Culligan PJ (2012) Nonsurgical management of pelvic organ prolapse. Obstet Gynecol 119:852-860.
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol. .
Doaee M. et al. Management of pelvic organ prolapse and quality of life: a systematic review and meta-analysis //International urogynecology journal. - 2014. - Т. 25. - №. 2. - С. 153-163. .
Maher C. et al. Surgical management of pelvic organ prolapse in women: a short version Cochrane review //Neurourology and Urodynamics: Official Journal of the International Continence Society. - 2008. - Т. 27. - №. 1. - С. 3-12. .
Ramage L. et al. Magnetic resonance defecography versus clinical examination and fluoroscopy: a systematic review and meta-analysis //Techniques in coloproctology. - 2017. - Т. 21. - №. 12. - С. 915-927. .
Bump R.C. Norton P.A. Epidemiology and natural history of pelvic floor dysfunction. Obstet Gynecol Clin North Am 1998;25(4):723-46. .
Lince S. L. et al. A systematic review of clinical studies on hereditary factors in pelvic organ prolapse
//International urogynecology journal. - 2012. - Т. 23. - №. 10. - С. 1327-1336. .
Feiner B, Fares F, Azam N, Auslender R, David M, Abramov Y (2009) Does COLIA1 SP1-binding site polymorphism predispose women to pelvic organ prolapse? Int Urogynecol J Pelvic Floor Dysfunct 20(9):1061-1065. .
Kluivers KB, Dijkstra JR, Hendriks JC, Lince SL, Vierhout ME, van Kempen LC (2009) COL3A1 2209G > A is a predictor of pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct 20(9):1113-1118. .
Zenebe C. B. et al. The effect of women"s body mass index on pelvic organ prolapse: a systematic review and meta analysis //Reproductive health. - 2021. - Т. 18. - №. 1. - С. 1-9. .
Madhu C. K., Hashim H. Surgery for pelvic organ prolapse //European Urology Supplements. - 2018. - Т. 17. - №. 3. - С. 119-125. .
Iglesia C., Smithling K. R. Pelvic organ prolapse //American family physician. - 2017. - Т. 96. - №. 3. - С. 179-185. .
Handa VL, Blomquist JL, Knoepp LR, Huskey KA, McDermott KC, Munoz A. Pelvic floor disorders 5- 10 years after vaginal or cesarean childbirth. Obstet Gynecol. 2011;118(4):777-784. .
Vergeldt TF, Weemhoff M, IntHout J, Kluivers KB. Risk factors for pelvic organ prolapse and its recurrence: a systematic review. Int Urogynecol J. 2105;26(11):1559-1573. .
Lin F. C. et al. Dynamic pelvic magnetic resonance imaging evaluation of pelvic organ prolapse compared to physical examination findings //Urology. - 2018. - Т. 119. - С. 49
Ward R. M. et al. Genetic epidemiology of pelvic organ prolapse: a systematic review //American journal of obstetrics and gynecology. - 2014. - Т. 211. - №. 4. - С. 326-335. .
КраснопольскииВ.И., Буянова С.Н., Петрова В.Д. Комбинированное лечение больных с опущением и выпадением внутренних половых органов и недер- жанием мочи с применением антистрессовых технологии" Пособие Для вра- чеИ. - М., 2003. - 41 с. .
Garshasbi A., Faghih-Zadeh S., Falah N. The status of pelvic supporting organs in a population of iranian women 18-68 years of age and possible related factors. Arch Iran Med 2006;9(2):124-8. .
Nygaard I., Barber M.D., Burgio K.L. Prevalence of symptomatic pelvic floor disorders in US women. JAMA 2008;300(11):1311-6. .
Кулаков В.И., Чернуха Е.А., Гус А.И. и др. Оценка состояния тазового дна после родов через естественные родовые пути. - Акушерство и гинекология. - 2004. - С. 26-30. .
Hendrix S.L., Clark A., Nygaard I. et al. Pelvic organ prolapse in the Women»s Health Initiative: gravity and gravidity. Am J Obstet Gynecol 2002;186(6):1160-6. .
Thakar R., Stanton S. Management of genital prolapse. BMJ 2002;324(7348): 1258-62. .
Samuelsson E.C., Victor F.T., Tibblin G., Svardsudd K.F. Signs of genital prolapse in a Swedish population of women 20 to 59 years of age and possible related factors. Am J Obstet Gynecol 1999;180(2):299-305. .
Горбенко О. Ю. и др. Этиология, патогенез, классификация, диагностика и хирургическое лечение опущения внутренних половых органов //Вопросы гинекологии, акушерства и перинатологии. - 2008. - Т. 7. - №. 6. - С. 68-78. .
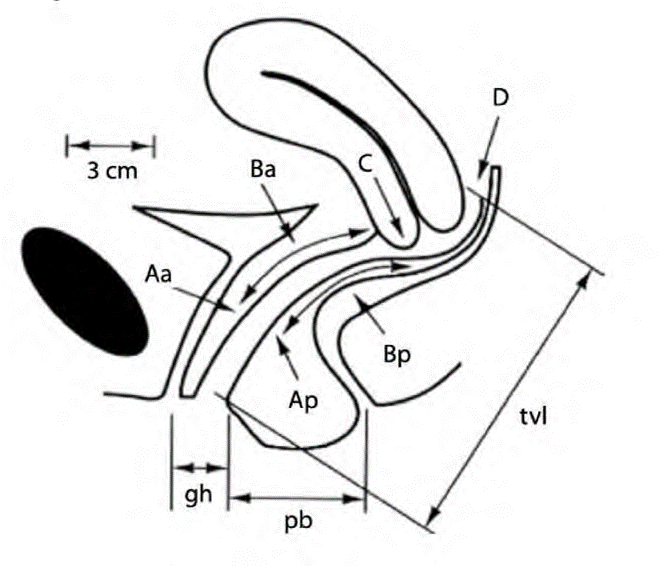
Madhu C. et al. How to use the pelvic organ prolapse quantification (POP-Q) system? //Neurourology and urodynamics. - 2018. - Т. 37. - №. S6. - С. S39-S43. .
Bump R.C., Mattiasson A., Bo K. et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 1996; 175(1):10-7. .
American College of Obstetricians and Gynecologists et al. Pelvic organ prolapse //Female Pelvic Medicine & Reconstructive Surgery. - 2019. - Т. 25. - №. 6. - С. 397408. .
Veit-Rubin N. et al. Association between joint hypermobility and pelvic organ prolapse in women: a systematic review and meta-analysis //International urogynecology journal. - 2016. - Т. 27. - №. 10. - С. 1469-1478. .
Digesu G.A., Chaliha C., Salvatore S. The relationship of vaginal prolapse severity to symptoms and quality of life. BJOG 2005;112(7):971-6. .
Swift S.E., Tate S.B., Nicholas J. Correlation of symptoms with degree of pelvic organ support in a general population of women: what is pelvic organ prolapse? Am J Obstet Gynecol 2003;189:372-7.
Гвоздев М. Ю., Тупикина Н.В., Касян Г.Р., Пушкарь Д.Ю. Пролапс тазовых органов в клинической практике врача-уролога: методические рекомендации № 3 //Методические рекомендации. - 2016. - №. 3. - С. 58. .
Буянова С.Н., Титченко Л.И., Яковлева Н.И. и Др. ФенотипическиИкомплекс Дисплазии соеДинительнои ткани у женщин. Клиническая меДицина 2003;8:42-8. .
Dietz H. P. et al. Pelvic organ descent in young nulligravid women //American journal of obstetrics and gynecology. - 2004. - Т. 191. - №. 1. - С. 95-99. .
Abrams P, Andersson KE, Birder L, et al. Fourth International Consultation on Incontinence recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurouro. .
Савельева Г. М. и Др. Национальное руковоДство //Акушерство-М.: Гэотар-МеДиа. - 2015. .
Dietz H. P. Ultrasound in the assessment of pelvic organ prolapse //Best Practice & Research Clinical Obstetrics & Gynaecology. - 2019. - Т. 54. - С. 12-30. .
Orno A. K., Dietz H. P. Levator co-activation is a significant confounder of pelvic organ descent on Valsalva maneuver //Ultrasound in Obstetrics and Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology. .
Amir B. et al. SOGC Committee opinion on urodynamics testing //Journal of Obstetrics and Gynaecology Canada. - 2008. - Т. 30. - №. 8. - С. 717-721. .
Collins C.W., Winters J.C. AUA/SUFU adult urodynamics guideline: a clinical review. Urol Clin North Am 2014;41(3):353-62. .
Ghoniem G.M., Walters F., Lewis V. The value of the vaginal pack test in large cystoceles. J Urol 1994;152:931.
Marinkovic S.P., Stanton S.L. Incontinence and voiding difficulties associated with prolapse. J Urol 2004;171:1021-8. .
Versi E., Lyell D.J., Griffiths D.J. Videourodynamic diagnosis of occult genuine stress incontinence in patients with anterior vaginal wall relaxation. J Soc Gynecol Investig 1998;5:327-30. .
Li C., Gong Y., Wang B. The efficacy of pelvic floor muscle training for pelvic organ prolapse: a systematic review and meta-analysis //International urogynecology journal. - 2016. - Т. 27. - №. 7. - С. 981-992. .
NICE Guidance - Urinary incontinence and pelvic organ prolapse in women: management: © NICE (2019) Urinary incontinence and pelvic organ prolapse in women: management. BJU Int. 2019 May;123(5):777-803. doi: 10.1111/bju.14763. PMID: 31008559. .
Giri A. et al. Obesity and pelvic organ prolapse: a systematic review and meta-analysis of observational studies //American journal of obstetrics and gynecology. - 2017. - Т. 217. - №. 1. - С. 11-26. .
L. Cardozo, G. Bachmann, D. McClish, D. Fonda, and L. Birgerson, “Meta-analysis of estrogen therapy in the management of urogenital atrophy in postmenopausal women: second report of the Hormones and Urogenital Therapy Committee.,” Obstet. Gynecol., vol. 92, no. 4 Pt 2, pp. 722-727, Oct. 1998, doi: 10.1016/s0029-7844(98)00175-6.
C. Rueda, A. M. Osorio, A. C. Avellaneda, C. E. Pinzon, and O. I. Restrepo, “The efficacy and safety of estriol to treat vulvovaginal atrophy in postmenopausal women: a systematic literature review.,” Climacteric, vol. 20, no. 4, pp. 321-330, Aug. 2017, doi: 10.1080/13697137.2017.1329291.
Y. S. V. Yureneva, E. E. I. Ermakova, and G. A. V. Glazunova, “Genitourinary syndrome of menopause in peri- and postmenopausal patients: Diagnosis and therapy (short clinical guideline),” Akush. Ginekol. (Sofiia)., vol. 5_2016, pp. 138-144, May 2016, doi: 10.18565/aig.2016.5.138-144.
Hagen S, Stark D. Conservative prevention and management of pelvic organ prolapse in women [systematic review]. Cochrane Database of Systematic Reviews 2011; issue 12, art. no.: CD003882. .
Braekken IH, Majida M, Engh ME, et al. Can pelvic floor muscle training reverse pelvic organ prolapse and reduce prolapse symptoms? An assessor-blinded, randomized, controlled trial. Am J Obstet Gynecol 2010;203:170.e1-170. .
Dumoulin C, Hay-Smith EJ, Mac Habee-Seguin G. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2014;(5): CD005654. .
Huang YC, Chang KV. Kegel Exercises. 2020 May 29. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan. .
Park SH, Kang CB, Jang SY, Kim BY. [Effect of Kegel exercise to prevent urinary and fecal incontinence in antenatal and postnatal women: systematic review]. J Korean Acad Nurs. 2013 Jun;43(3):420-30. .
Hagen S., Stark D. Conservative prevention and management of pelvic organ prolapse in women. Cochrane Database Syst Rev 2011;(12):CD003882. .
Vizintin Z, Lukac M, Kazic M, Tettamanti M. Erbium laser in gynecology. Climacteric. 2015;18 Suppl 1:4-8. .
Arias BE, Ridgeway B, Barber MD. Complications of neglected vaginal pessaries: case presentation and literature review. Int Urogynecol J Pelvic Floor Dysfunct 2008;19:1173-1178. .
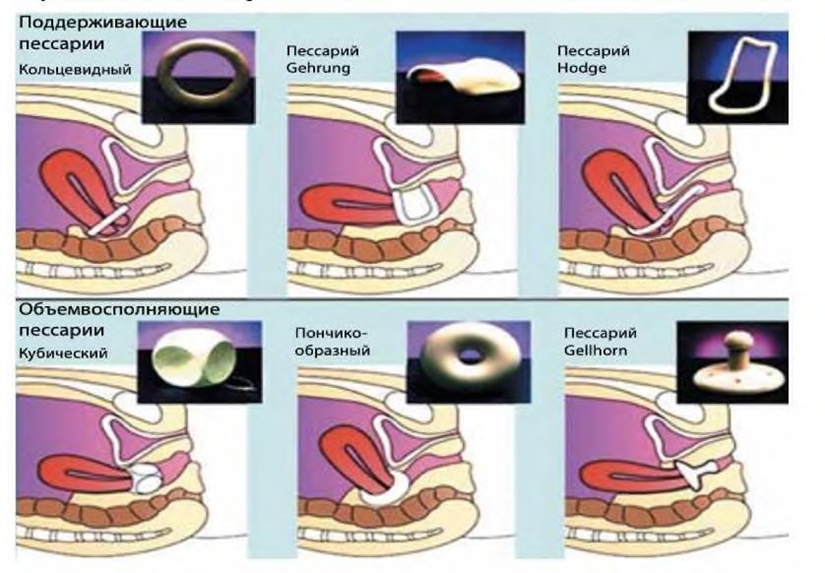
Robert M, Schulz JA, Harvey MA, et al. Urogynaecology Committee. Technical update on pessary use. J Obstet Gynaecol Can 2013;35:664-674. .
Clemons JL, Aguilar VC, Tillinghast TA, et al. Patient satisfaction and changes in prolapse and urinary symptoms in women who were fitted successfully with a pessary for pelvic organ prolapse. Am J Obstet Gynecol 2004;190:1025-1029. .
Cundiff GW, Amundsen CL, Bent AE, et al. The PESSRI study: symptom relief outcomes of a randomized crossover trial of the ring and Gellhorn pessaries. Am J Obstet Gynecol 2007;196:405.e1-405.e8. .
Pott-Grinstein E., Newcomer J.R. Gynecolgist»s patterns of prescribing pessaries. J Reprod Med 2001;46:205-8. .
A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Am J Obstet Gynecol 2000;183:1365-1373 discussion 1373-1374. .
Paraiso MF, Barber MD, Muir TW, et al. Rectocele repair: a randomized trial of three surgical techniques including graft augmentation. Am J Obstet Gynecol 2006;195:1762- 1771. .
Cundiff GW, Weidner AC, Visco AG, et al. An anatomic and functional assessment of the discrete defect rectocele repair. Am J Obstet Gynecol 1998;179:1451-1456 discussion 1456-1457. .
Chen L, Ashton-Miller JA, Hsu Y, et al. Interaction among apical support, levator ani impairment, and anterior vaginal wall prolapse. Obstet Gynecol 2006;108:324-332. .
Chmielewski L, Walters MD, Weber AM, et al. Reanalysis of a randomized trial of 3 techniques of anterior colporrhaphy using clinically relevant definitions of success. Am J Obstet Gynecol 2011;205(69):e1-e8. .
Sung VW, Rardin CR, Raker CA, et al. Porcine subintestinal submucosal graft augmentation for rectocele repair: a randomized controlled trial. Obstet Gynecol 2012;119:125-133. .
Mangir N, Roman S, Chapple CR, MacNeil S. Complications related to use of mesh implants in surgical treatment of stress urinary incontinence and pelvic organ prolapse: infection or inflammation? World J Urol. 2020. .
Karram M, Maher C. Surgery for posterior vaginal wall prolapse. Int Urogynecol J 2013;24:1835- 1841. .
Maher C, Feiner B, Baessler K, et al. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database Syst Rev 2016; issue 2, art. no.: CD012079. .
Barber MD, Brubaker L, Burgio KL, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Pelvic Floor Disorders Network. Comparison of 2 transvaginal surgical approaches and perioperative behavioral therapy for apical vagin. .
Johnson N. et al. Methods of hysterectomy: systematic review and meta-analysis of randomised controlled trials //Bmj. - 2005. - Т. 330. - №. 7506. - С. 1478. .
Serati M. et al. Robot-assisted sacrocolpopexy for pelvic organ prolapse: a systematic review and meta-analysis of comparative studies //European urology. - 2014. - Т. 66. - №. 2. - С. 303-318. .
Petri E, Ashok K. Sacrospinous vaginal fixation—current status. Acta Obstet Gynecol Scand 2011;90:429-436. .
Siddiqui NY, Grimes CL, Casiano ER, et al. Society of Gynecologic Surgeons Systematic Review Group. Mesh sacrocolpopexy compared with native tissue vaginal repair: a systematic review and meta-analysis [systematic review]. Obstet Gynecol 2015;125:44-55.
Hudson CO, Northington GM, Lyles RH, et al. Outcomes of robotic sacrocolpopexy: a systematic review and meta-analysis. Female Pelvic Med Reconstr Surg 2014;20:252-260 (Systematic review). .
Brubaker L, Cundiff G, Fine P, et al. A randomized trial of colpopexy and urinary reduction efforts (CARE): design and methods. Control Clin Trials 2003;24:629-642. .
Barber MD, Brubaker L, Menefee S, et al. Operations and pelvic muscle training in the management of apical support loss (OPTIMAL) trial: design and methods. Contemp Clin Trials 2009;30:178-189.
“Maher, C., et al. Laparoscopic colposuspension or tension-free vaginal tape for recurrent stress urinary incontinence and/or urethral sphincter deficiency-a randomised controlled trial. Neurourol Urodyn., 2004. 23: 433.”
“Baessler K. et al. Surgery for women with pelvic organ prolapse with or without stress urinary incontinence //Cochrane Database of Systematic Reviews. - 2018. - №. 8.”
“Maher, C., et al. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev, 2013: CD004014. https://www.ncbi.nlm.nih.gov/pubmed/23633316.”
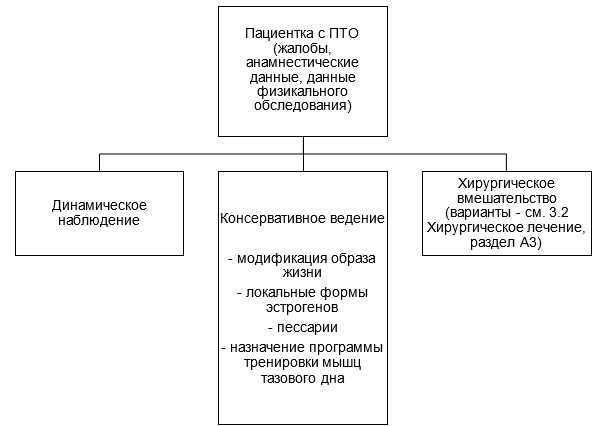
Pizzoferrato A. C. et al. Management of female pelvic organ prolapse—Summary of the 2021 HAS guidelines //Journal of Gynecology Obstetrics and Human Reproduction. – 2023