methicillin-resistant Staphylococcus aureus bacteremia. //JPIDS 2023: 12(5):308-318
180. McCall D. et al. Gilteritinib combination therapies in pediatric patients with FLT3-mutated acute myeloid leukemia //Blood Advances. – 2021. – Т. 5. – №. 23. – С. 5215-5219.
181. Selected schedules in the therapy of childhood cancers, 1st edition/ G. Henze, H. Weinberger; Baxter oncology Gmbh – Berlin, 2012. – 125 p. – ISBN 976-3-927105-97-3.
182. Диагностика и лечение острого миелоидного лейкоза у детей / И. И. Калинина, А. А. Масчан, Ю. В. Ольшанская [и др.] ; Организация-разработчик: ФГБУ НМИЦ Детской гематологии, онкологии и иммунологии им. Дмитрия Рогачева Министерства здравоохранения Российской Федерации. – Москва : Национальный медицинский исследовательский центр детской гематологии, онкологии и иммунологии им. Д. Рогачева, 2021. – 104 с. – ISBN 978-5-6047047-2-1. – EDN QTNIHQ.
183. Aplenc R, Alonzo TA, Gerbing RB, Lange BJ, Hurwitz CA, Wells RJ, Bernstein I, Buckley P, Krimmel K, Smith FO, Sievers EL, Arceci RJ; Children's Oncology Group. Safety and efficacy of gemtuzumab ozogamicin in combination with chemotherapy for pediatric acute myeloid leukemia: a report from the Children's Oncology Group. J Clin Oncol. 2008 May 10;26(14):2390-3295. doi: 10.1200/JCO.2007.13.0096. PMID: 18467731; PMCID: PMC4558626.
184. LeBlanc FR, Breese EH, Burns KC, Chang EK, Jones LM, Lee L, Mizukawa B, Norris RE, O'Brien MM, Phillips CL, Perentesis JP, Rubinstein J, Pommert L. Clinical outcomes of hypomethylating agents and venetoclax in newly diagnosed unfit and relapsed/refractory paediatric, adolescent and young adult acute myeloid leukaemia patients. Br J Haematol. 2024 Sep;205(3):1055-1066. doi: 10.1111/bjh.19679. Epub 2024 Jul 31. PMID: 39082439.
185. Badawi M, Gopalakrishnan S, Engelhardt B, Palenski T, Karol SE, Rubnitz JE, Menon R, Salem AH. Dosing of Venetoclax in Pediatric Patients with Relapsed Acute Myeloid Leukemia: Analysis of Developmental Pharmacokinetics and Exposure-Response Relationships. Clin Ther. 2024 O